INTRODUCTION
As the saying goes, “an ounce of prevention is worth a pound of cure.” Indeed, it has long been the goal of rehabilitation professionals to develop effective injury prevention programs for athletes due to high injury rates. In the United States, competitive and recreational athletes reported 8.6 million injuries annually with up to 42% of them involving the lower extremity.1 One common non-contact lower extremity injury, anterior cruciate ligament (ACL) rupture, is often the target of prevention programs. However, these prevention programs have room for further improvement. For example, Noyes & Barber-Westin2 found that to prevent one non-contact ACL rupture, 70 athletes need to participate in the prevention program. These current programs largely target improving the physical and biomechanical aspects of movement related to injury prevention. One possible missing component is the contribution of cognitive impairment on injury risk.
Participation in sport requires the integration of many different inputs to successfully accomplish a task. Athletes must sort through high amounts of sensory information, while avoiding or challenging an opponent, and attempting to achieve the goal (e.g., score or prevent the score). A possibility of increased injury risk exists where participants respond to unanticipated events or undertake rapid visual-motor decision making - such is the case during athletic participation.3 Indeed, cognitive integration clearly plays a role in task achievement during sport. The idea that the addition of cognitive load could result in riskier biomechanics during a relatively simple physical task relates to a concept known as the “capacity model of attention”.4 The cognitive process of attention is considered the bottleneck of information processing, creating a natural limit to an individual’s capacity to perform mental and motor tasks,5 and different activities impose different demands on this limited capacity.6 Thus, lower attentional and/or cognitive reserves due to innate natural abilities, previous head injuries, or task load, may leave athletes at a higher risk for non-contact injuries. Widening clinical attention from simply a physical, biomechanical approach to more of a holistic viewpoint could boost the effectiveness of injury prevention programs, at least for some athletes.
To fully understand the effects of cognitive function on lower extremity non-contact injury risk, it is important to define cognition and its relation to kinetics and kinematics. According to Herman and Barth,7 ‘cognition’ is a process related to the abilities of the cortical and subcortical brain systems to function. It includes some aspects not considered related to non-contact injury risk such as language, intelligence, and social functioning. Other aspects of cognition such as visual attention, self-monitoring, agility, fine motor performance, processing speed and reaction time may hold importance when it comes to injury risk in sports.7 For the purposes of the present work, the definition of cognition will include processes related to the abilities of the cortical brain systems including visual attention, fine motor performance, processing speed and reaction time. A rich collection of literature exists comparing the above listed domains of cognition and lower extremity injury risk, and these domains are easily measured using standardized approaches, simplifying comparisons across studies.
Cognitive prowess can depend on natural abilities, history of neurologic trauma or the mental load of a task. Researchers, in particular over the last two decades, have investigated the effect of natural cognitive ability on performance of motor tasks7 or direct injury rates.8,9 Even more recently, connections between athletes who have suffered a concussion and injury rates have been studied.10,11 The history of concussion can be considered a modification of cognitive ability and thus that body of literature has been included in the present scoping review. Other researchers have increased the cognitive load of common biomechanical tasks by adding a cognitive component to motor tasks to assess the effects on mechanics in healthy athletes.4,12
However, rehabilitation professionals likely lack full comprehension regarding the extent of the connection between cognitive function and non-contact injury risk across this broad literature. Better understanding of the underlying mechanisms responsible for non-contact lower extremity injury can help to determine specific cognitive and neuromuscular activities that facilitate lower extremity injury prevention and/or recovery. The purpose of this scoping review was to examine the existing literature to determine the extent to which cognitive function (both cognitive ability and task cognitive load) influences non-contact lower extremity injury risk in male and female athletes with a broad variety of athletic expertise.
