INTRODUCTION
Developmental dysplasia of the hip (DDH) defines a hip joint with reduced acetabular coverage of the femoral head1 and is prevalent in 32% of primary care patients with hip pain.2 The radiologic features of dysplasia are found in 3-20% of the general population.3,4 Patients with DDH may experience hip pain, impaired physical function, and low quality of life.5–9 An association with DDH and early development of hip osteoarthritis (OA) has been established10 with three times greater odds of progressing from mild to end-stage OA or total hip replacement.11,12 The acetabular coverage can be increased with the surgical procedure, periacetabular osteotomy (PAO).1,13 The goal of the PAO is to reduce the likelihood of hip OA by increasing the acetabular coverage of the femoral head.14
Historically, outcomes of PAO have been derived from surgeons’ definition of success,15,16 which are often based on imaging outcomes.1,13,15 However, in recent years, there has been a shift towards including other measures of successful surgery, including physical impairments and patient-reported outcomes.7,17,18 This is supported by studies which suggest structural pathology may not be the sole contributing factor to pain.19,20 For example, a high prevalence of labral tears (54%) has been shown to exist in asymptomatic subjects.19 Mose et al. also reported no association between the level of pain and severity of labral lesions or to the degree of bony coverage in patients with DDH.20 For patients to give truly informed consent to undergo PAO, there must be robust evidence of the likely outcome of surgery on not only pain, but also in regard to physical function.21
Physical impairments may potentially explain deficits in in those with worse outcomes following PAO. Patients with DDH who undergo PAO have reported improvements in pain, function, and quality of life. However, up to 32-months after PAO, these outcomes were still significantly worse compared with asymptomatic participants.9 It is possible that these deficits are related to physical impairments. Physical impairments after PAO have been reported in individual studies.7,8,17,22–25 However, no reviews have systematically synthesized physical impairments in patients with DDH undergoing PAO. For future patients to be appropriately informed, and to improve clinicians’ knowledge and ability to help these patients, a systematic review on physical impairments in patients with DDH undergoing PAO is warranted.
This systematic review aimed (i) to compare physical impairments in patients undergoing PAO for DDH to asymptomatic participants, and (ii) to investigate pre- to post-PAO changes in physical impairments in patients with DDH.
METHODS
Study selection, eligibility criteria, data extraction, and statistical analysis were performed according to the Cochrane Collaboration guidelines.26 The systematic review was reported in accordance with the preferred reporting guidelines for systematic reviews and meta-analysis (PRISMA) guidelines,27 and was registered on the Prospero international prospective register of systematic reviews (ID: CRD42020180571).
Search Strategy
A comprehensive, reproducible search strategy was performed on the following databases MEDLINE CINAHL, EMBASE, Sports Discuss, and PsychINFO from inception until 5th January 2021.
The search strategy was conducted by two reviewers (MO, AS) and used the following concepts:
(i) Humans with DDH aged 15 years and older
(ii) Periacetabular Osteotomy
(“Joint Instability”[Mesh] OR instability[tiab] OR unstable[tiab] OR lax[tiab] OR laxity[tiab] OR
subluxation[tiab] OR dysplasia[tiab] OR dysplastic[tiab] OR anterversion[tiab] OR
retroversion[tiab]) AND (Periacetabular [Mesh] OR periacetabular [tiab] OR Osteotomy[Mesh] OR osteotomy [tiab]) AND (Hip[Mesh] OR Hip[tiab] OR hips[tiab] OR “Hip Joint”[Mesh] OR “coxofemoral joint”[tiab]) OR Pelvis [Mesh] OR Pelvis [tiab] OR Pelvic [Mesh] OR Pelvic [tiab])
The search strategy was modified for each database. All potential references were imported into Endnote X8 (Thomson Reuters, Carlsbad, California, USA) and duplicates were removed. All included studies were then uploaded into Covidence software (Veritas Health Innovation Ltd, Australia) for screening. Title, abstract and full text screening was conducted by three independent reviewers (MO (A-Z), CS (A-M), LT (N-Z). Any disagreements were resolved by a fourth independent reviewer (JK).
Eligibility criteria
Studies were eligible for inclusion if they used a hip-specific physical impairment measure and were written in English. All quantitative observational study designs were considered eligible including randomised control trials, non-randomised controlled trials, case series, prospective or retrospective study designs. Animal studies and case studies were excluded.
