INTRODUCTION
Traumatic shoulder instability is a common upper extremity injury.1 Incidence rates range from 23.9 per 100,000 person-years in the general population2 to 435 per 100,000 person-years in military cadets.3,4 Surgical stabilization reduces recurrence and improves self-reported function compared to conservative management for active young adults.5,6 Return to sport typically occurs six months postoperatively, with time from surgery used as the primary measure of readiness.7 However, athletes often lack rotational strength and upper extremity performance,8 with only 80% of athletes and 68% of overhead throwing athletes reaching their pre-injury play level.9 Since the rotator cuff stabilizes the humeral head within the glenoid, incomplete recovery of rotational strength may contribute to recurrent instability and failure to return to sport following shoulder stabilization surgery.
Exercising with loads at 70-85% of one-repetition maximum improves muscle strength but is challenging, symptom-producing, or sometimes even contraindicated following surgery.10 Blood flow restriction (BFR) training uses a tourniquet to impede arterial inflow while occluding venous return, stimulating anaerobic metabolism without heavy resistance.11–14 Blood flow restriction training is safe and well-tolerated in the acute phase of tissue healing.11,14,15 Local physiologic adaptations from BFR training primarily occur in muscles distal to tourniquet placement. However, increased metabolite accumulation, selective recruitment, cellular swelling, and myostatin down-regulation may activate a systemic release of anabolic hormones − growth hormone and insulin-like growth factor-1 − suggesting BFR training may stimulate muscle growth proximal to tourniquet placement.1–5,13,16–19 Long occlusion times with combined aerobic and anaerobic exercise may add to the systematic release of anabolic hormones, further contributing to proximal muscular adaptations seen with BFR training.4–6
Exercising with BFR is gaining popularity for upper extremity injuries,20–24 but its effectiveness following shoulder stabilization surgery requires additional exploration. Therefore, the purpose of this case series was to observe changes in shoulder strength, self-reported function, upper extremity performance, and range of motion (ROM) in military cadets recovering from shoulder stabilization surgery who completed a standard rehabilitation program with six weeks of BFR training.