METHODS
Literature Search Strategy
Search terms included Boolean combinations of “cognition”, “concussion”, “ImPACT”, “cognitive deficit”, “mild traumatic brain injury (mTBI)” and “neuropsychological function” as cognitive descriptors. The terms “injury risk” and “lower extremity injury” as injury terms (Appendix 1). The following electronic databases were searched: CINAHL, SPORTDiscus, Google Scholar, and MEDLINE with the most recent search conducted in August 2021.
Study Selection Criteria
Inclusion criteria consisted of English-language studies with a publication range from 2000-2021. Exclusion criteria consisted of neurological and cognitively atypical populations including diagnoses such as Attention Deficit Hyperactivity Disorder (ADHD), traumatic brain injury (TBI), cerebral palsy (CP), multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS) and Autism Spectrum Disorder. One notable exception was the inclusion of concussion as a diagnostic category for this scoping review. Concussion (AKA mild traumatic brain injury or mTBI) is a unique example of potentially impaired cognitive capacity that potentially could increase LE non-contact injury risk. Articles that fell into this category were analyzed separately from all other articles.
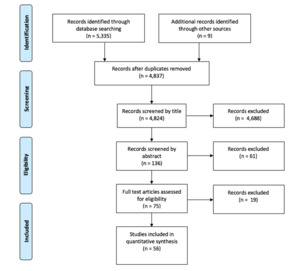
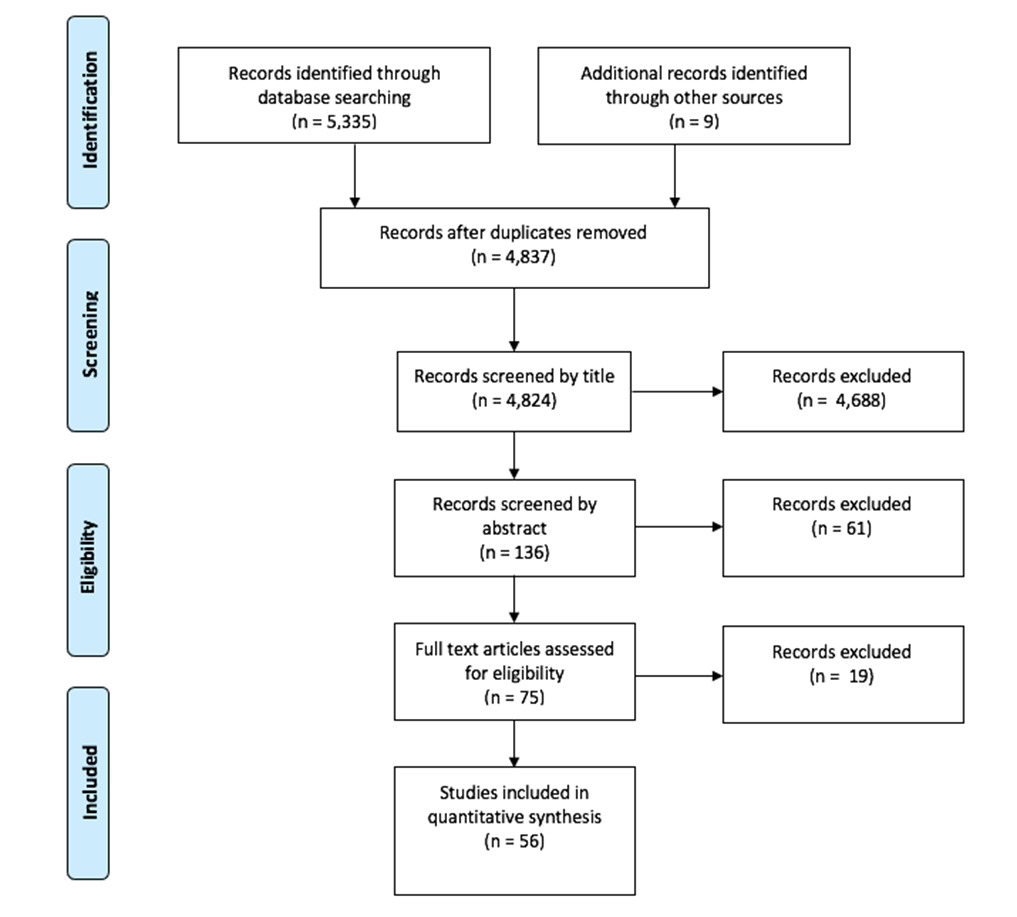
Using the article selection strategy suggested by Smith,13 the initial search yielded 5,335 results (Figure 1). After removing duplicates, 4,824 studies remained. Authors divided the 4,824 articles among themselves and individually assessed whether they met the inclusion criteria or violated the exclusion criteria. Articles that did not clearly meet the inclusion criteria were discussed by the entire group and a determination made by consensus. Studies not meeting the inclusion criteria or violating the exclusion criteria were removed; first by article title (4,688 articles), next by abstract (61 articles) and finally by full text content (19 articles). These articles were removed during full-text screening because they did not satisfy the purpose of this study. Following full-text screening, article references were reviewed for additional content that met the inclusion criteria (nine articles). Finally, 56 articles were included for review (Figure 1).
