INTRODUCTION
Exercise often leads to clinical symptoms of pain, soreness, or tightness. Adequate recovery of the involved soft tissues is required in order for increases in exercise capacity and strength to occur with repeated bouts of exercise. This clinical manifestation and progression of exercise-induced muscle damage (also known as delayed onset muscle soreness [DOMS)] commonly begins 6–12 hours after exercise, increases progressively until peak soreness occurs around 48–72 hours, and finally decreases until soreness is completely imperceptible 5–7 days after exercise.1–3 DOMS is often accompanied by impaired muscle contraction and reduced force capacity,2,4,5 while a local or even global area of increased muscle tone is commonly observed.6–9 DOMS is also associated with reduced range of motion (ROM) and altered biomechanical function of the adjacent joints.2,4,5,10,11 It is commonly accepted that the main mechanisms of DOMS are related to ultrastructural damage of skeletal muscle, sarcolemmal disruption, and Z-Band streaming, caused by intense and exhausting exercise and/or unfamiliar sporting activity.7,12,13
An important determinant of muscle function is musculotendinous architecture, which is the arrangement of contractile and connective tissue elements within a muscle.14 Pennation angle (PA), defined as the angle between the muscle fiber and the intramuscular tendon, is an important architectural and functional factor of a pennate muscle.15 Additionally, muscle thickness (MT), the distance between the superficial and deep tendon aponeurosis,14,16 can be considered an indirect measure of strength and can also be an important factor influencing a muscle’s function.4,14,16–19 Passive muscle-tendon lengthening has been shown to decrease PA and decrease muscle width and depth in the medial gastrocnemius.20 These architectural changes are associated with increased ROM. Therefore, changes in muscle architecture can serve as an indicator of individual muscle tightness, which are consequences of DOMS.8
Low intensity training has been suggested after eccentric or high-intensity training sessions with the thought of reducing DOMS.7 It has been proposed that the short-term alleviation of pain during exercise is due to the breakup of adhesions in the sore muscles, an increased removal of noxious waste products via an increased blood flow, or an increased endorphin release.21 Due to this theory, research has become focused on creating similar effects with passive modalities. Percussive therapy is a recent therapy that delivers gentle, rhythmic pulses to soft tissue with the use of a handheld device or therapeutic massager. These commercially available devices fall under classification as a therapeutic massager which is defined by the FDA as “an electrically powered device intended for medical purposes, such as to relieve minor muscle aches and pains.” It is suggested that these devices are able to “soften” muscle tissue, alleviate pain, and improve blood flow, which is similar to the suggested effects of instrument assisted soft tissue mobilization (IASTM) when used to reduce DOMS. However, some individuals have increased soreness or a negative response following an acute bout of percussive therapy.
Percussive therapy has only been scientifically investigated in one recent study, and no studies were identified that examine the varying soreness response of participants.22 Also, no study has evaluated the effects of percussive therapy at the shoulder. Evaluating the varying soreness response of participants can help clarify why some participants experience worsened muscle soreness after percussive therapy. Additionally, it is unknown if there is any effect of percussive therapy on shoulder ROM, strength, and muscular architecture, which is an important determinant of muscle function and underlying mechanisms for tissue ROM and strength.14 Researching the effects of percussive therapy on healthy controls is a valuable assessment for understanding basic mechanistic changes at the shoulder, which can lead to future research in injured and athletic populations.
Therefore, the primary purpose of this study is to compare the acute effects of percussion therapy on passive range of motion (ROM) and tissue-specific ultrasound measures (pennation angle [PA] and muscle thickness [MT]) between healthy individuals responding positively vs. negatively to percussive therapy performed on the dominant arm posterior rotator cuff.
MATERIALS AND METHODS
This study used a cross-sectional laboratory study. A convenience sample of healthy and active individuals were recruited through advertisement at a local university. No study participants were competitive collegiate athletes. Only participants 18-40 years of age with no upper extremity injuries/surgeries within the prior year were included.