METHODS
This study was a prospective case series. Eligible participants were current military cadets, fluent in English, and within six weeks of shoulder stabilization surgery. Shoulder stabilization was defined as any procedure to tighten or repair the glenoid labrum or glenohumeral ligaments. Participants were excluded if they were immunocompromised; required general anesthesia for another medical procedure within six weeks of consent; underwent concomitant rotator cuff repair; had a humeral neck or shaft fracture; or had a history of deep vein thrombosis, endothelial dysfunction, or bleeding disorders.
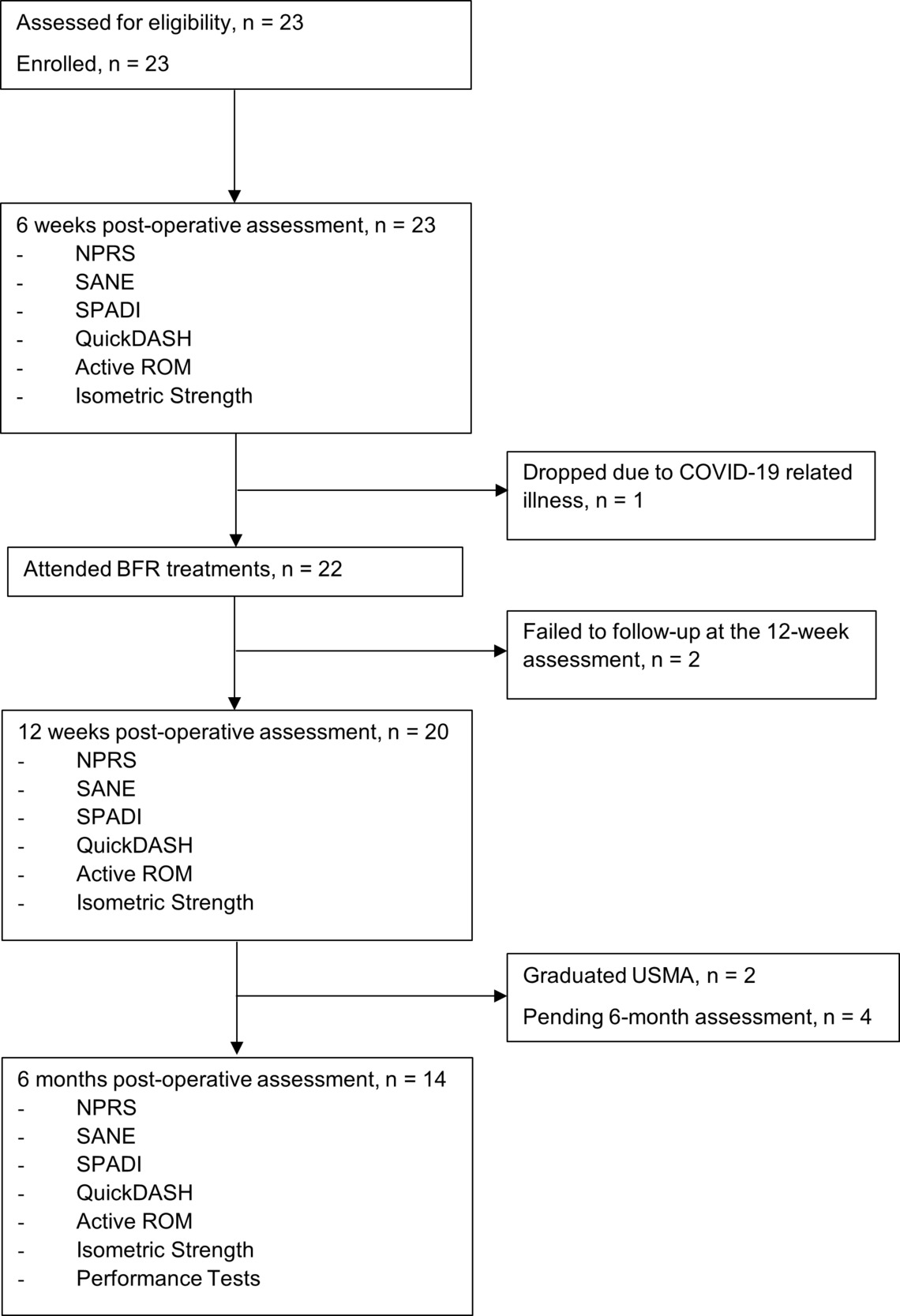
Twenty-three military cadets, status-post shoulder stabilization surgery were screened for eligibility and enrolled in the study (Figure 1). The most common surgical procedure performed was a Bankart repair of the anterior-inferior glenoid labrum. Of the 23 participants, three dropped from the study, with two failing to follow up within the required time points and one unable to receive BFR treatments after enrollment due to COVID-19-related illness. Eighteen participants completed all follow-up assessments, with two graduating before the six-month evaluation.
Physical Therapist
A single physical therapist recruited, treated, and assessed the outcomes on all participants. The physical therapist was board certified in orthopedic physical therapy and a fellow in training at a Division 1 sports physical therapy fellowship program. The physical therapist provided tailored manual therapy and home exercise programs addressing individual impairments as needed as part of standard rehabilitation.
Blood Flow Restriction
Blood flow restriction treatments began post-op week six when participants were cleared from ROM restrictions and permitted to begin isotonic resistance exercises. Participants performed two to three BFR treatments per week in addition to a standard rehabilitation protocol. A Delfi Personalized Tourniquet System (Delfi Medical Innovations Inc., Vancouver, Canada) was used to automatically regulate pressure with the tourniquet (18 x 4.5-inch contour cuff) applied to the upper brachium of the surgical extremity (Figure 2). Inflation time was set to 30 minutes, and limb occlusion pressure was set to 50%. The tourniquet remained inflated during all exercises but did not exceed 30 minutes per session.