Data Synthesis
Data from each article including experimental design, sample size, participants, task, dependent measures, and results/conclusions were extracted (Appendix 2). Fifty-six articles were classified into five categories based on participant demographics and dependent measures: natural cognitive ability in a healthy population, performance during dual-task paradigms in healthy populations, performance during dual-task paradigms in participants with a history of concussion, LE injury risk in participants with a history of concussion, and lastly, cognitive testing performance in participants with a history of concussion.
Methodological risk of bias was assessed using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies from the National Institutes of Health,14 which includes 14 items. While not all articles fell in the observational and cohort and cross-sectional study categories (see Table 1), the authors chose to use a single quality assessment tool for consistency across all included articles. Each publication was given an overall score of ‘good’, ‘fair’, or ‘poor’ (Table 1) based on this tool. Initial scoring was performed by a single author (MR, MP, TW or DL), then the first four authors (MR, MP, TW and DL) discussed all included papers and reached consensus on scoring.
RESULTS
Risk of Bias
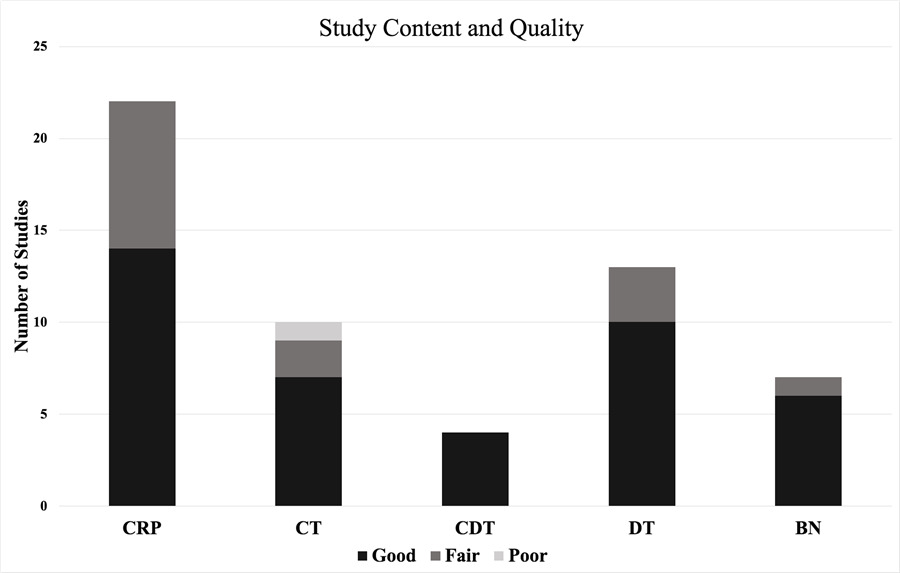
Discussion and strict adherence to the quality appraisal tool was utilized to come to consensus for all included studies. Forty-one out of the fifty-six articles had strong methodological quality, while fourteen articles had fair methodological quality, and one article had poor quality (Figure 2). Common reasons for articles not having strong methodological quality included: small sample size (based on a lack of a sample size justification, power description, or variance / effect size data), insufficient time between exposure and outcome (determined on a case-by-case basis for each paper), and lack of blinding to participants and researchers.