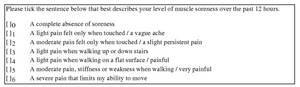
Study approval was received by the Temple University Institutional Review Board (IRB). Participants read and signed an IRB-approved consent form and completed a health history questionnaire. A previously developed Likert Scale of Muscle Soreness was used to determine the participants’ level of soreness specific to their shoulder prior to and following treatment (Figure 1).23 The original scale was adapted to focus on pain throughout the shoulder ROM instead of during walking. A change in score was then calculated as the difference in Likert score from pre- to post-treatment to determine if the participant experienced a change in muscle soreness as a result of percussive therapy. Participants with no change or a decrease in muscle soreness were assigned to the “positive” response group and participants who reported an increase in muscle soreness were assigned to the “negative” response group. Clinical measures and muscle architecture (via ultrasound) were evaluated before percussive therapy, and then 20 minutes after percussive therapy intervention.
Glenohumeral Range of Motion
For ROM, participants were asked to lie supine on a treatment table with their dominant shoulder abducted to 90 degrees and elbow flexed to 90 degrees. One tester (S.J.T.) used one hand to stabilize the scapula over the anterior shoulder and the other hand to rotate the participant’s shoulder into IR until scapular motion was detected. A second tester (M.P.) placed a digital inclinometer (Saunders Group Inc, Chaska, MN) along the lateral forearm and recorded the amount of glenohumeral rotation (degrees). Three measurements were obtained and the average was calculated. The same procedures were completed for external rotation. Reliability for the testing investigator was previously established and published.24
Glenohumeral Strength
For isometric strength, participants were asked to lie supine on a treatment table with their dominant shoulder abducted to 90 degrees in neutral rotation and elbow flexed to 90 degrees. A tester (S.J.T.) then placed a digital hand-held-dynamometer (Hoggan Health Industries, Draper, Utah) at the distal wrist on the dorsal (posterior) side and instructed the participant to maximally contract in the direction of ER for five seconds. The same procedures were completed for IR, except for the digital hand-held-dynamometer being placed on the ventral (anterior) side of the distal wrist. This was repeated three times and the mean recordings were utilized for data analysis.
Muscle Architecture
All ultrasound imaging was performed by one investigator (S.J.T.) using a 15-MHz linear-array transducer (FujiFilm Sonosite Inc. Bothel, WA, USA) using previously-published ultrasound techniques to measure muscle architecture.25 For ultrasound imaging, male participants were asked to remove their shirts, while female participants were asked to wear a tank top prior to arriving. All participants were seated in a chair with their forearm resting on their thigh. For images of the infraspinatus and teres minor, the tester placed standard ultrasound gel on the ultrasound probe and placed it directly on the participant’s skin for the scanning of each muscle. To evaluate the infraspinatus, the transducer was placed horizontally just lateral to the infraspinous fossa at the medial border of the scapula. The transducer was moved horizontally from the infraspinous fossa towards the infraspinatus insertion at the posterior aspect of the greater tuberosity for the clearest image of the muscle fascicles and tendon aponeuroses. To visualize the teres minor, the transducer was placed horizontally just lateral to the inferior angle of the scapula. The transducer was moved laterally at a diagonal toward the humeral head until the clearest image of the muscle fascicles and the tendon aponeuroses.
Percussive Therapy Intervention
For the percussive therapy, participants were asked to lie prone on a treatment table with their arms by their side. Five minutes of percussive therapy (Power Massager Pro, TimTam, TT Therapeutics LLC., Missouri City, TX) was administered along the infraspinatus and teres minor muscle belly using the default ball-shaped articulating head (Figure 2). Due to the articulating head and 20-mm stroke length, the head of the percussion massager was able to target the infraspinatus and teres minor simultaneously. The device delivered a percussive frequency of 2800 strokes per minute while the tester guided the device across the infraspinatus and teres minor muscle bellies back and forth from origin to insertion. The tester continued to guide the device back and forth along the muscle bellies for all five minutes of the intervention session.