Determining Intensity and Resistance
Perceived exertion is a good indicator of physical strain and is used to help prescribe and regulate intensity during aerobic and anaerobic training.25–29 Participants were given a Rating of Perceived Exertion (RPE) scale at the beginning of each treatment.29 Before applying the tourniquet, participants performed a few repetitions of each exercise without BFR on both extremities to determine the load-RPE for their working sets.26 For their surgical extremity, participants selected a resistance at an RPE between seven (extremely light) to nine (very light), corresponding to 30% of a one-repetition maximum effort.26 This was used as the starting resistance for their surgical extremity. On their non-surgical extremity, participants performed the same procedure but selected a resistance at an RPE between 15 (hard) to 17 (very hard), corresponding to between 70% to 90% of a one-repetition maximum effort.26 Participants were permitted to adjust the resistance as needed but were instructed to keep pre-BFR resistance within the predetermined RPE ranges.
Aerobic Exercise
Participants began treatment with an upper body cycling exercise on a Biodex Upper Body Cycle (UBC) (Model 950-138, Shirley, New York). Participants cycled forward at their self-selected pace for five minutes at a pre-BFR resistance RPE between nine (very light) to eleven (light).27
Strength Exercises
Participants performed three strengthening exercises targeting the rotator cuff and periscapular musculature: resisted external rotation, scapular retraction with shoulder extension, and scapular plane abduction. A Keiser Functional Trainer (Keiser Corp model 003025.15, Fresno, CA) was used to adjust resistance and transition between extremities and exercises easily. For the surgical extremity, four sets of each exercise were performed using the 30-15-15-15 repetition method recommended by Patterson et al.14 For the non-surgical extremity, four sets of 12 repetitions were performed without BFR. Participants alternated between extremities completing one exercise before moving to the next. If participants failed to complete all exercises in the allotted 30 minutes, the tourniquet was removed, and participants finished the remaining exercises without BFR.
Outcome Measures
Primary outcomes included shoulder isometric strength and patient-reported function measured from the surgical date at three follow-up assessments: six weeks, 12 weeks, and six months. Secondary outcomes included physical function assessed by performance tests during the six-month follow-up and shoulder active range of motion measured at six weeks, 12 weeks, and six months postoperatively.
Isometric Strength
The physical therapist assessed isometric shoulder external rotation, internal rotation, and abduction strength using a hand-held dynamometer (Microfet 2, Hoggan Health Industries Inc. Draper, UT, USA). Hand-held dynamometry is reliable and has concurrent validity with isokinetic testing while being practical in a clinical setting.30 Participants performed a submaximal effort at 50% before performing two test efforts in each position. Test efforts consisted of a five-second maximal contraction. The surgical extremity was tested before the non-surgical extremity. Strength was normalized by dividing the average force in kilograms produced by kilograms of body mass and then compared to the contralateral extremity. For analysis, a percent change of 15% is considered clinically meaningful.31
External and internal rotation strength was assessed in the supine position with the shoulder in 45 degrees of abduction (Figure 3). This position stabilizes the scapulothoracic articulation and is described as the optimal position to reduce the coefficient of variation.32–34 A bolster was placed under the elbow to maintain neutral shoulder flexion and extension and between the arm and trunk to maintain 45 degrees of abduction.34 The hand-held dynamometer was positioned proximal to the styloid process of the wrist joint.
Abduction strength was assessed with the participant seated on the plinth with their shoulder abducted 45 degrees in the scapular plane.34 The hand-held dynamometer was placed proximal to the elbow.