Methodological Design
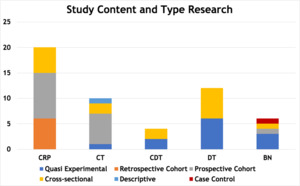
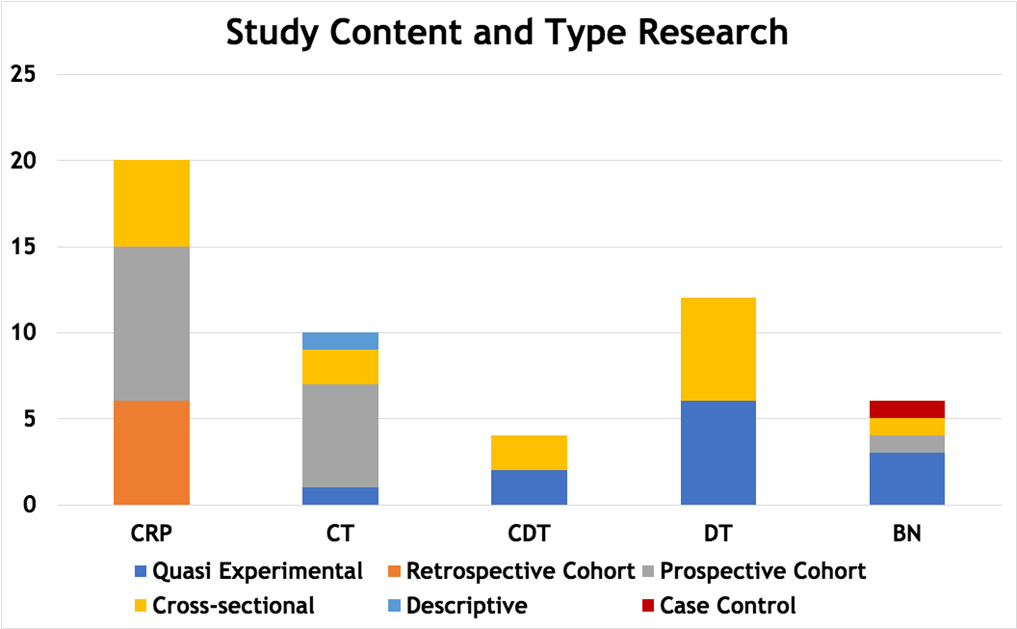
Methodological design of the included papers determines the level of evidence for this scoping review. Figure 3 illustrates the number of articles by topical category and experimental approach (Refer to Table 1 for the specific articles that fell into each category). Sixteen studies utilized a prospective cohort design. Twelve studies were retrospective cohort design. Ten studies were prospective quasi-experimental design. Twelve studies used a prospective cross-sectional design. Five studies used retrospective cross-sectional design. One study used a retrospective case control design. The specific demographic data, methods and conclusions for each study are provided in Appendix 2.