Image Analysis
ImageJ software (National Institutes of Health, Bethesda, MD) was used to assess PA and MT utilizing a previously-published and reliable technique.25 The superficial PA was quantified by measuring the angle between the deep aponeurosis and the muscle fascicles superficial to the deep aponeurosis, while the deep PA was quantified by measuring the angle between the deep muscle fascicles and the deep aponeurosis. This definition of superficial and deep PA was used for both the infraspinatus and teres minor. In contrast, MT quantification varied between the infraspinatus and the teres minor due to differences in measurement location. Infraspinatus MT was measured at the location of the suprascapular notch for consistency (Figure 3), while teres minor MT was measured at the location of the most lateral aspect of the scapula (Figure 4). MT was measured between the top of the muscle and the bottom of the muscle at these specified locations. Two subjects’ teres minor data was excluded from the analysis due to poor image quality.
Statistical analysis was performed using SPSS version 26.0 (SPSS IBM Inc. Armonk, NY). Independent sample t-tests were utilized to compare continuous demographic variables between groups, while Fisher’s exact tests and Chi Square tests were used to compare categorical demographic variables. Finally, separate one-way ANOVAs were used to compare the change in clinical measures and muscle architecture between groups (positive and negative). The alpha level was set to p≤0.05.
RESULTS
Fifty-five recreationally active participants (29 male, 26 female) were included with a mean age of 23.7 ± 3.4 years. Eighteen participants (32.7%) reported a decreased Likert score (Negative response group; i.e. worse subjective shoulder soreness) after percussive therapy, while 37 (67.3%) reported either the same Likert score or an increased Likert score (Positive response group; i.e. similar or improved subjective shoulder soreness) after percussive therapy. There were no significant demographic differences between the positive and negative groups (Table 1).
The negative group had decreases in IR ROM (-1.3° negative) as compared to the positive group (2.3° positive, p=0.021) and IR strength (-1.2 lbs vs. 1.1 lbs, p=0.011, respectively) after percussive therapy (Table 2) (Figure 5). Meanwhile, the positive and negative groups had similar changes in ER ROM and ER strength due to percussive therapy. Regarding muscle architecture, the negative group had a greater change in teres minor thickness (0.11 mm vs. 0.00 mm, p=0.019) after percussive therapy (Figure 6). All other muscle architecture changes were similar between groups.
DISCUSSION
The results of this current study found that participants with a self-reported negative response to percussive therapy had worsened dominant arm IR ROM and IR strength, and increased teres minor MT, after percussive therapy compared to the positive response participants. Meanwhile, both groups had similar changes in ER ROM and ER strength, PA of the infraspinatus and teres minor, and MT of the infraspinatus.
The pain gate theory may explain the differential response among participants (positive and negative groups). The theory states that sensory stimulation can activate either large and fast non-nociceptive fibers (Aβ fibers) leading to alleviation of pain and/or soreness, or smaller nociceptive fibers (Aδ and C fibers) leading to exacerbated pain and soreness, for 30 minutes or longer.26–28 When percussive therapy is applied to the posterior shoulder muscles, the speed at which the percussion massager compresses the muscles may be over-stimulating the muscles with non-nociceptive impulses, thus blocking the nociceptive impulses. The blocking of these nociceptive impulses is thought to result in a relaxation effect that inhibits muscle guarding when there is sensory input related to pain or soreness. However, the negative group may have highly sensitive nociceptive fibers that became activated during percussion therapy, resulting in increased soreness and muscle guarding after percussive therapy. This potential response following percussion therapy should be considered by clinicians prior to implementation into a warm-up, injury prevention, or rehabilitation protocol.