Patient-reported Function
Participants completed the Numeric Pain Rating Scale (NPRS), the Single Assessment Numeric Evaluation (SANE), the Shoulder Pain and Disability Index (SPADI), and the modified Disability Arm Shoulder Hand (QuickDASH) at each follow-up assessment. The NPRS assessed pain intensity on an 11-point scale (zero being no pain and ten being the worst). The NPRS is reliable, valid, and responsive, with a change of two or more considered clinically meaningful.35 The SANE assessed shoulder function as a percentage of normal (zero being no function and 100% being normal). The SANE is reliable, valid, and responsive, with a change of 15% considered clinically meaningful.36,37 The SPADI and QuickDASH are reliable, valid, and responsive for assessing pain and disability for multiple shoulder conditions. A change of 18 points was considered clinically meaningful for the SPADI38,39 and 16 points for the QuickDASH.40–42
Performance Tests
Participants performed the CKCUEST (Figure 4a), the UQYBT (Figure 4b), and the USPT (Figure 4c) following isometric strength testing at the six-month follow-up assessment. The surgical shoulder was assessed before the non-surgical shoulder for all tests.
The CKCUEST is a reliable measure of upper extremity closed kinetic chain function.43 Participants assumed a standard push-up position with their hands placed inside two pieces of athletic tape measured 36 inches apart and their feet no more than 12 inches apart. When instructed, participants reached, alternating hands, touching the athletic tape under the opposite hand. The total number of cross-body touches in 15 seconds was recorded. Participants performed a submaximal trial before performing three test efforts. An average of three efforts was used for analysis. Results were compared to reference values with a score of greater than or equal to 21 touches considered above average for healthy college-aged students.8,43–45
The UQYBT is a reliable measure of unilateral upper extremity closed kinetic chain excursion.44,46 Participants assumed a standard push-up position with their feet no more than 12 inches apart. Participants reached as far as possible in three directions with their free hand. Participants performed three practice trials before performing three test efforts.44 A total excursion score was calculated by summing the average of each reach direction. A composite score was calculated to normalize for limb length, taking the total excursion distance and dividing it by three times the upper limb length.44 Limb symmetry index (LSI) was then calculated by dividing the composite score of the surgical extremity by the composite score of the non-surgical extremity and then multiplying by 100. Scores were compared to reference values from a cohort of military cadets, with an LSI of 95% considered normal.44
The USPT is a functional test of upper extremity power with good test-retest reliability in college male and female athletes.47,48 Participants sat with their back against a wall, feet flat on the floor, knees at a 90-degree angle, and their non-testing hand across their chest. In a pushing motion, participants maximally tossed a 2.72-kilogram medicine ball from shoulder height as far forward as possible while keeping their head, non-tested scapula, and back in contact with the wall. Participants performed three submaximal practice tosses before performing three test efforts. Using the methods described by Chmielewski et al., average scores were allometrically scaled ([distance (cm)/body mass (kg)]0.35) with body mass as the anthropometric measure.48 The exponent 0.35 removed the influence of body mass, yielding a body size-independent measure.48 An LSI of 90% accounted for limb dominance and was considered normal.48
Active Range of Motion
Before isometric testing, the physical therapist measured active flexion, external rotation, and internal rotation using a digital inclinometer (Baseline Digital Inclinometer 12-1057; Fabrication Enterprises INC, New York, USA). Participants were positioned supine with their knees flexed, feet flat, and low back flush on a standard treatment plinth. Measurement was recorded at the end of available active ROM (loss of test position or limitation due to pain). Two trials were completed bilaterally, with the average used for analysis.
Shoulder flexion was measured with the digital inclinometer positioned on the arm between the olecranon process and axilla for flexion. External and internal rotation were measured in 90 degrees shoulder abduction, 90 degrees elbow flexion, and neutral forearm rotation.49,50 The distal half of the humerus was positioned off the plinth to allow for full ROM. The therapist applied manual anterior-posterior pressure to the humeral head to decrease compensatory movements.49,50 The digital inclinometer was placed on the forearm between the ulnar styloid process and the olecranon process.49
DATA ANALYSIS
Descriptive statistics, including central tendency and variability measures, were the primary means of analyzing data. A one-way, repeated-measures analysis of variance was used to analyze changes in all outcome measures over time. An alpha of .05 was set with time as the within-subject factor. A Bonferroni correction was used for three planned pairwise comparisons to examine the differences between the various time points (α = .0167), with 95% confidence intervals (CIs) calculated for mean differences. All data were analyzed using SPSS Version 28 for Windows software (SPSS Inc, Chicago, IL.).