The effect of cognitive ability on lower extremity movement in healthy athletes
Baseline Cognitive ability. Seven articles examined athletes’ natural cognitive function and its relationship to task performance and injury risk.7–9,12,15–17 These studies investigated the relationship of a person’s baseline cognition, as defined by each researcher, to injury risk. Six of the seven articles found athletes with lower baseline cognitive function had significantly altered mechanics.7–9,12,16,17
Four studies utilized the IMmediate Post-concussion Assessment and Cognitive Testing (ImPACT) scores to relate cognitive function and injury risk.8,9,12,15 As the name suggests, the ImPACT is a measurement tool designed to assist with return-to-play decisions post-concussion.18 Since it gives such a broad cognitive screen, the use of the ImPACT to identify post-concussion cognitive deficits is debated in literature. The test consists of six neuropsychological tests designed to target different aspects of cognitive functioning including attention, memory, processing speed and reaction time. From these six tests, four composite scores are generated including verbal memory, visual memory, visuomotor speed and reaction time. Although this test was designed for concussion management, the domains of the ImPACT may also prove useful as a measurement of baseline cognition. Three studies found a positive relationship between cognitive function and LE injury risk with lower ImPACT score.8,9,12 These studies varied significantly in participant populations including male football players at one university,9 recreational female college athletes12 and male and female athletes at different universities.8 The study that reported null differences between groups studied 14-17 year old ski and snowboard athletes.15
The robustness of findings across participant groups matched the variety of dependent measures included in these studies. Slower reaction times on the ImPACT test correlated with increased vertical ground reaction force with unanticipated jumping conditions12 and an increased likelihood of lower extremity injury during one football season.9 Other factors of the ImPACT test including of verbal memory, visual memory and processing speed were worse in participants who sustained a non-contact ACL injury.8 Out of the studies looking at ImPACT scores and baseline cognitive function, one study did not find significant differences on pre-season ImPACT testing for the injured group and non-injured group.15 This study may have a different result due to the ages of participants being younger (14-17 v. 18-24 year-olds) or the difference in the environmental demands of downhill skiing (snow conditions may have led to a non-impact ACL injury versus football and unanticipated jumping with relatively stable playing surfaces).
Three studies utilized other methods to define baseline cognitive function. One study utilized the Concussion Resolution Index (CRI) which examines memory, reaction time, speed of decision making, and speed of information processing in a computer test like ImPACT.7 Herman and Barth found that low performers had increased peak anterior tibial shear force, knee abduction moment, knee abduction angle, and decreased trunk flexion angle on a drop-landing task,7 often considered mechanics that lead to ACL rupture.
Another tool used to measure cognitive function is the CNS Vital Signs computer-based cognitive tests. A group with chronic ankle instability had significantly lower composite memory, visual memory, and simple attention compared to the control group.17 Finally, female jumping and cutting athletes with a lower score on the Symbol Digit Modalities Test had significantly increased quadriceps activity before and after ground contact and decreased co-contraction ratio only after ground contact with unanticipated cutting tasks and single leg landing.16 Together, these results indicate that across sports (note the exception of skiing / snowboarding15) measures of cognition and measures of kinetics / kinematics, a negative relationship exists with poorer biomechanical performance and/or increased injury rates in athletes with lower baseline cognitive performance.
The effect of cognitive load on lower extremity movement in healthy athletes
Dual Task Activities. While one approach to determine the role of cognitive ability on lower extremity injury risk is to measure natural baseline function, it may not consider the additional resources needed in game time situations. Another approach is to add a second cognitive operation in addition to performing a motor task. The use of single motor tasks to assess athletic performance, such as a drop vertical jump, balance measures, and reaction time have not been specific enough to determine which athletes would ultimately sustain a lower extremity injury.19 Single motor tasks may not be challenging enough from a cognitive perspective and do not replicate the full demands of sport participation. Dual task paradigms explore the impact on performance when a cognitive task, such as trail making, serial 7’s, word spelling, or reciting months in reverse order, is combined with a physical task, such as maintaining postural stability during perturbations, walking, balancing, or cutting activities. The addition of a cognitive demand, and thus the utilization of dual-task paradigms, has shown increases in the incidence of more risky lower extremity mechanics.20 The decrease in cognitive or physical performance during dual task paradigms compared to performance during single physical tasks is termed dual-task cost.21
Ten articles in this category utilized jump landing tasks to examine participants’ ability to maintain controlled lower extremity mechanics to decrease injury risk.4,12,19,20,22–27 Five utilized a similar method of introducing cognitive demand, including counting, math, memorization, and visual distractions,4,23–25,27 while the other five articles12,19,20,22,26 used decision-making and sport activities (cutting, passing, overhead goal, dribbling a soccer ball) to increase cognitive demand. In all cases, the ten studies demonstrated that when a second simultaneous task was added, lower extremity mechanics changed including increased number of failed trials,4,19 decreased overall jump height,4,23 higher peak vertical ground reaction force,12,24,28 decreased knee flexion,12,22,28 decreased postural stability,25 and increased knee valgus.22,26 These altered lower extremity mechanics are classified as “risky” mechanics leading to increased lower extremity injury risk.