The current study found that the positive group had increased IR ROM by almost 4 degrees compared to the negative group following percussion therapy. Conversely, the posterior shoulder muscles in the positive group may have exhibited an increased mechanical softening effect as shown by an IR ROM increase of about 2 degrees. However, the clinical significance of either of these changes is unclear due to the numerical values not exceeding measurement error. Mechanical softening of the tissue is the result of various mechanical forces including compression, tension, torsion, or shear on the tissues, which can lead to the tissue becoming more pliable.29,30 The softening could have allowed more elasticity in the passive elements of the muscle and allowed a greater degree of stretch. Treatment was only applied to the external rotator muscles which would allow greater stretch into IR. Since treatment was isolated to the ER muscles, it is not surprising that there were differences in IR ROM but no changes in ER ROM. The observed differences may be explained by the muscle soreness after percussive therapy causing an increased nociceptive response, and also a slight increased teres minor MT, which was likely a result of increased blood flow. Increased fluid volume either in a muscle or joint has the potential to limit joint ROM as seen in acute muscle and joint injuries that result in swelling. Previous research has shown that blood volume can have an effect on passively stretched and actively contracted muscles. For example, a previously published theoretical model, small increases in intramuscular volume can lead to a 50% increase in passive stretch tension.31 Another study found that increasing the fluid volume of the muscle in a bullfrog by 40% resulted in a 69% increase in tension produced during passive stretch.32 However, since the increased MT was very minimal, the clinical significance is questionable.
Interestingly, the authors did not find any group differences in muscle PA. Previous research has found that the PA of muscles is adaptable and can change due to alterations in the passive components of muscle or the neuromuscular activation of a muscle.33 Due to the acute increase in soreness in the negative group, the authors expected there would be more involuntary activation to the muscle at rest in these patients, resulting in an increased PA. However, PA changes were similar to the positive group, suggesting that a single bout of percussion therapy does not affect the involuntary activation of the posterior rotator cuff muscles. Future research examining a longitudinal, repetitive application of percussion therapy may clarify this relationship.
Unlike traditional warm-up programs with static stretching pre- or post-competition, which often results in a loss of strength, percussive therapy appears to elicit the benefits of static stretching without a reduction in strength for individuals who respond positively to the treatment. In a clinical setting, increasing ROM while maintaining strength is crucial to performance and the reduction of injury risk. For example, overhead athletes tend to lose IR ROM and strength as the competitive season progresses, resulting in decreased performance and/or increased injury risk.34–38 However, individuals interested in using percussive therapy may be tested to determine their soreness response.30,39–41 Those who respond positively to percussive therapy may benefit from the implementation of percussive therapy into their injury prevention and/or rehabilitation programs.
There are several limitations to this study. First, muscle soreness was quantified using a self-reported Likert scale which is subject to reporter bias. Also, only healthy volunteers were included in this study, so findings may not be generalizable to injured or athletic populations. Finally, while statistically significant differences were observed, the clinical relevance of the study findings could not be clarified. Future research that includes injured and/or athletic populations can help clarify the clinical applicability of percussive therapy and identify patient populations that benefit significantly from the treatment.
CONCLUSION
The results of the current study indicate that participants with a positive response to percussive therapy had increased dominant arm IR ROM and IR strength, and decreased teres minor MT, after percussive therapy compared to the negative response participants.
Acknowledgements
Thank you to TT Therapeutics (Missouri City, TX) for providing the percussive therapy device.
Disclosures
Jack Trainer: Received percussion therapy device from TT Therapeutics to perform the study. Was hired and shortly worked for TT Therapeutics after completion of the study. TT Therapeutics was not involved in the data collection, analysis, interpretation, writing, or approval of the study.
Matthew Pascarella: None
Ryan Paul: None
Stephen Thomas: None



_range_of_motion_(rom)_and_strength_bet.jpeg)
_muscle_thickness_between_positive_response_an.jpeg)




_range_of_motion_(rom)_and_strength_bet.jpeg)
_muscle_thickness_between_positive_response_an.jpeg)