OUTCOMES
Participant characteristics are summarized in Table 1.
Isometric Strength
Participants experienced statistically significant improvements in surgical extremity external rotation strength (F = 10.0, p < 0.001), abduction strength (F = 25.8, p < 0.001), and internal rotation strength (F = 11.3, p < 0.001). Post hoc comparisons revealed statistically significant increases in external rotation strength, internal rotation strength, and abduction strength from six to 12 weeks (Table 2). From six weeks to 12 weeks, 17 of 20 participants achieved clinically meaningful improvements in surgical extremity external rotation strength (Figure 5), 17 of 20 for abduction strength, and 14 of 20 for internal rotation strength. No statistically significant strength increases occurred in the non-surgical extremity.
Patient-reported Function
Participants experienced statistically significant improvements in reported function measured by the SANE (F = 19.7, p < 0.001), the SPADI (F = 24.8, p < .0001) and the QuickDASH (F = 61.8, p < 0.001). Post hoc comparisons revealed statistically significant improvements and clinically meaningful improvements on the SANE and SPADI from six to 12 weeks and statistically significant improvements on the SANE, the SPADI, and QuickDASH from six weeks to six months (Table 3). From six to 12 weeks, 16 of 20 participants achieved clinically meaningful improvements on the SANE and 17 of 20 on the SPADI.
Performance Tests
Five of 18 participants met or exceeded reference values on all three performance tests, nine of 18 passed only two tests, three passed only one test, and one participant failed to pass a single test (Table 4). Only three of 18 participants met or exceeded reference values on all performance tests and had 90% limb symmetry for each isometric strength measure at the 6-month assessment. No performance test had a higher pass rate, as 12 of 18 participants met the reference value for each test.
Active Range of Motion
Participants experienced statistically significant improvements in surgical extremity external rotation ROM (F = 40.02, p < 0.001), flexion ROM (F = 33.56, p < 0.001), and internal rotation ROM (F = 16.7, p < 0.001). Post hoc comparisons revealed statistically significant improvements in surgical extremity ROM across all timepoints (Table 5).
DISCUSSION
This case series aimed to observe changes in shoulder strength, self-reported function, upper extremity performance, and shoulder ROM in military cadets recovering from shoulder stabilization surgery who completed a standard rehabilitation program with six weeks of BFR training. To the authors’ knowledge, this is the first study to explore the addition of upper extremity BFR training to rehabilitation following shoulder stabilization surgery. Statistically significant and clinically meaningful improvements in shoulder strength and self-reported function were observed in participants who performed BFR training twice a week, beginning six weeks postoperatively. Most participants met or exceeded reference values on two upper extremity performance tests. No adverse events occurred, and no participant discontinued BFR treatments.