Three included articles took a different approach to quantify athlete’s ability to maintain safe mechanics during activities other than jump landings, such as balance assessments29,30 and repeated hop tests.31 These three articles introduced additional cognitive demand through the use of more reactive tasks such as the Auditory Procedural Reaction Time (APRT) test and the Procedural Reaction Time Throughput (PRTT) test,29 modified Stroop test and the Brooks Spatial Memory Test,30 and reaction to color identifying initiation of hopping task.31 The APRT and PRTT increase cognitive demand through the participant reacting to auditory (APRT) or visual (PRTT) stimuli to assess reaction time. The Stroop test increases cognitive demand through higher level processing to report the color of the work presented which is typically also a color (the word ‘red’ presented in blue font). The Brooks Spatial Memory Test involves a person describing a set of numbers on a grid to a participant and the participant must then report the order of the numbers on a grid from memory, increasing cognitive load during other tasks. Under dual task conditions, reaction time decreased,29,31 mechanics were modified to maintain stability,29,30 and athletes had more difficulty maintaining balance control,30 potentially leading to increased injury risk compared to single task conditions.
The effect of cognitive ability and cognitive load on lower extremity movement in concussed athletes
In recent years, a considerable number of studies have addressed the impact of a concussive event on lower extremity injury risk and the presence of altered lower extremity mechanics post-concussion. These authors focused on the effect of concussion itself on injury risk. A slightly different perspective on this patient population can be taken. Rather than focusing on the diagnosis of concussion, these studies were included as concussions lead to short-term cognitive deficits32,33 and potentially represent lower cognitive ability. However, due to the transient nature and significant variability of concussive effects,34,35 the results of these articles were summarized separately from the other categories.
Concussion and Dual Task Performance. Four articles21,36–38 examined the effect a positive history for concussion on participant performance during dual task paradigms. These studies included division I collegiate athletes21,36 and recreational athletes.37,38 Cognitive tasks included the Standard Assessment of Concussion (SAC) test, Trail Making A and B, processing speed tasks, spelling five letter words backwards, subtracting by serial 7s from a randomly presented 2-digit number, and reciting the months of the year in reverse order. Participants performed these cognitive tasks while maintaining postural stability, performing an 8- or 10-meter walk test and performing tandem gait tests, functional movement tasks such as jump landing tasks and cutting tasks.39 Three studies21,37,39 explored the dual task cost when cognitive assessment tasks were performed simultaneously during gait tasks while one study examined dual task during quiet stance.36 All four papers found a decreased level of performance in the recently concussed cohort compared to healthy controls.21,36,37,39 Participants with a recent concussion not only reported more symptoms, but also walked significantly slower during dual task conditions and responded with slower simple reaction times. Although the differences were less significant during functional tasks, the control group displayed better reaction time than the concussed group during the anticipated cutting and the concussed group displayed greater trunk flexion while cutting.39 Recently concussed athletes exhibited less postural stability compared to healthy controls, even when tested 6-weeks post-concussion and beyond the resolution of symptoms.36