Few studies have examined BFR training for the upper extremity, and even fewer have examined BFR training following an upper extremity musculoskeletal injury.20–24 In a randomized study of 32 healthy adults, Lambert et al. compared BFR training to low-intensity exercise alone on rotator cuff strength and endurance.23 After eight weeks of BFR training, the only statistically significant between-group change was increased internal rotation strength for participants in the BFR group. Likewise, Brumitt et al. found no between-group difference in rotator cuff strength in 46 healthy participants who performed BFR training compared to those who performed exercise alone.24
In contrast, Bowman et al. found BFR training to be more beneficial than exercise alone in improving shoulder strength in 24 healthy adults.22 After six weeks of training, participants in the BFR group averaged 48%, 39%, and 33% improvement in shoulder scaption, flexion, and abduction isometric strength, respectively.22 Regarding rotational strength, participants in the BFR group averaged a peak torque improvement of 11% for internal rotation and 15% for external rotation.22 Participants in the BFR cohort performed exercises with continuous BFR on one extremity and without BFR on the contralateral extremity, whereas Lambert et al. and Brumitt et al. had participants perform exercises on one extremity.22–24
In the current study, surgical extremity external rotation, abduction, and internal rotation strength improved by an average of 42%, 44%, and 40% from six weeks to 12 weeks, whereas, the non-surgical extremity had a percent change of six percent, seven percent, and minus seven percent respectively. Our BFR parameters were consistent in training frequency, tourniquet pressure, and restriction method outlined by a panel of experts in occlusion training.14 The protocol followed methods outlined by Cancio et al., who found 30 minutes of low load continuous BFR training at 50% limb occlusion pressure more beneficial in improving self-reported function than standard care alone in participants recovering from distal radius fractures.20 Like Cancio et al., no participant in the current study discontinued BFR treatments. However, five participants in our study needed the limb occlusion pressure reduced from 50% to 40% during the initial BFR treatment due to moderate discomfort in the surgical extremity.
Studies investigating a return to sport criteria following shoulder stabilization surgery have identified time from surgery as the most common indicator of readiness, with athletes typically cleared for sport between five to six months postoperatively.7,51 Wilson et al. used a battery of tests consisting of isokinetic strength testing and two functional tests to assess return to play readiness in competitive athletes six months following shoulder stabilization surgery.8 Only 20 of 43 athletes had an LSI of 90% for internal rotation strength, and only 12 of 43 had an LSI of 90% for external rotation strength.8
The current study observed an LSI of 90% in 13 of 20 participants for internal rotation strength and nine of 20 for external rotation strength at 12 weeks postoperatively. At six months, an LSI of 90% was observed in 12 of 18 participants for internal rotation strength and 11 of 18 for external rotation strength. While Wilson et al. did not assess abduction strength, an LSI of 90% for abduction was observed in 14 of 20 participants at 12 weeks and 13 of 18 at six months postoperatively. Despite the observed improvements, only three of 18 participants had 90% limb symmetry on all strength measures and met reference values on all performance tests at the six-month assessment, suggesting the need for further research to define the best return to sport criteria after shoulder stabilization surgery.
Although the authors are uncertain of the mechanism of action and contribution that BFR had to the observed improvements in the current study, the results are promising and, at minimum, provide preliminary data for future studies.
Limitations
While statistically significant and clinically meaningful changes in shoulder strength and self-reported function were observed, a causal relationship between intervention and outcome cannot be assumed. The small sample size and lack of a control group mean observed changes may have been a product of time, the natural progression of the condition, or standard rehabilitation. The participants were homogenous regarding age, health, and activity level limiting generalizability to populations outside of young athletes. Furthermore, home exercise programs and manual therapy were tailored to participants, possibly confounding the BFR-specific effects.
CONCLUSION
After shoulder stabilization surgery, significant improvements in shoulder strength, self-reported function, and ROM were observed with six weeks of BFR training in 20 military cadets. No participant discontinued the BFR treatments, and no adverse events occurred. While the degree of improvement attributable to the addition of BFR is unknown, the clinically meaningful improvements in shoulder strength, self-reported function, and upper extremity performance warrant further exploration of BFR during upper extremity musculoskeletal rehabilitation. Future studies should include randomized control groups with and without BFR and explore varying occlusion times to determine the effectiveness of adding BFR to standard postoperative rehabilitation.
DISCLOSURE/DISCLAIMER
The authors have no relevant or material financial interests that relate to this study. The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the United States Army or Department of Defense.
ETHICS APPROVAL
Study was approved by the Naval Medical Center Portsmouth Institutional Review Board



_closed_kinetic_chain_upper_extremity_stability_test_(ckcuest)__(b)_upper_quarter-y-bal.jpeg)



_closed_kinetic_chain_upper_extremity_stability_test_(ckcuest)__(b)_upper_quarter-y-bal.jpeg)