Concussion and Risk Prediction. Twenty-two articles10,11,36,38,40–57 examined the influence of concussion on lower extremity injury rates. Researchers across these studies examined participant data longitudinally and included a wide variety of participant characteristics: both male and female participants, recreational, university, and professional athletes, soldiers, high school-aged athletes, retired professional athletes, participants from multiple countries, and participants across many sport activities. All twenty-two studies reported an increased risk of lower extremity injury after experiencing one or more concussive events. A history of concussion can increase the risk of sustaining a lower extremity injury between 1.60 times42 to 7.37 times.40 Injury rates remained increased far beyond the resolution of symptoms and even remained increased following an appropriate return to play (RTP) protocol. A 38% greater risk of lower extremity injury up to two years post-concussion has been reported.47 Time to lower extremity injury after RTP, was significantly shorter in concussion groups than in control groups.36,52 Lastly, multiple concussions were often associated with higher incidence or greater odds of sustaining a lower extremity injury,38,45,48,51,52 with one study reporting a 34% increase in odds of sustaining a lower extremity injury for every previous concussive event.38
Concussion and Baseline Testing. Ten papers58–67 examined the effect that a history of concussion has on motor performance. Tests in this category included rapid alternating movement,58 the Bruininks-Oseretski Test of Motor Proficiency (BOTMP),61,62 the modified Romberg test on foam,65 the Balance Error Scoring System (BESS), the Y-balance test,63,64,67 balance tasks66 and the functional movement screen (FMS).59,67 Participants varied in age range and participation level, including children aged 7-16 years old,61,62 high school athletes,65,66 recreationally active college students,59,66 and Division I collegiate athletes.58,63,64,67
Five of the ten articles reported significant test performance deficits by participants who had a history of at least one concussive event. Performance test deficits included greater inhibition of the primary motor cortex during a balance task,58 altered lower extremity stiffness during landing,60 decreased performance on the BOTMP,61,62 and increased errors on the BESS test.67 The remaining five articles did not find statistically significant differences between concussed and non-concussed groups when examining performance during testing.
DISCUSSION
Cognition most likely contributes to lower extremity injuries when the system is taxed beyond capacity. Exceeding cognitive limits can occur either due to limited cognitive ability or to increased task demands. Articles addressing both components of cognitive function (ability and demand) were included in this scoping review to assess the robustness of any cognitive contributions to LE injury risk. No constraints were placed on sport, gender or experience level for the same reason. Additionally, studies that directly measured both the predictive ability of cognitive function on lower extremity rates and ones measuring biomechanical factors known to lead to ACL injury were included to cast a wide net. Consistent across participant demographics, tasks, and dependent measures, fifty-one of fifty-six assessed articles concluded that decreased cognitive ability or increased cognitive load led to risky LE mechanics or a direct increase in non-contact LE injury risk. The six studies that did not support the previous statement had some commonalities: four of six had fair or poor methodological quality and five of six fell under the concussion and baseline testing category. Limitations of these latter five articles included: investigating sub-concussive events,64 fair methodological quality,63,65 poor methodological quality due to non-matched cohorts,64 club level athletes as participants,59 and small sample size.64
The results from the 51 papers provide some insight on how clinicians might further consider how to optimize current injury prevention and return-to-sport protocols. A cognitive component contributing to decreased reaction time, decreased attentional resources, and altered LE mechanics leading to increased risk of non-contact injury has largely been ignored in both research and clinical practice settings. Dual task conditions, which are common in sport, challenge cognitive reserve which then results in decreased physical and cognitive performance during biomechanical tasks in both healthy and previously concussed populations.21 Further research is needed to evaluate the effectiveness of novel prevention and intervention programs that address cognitive functional deficits in addition to biomechanical considerations. Future studies should include methods to quantify the risk associated with altered cognitive function.
Limitations
In such a broad, scoping review, decisions for article inclusion to increase the robustness of the findings also created some limitations. The intent of the present study to uncover cognitive contributions to lower extremity non-contact injury risk led to casting a wide net by including athletes with impaired cognitive function (concussion), athletes with a natural variance in typical cognitive function and also athletes undergoing tasks with higher cognitive load (dual-task paradigms). Cognition is impacted both by an individual’s cognitive capacity and the cognitive demands of a task. In sport, the cognitive demands are typically high in sports where most non-contact ACL injuries occur (e.g., soccer, basketball). Add to that diminished cognitive ability, either through a natural baseline or through brain injury, an athlete might be at higher risk of injury. It is explicitly for this reason, populations with differences in cognitive ability and populations undergoing tasks with higher cognitive loads were included to determine if both cognitive ability and cognitive demands had a similar impact on injury risk. Far more research exists on the effect of concussion on injury risk than typical baseline function, so this population was included in the present scoping review. These cases of concussion were intentionally evaluated separately in case the results deviated from healthy individuals, which ended up not being the case.
Attempting to define cognitive ability (whether natural variance or after brain injury) is difficult. In this manuscript, the definition provided by Herman and Barth7 was used, which includes multiple domains presumed not to affect motor function (social interactions, intelligence) and others that do (reaction time, attention, working memory). The findings of this manuscript do not allow the reader to identify the specific cognitive domains most critical for efficient lower extremity function. Future work is needed to pinpoint domains most ripe for intervention to prevent injury.
Studies investigating actual risk (AKA reporting injury rates in sub-populations) and studies measuring lower extremity mechanics thought to lead to non-contact ACL injury were included in the present scoping review. It is important to distinguish between the two. Research evaluating actual risk were confined to the categories of baseline cognitive function and athletes who have experienced concussion, whereas at least one paper in each category included in this scoping review evaluated changes in lower extremity mechanics based on cognition (either cognitive capacity or task cognitive load). Caution must be taken in the interpretation of changes in mechanics as it may not directly lead to injury.
Although 56 articles were included in the present scoping review, not enough articles existed to allow any conclusions to be made specific to gender, age, or level of sport. Interestingly, in spite of the significant variation in researched sport, level of competition and gender, the results were surprisingly consistent that cognition did appear to play a factor. An interesting line of future research would be to explore any one of these categories relative to cognition and injury risk.
Some may consider another limitation of the present scoping review is that of including eleven doctoral dissertations, although others would not. While these documents would have not gone through blinded peer-review, they would have been extensively reviewed by a dissertation committee that would presumably consist of experts in the research area. The methods of the dissertations were reviewed in the same manner as the published articles to ensure methodological quality using the NIH checklist. None of them exhibited poor or fair quality.
Overall, the literature is dominated by concussion studies, and more research needs to focus on cognitively typical populations. Of the studies that do study cognitive function and dual tasks, large variability exists in the objective measures used to demonstrate decreased cognitive function, allowing for limited capability in comparing measures among studies. Future research will need to determine cut-off scores for cognitive tests and dual task performance tests to better define what constitutes an at-risk athlete based on cognitive performance.
Clinical Implications
Determining the impact of cognitive function on non-contact LE injury will guide rehabilitation professionals to develop innovative, evidence-based prevention strategies to decrease risk of non-contact LE injury in a wide variety of populations that may have a cognitive component to injury risk. Training cognitive factors may serve as the missing link in highly effective and robust injury prevention programs and warrants further study.
CONCLUSIONS
Results of this scoping review demonstrate decreased cognitive function and increased cognitive load related to task demands are associated with increased lower extremity injury risk via decreased attentional resources, slowed reaction time, and altered LE mechanics. Further investigation is needed to understand how cognitive function can be improved to decrease the risk of future non-contact LE injury, address these deficits and to better understand how baseline cognition and dual task conditions can impact and improve functional rehabilitation protocols. Additionally, it will be important to determine how functional rehabilitation protocols can maximize performance in individuals with a history of concussive event(s) or otherwise lower cognitive function.
Grant support
None.
Financial Disclosure and conflict of interest
Authors have nothing to report.