Participants/Population
People aged 15 years and older with DDH undergoing PAO (based on the mean or median age of the study sample) were included. Studies were not eligible if the PAO was undertaken in people with Cerebral Palsy, Down Syndrome or Charcot-Marie Tooth Disease.
Intervention(s), Exposure(s)
Studies that used PAO surgery as primary intervention for DDH were included. The terms ‘Bernese Osteotomy’ and ‘Ganz Osteotomy’ were considered interchangeable with ‘Periacetabular Osteotomy’. Studies were not eligible if the PAO was reported to be a ‘rotational’ or ‘curved’ as these procedures differ in surgical technique.
Comparator(s)/control
Studies using sham treatment, no treatment or other treatment (e.g., total hip joint replacement or hip arthroscopy surgery) as the comparator/control treatment were included. We also included studies where no comparison group was present if they used two timepoints (for example: case series). In this instance, the pre-intervention time-point was considered the ‘comparison’.
Outcomes
Primary outcomes of interest were hip-related physical impairment measures. These included pain provocation tests, hip muscle strength, hip range of motion (ROM) and gait analysis.
Quality Evaluation
A modified version of the Downs and Black checklist was used to assess the quality of included studies. This modified version scores 18 potential criteria and has been used in other systematic reviews on hip pain.28 Studies were considered high quality with a score of more than 60%.28 Included studies were rated by two independent reviewers (MO, LT). Any disagreements between reviewers were discussed in a consensus meeting and an independent arbitrator (JK) was employed when consensus could not be met. Agreement between rates was determined using Cohen’s Kappa (κ).
The Grades of Recommendation, Assessment, Development and Evaluation (GRADE)29,30 was applied to assess the quality of evidence for each meta-analysis. The overall GRADE certainty ratings included ‘very low’, ‘low’, ‘moderate’ and ‘high’. Observational data was initially graded as ‘low’ and could be increased or decreased.31 Certainty could be rated up for (i) large magnitude of effect, (ii) clear dose-response gradient suggesting causal relationship, (iii) all residual confounding would decrease magnitude of effect. Certainty could be rated down for (i) methodological quality (if mean modified epidemiology appraisal instrument scored less than 60%), (ii) imprecision (if upper or lower confidence interval (CI) spanned a standardized mean difference (SMD) or standardized paired difference (SPD) of 0.5 in either direction), (iii) inconsistency (if I2 was 25% or greater), (iv) indirectness (if clinically heterogeneous) and (v) publication bias (for example, small studies that are industry-sponsored).
Data extraction, synthesis and analyses
Data were extracted by two independent reviewers (MO, LT) into customized excel worksheets. The following data was extracted: Author, year, country of origin, number of participants, demographic characteristics of participants (age, sex, body mass index (BMI), type of PAO), physical impairment measure, length of follow-up and a summary of findings were collated. Any discrepancies in data extraction were resolved by an independent reviewer (JK).
Studies were grouped according to design including (i) between-group studies (asymptomatic participants or other intervention) or (ii) paired-data studies assessing change between pre- and post-PAO, and by assessment time-points such as 6-months or 12-months post-PAO. If studies used a similar outcome at similar timepoints then we performed meta-analysis using random effects model. For between-group results this was done using Review Manager (RevMan) (Version 5.4.1 The Cochrane Collaboration, 2020) with a SMD and 95% CI for continuous data. For analysis of paired-data studies, an SPD was calculated using R statistical software (version 4.0.4, Metafor package version 3.0-2). The SPD and 95% CI were calculated from the sample size, mean and standard deviation (SD) of the difference between timepoints. SMDs and SPDs of 0.2, 0.5 and 0.8 were interpreted as small, moderate and large effect sizes, respectively.32 Subgroup analyses were performed for different timepoints. Statistical heterogeneity across the pooled data was assessed using an I2 statistic, with 25% considered low, 50% moderate and 75% as high levels of heterogeneity.33 Proportions such as hip impingement test data were pooled using Jamovi (Version 1.8.1.0) providing mean and 95% CI calculations. If SMD or SPD was unable to be calculated due to missing information (such as no variance measure), then we reported this as not estimable.
Where individual studies were not sufficiently homogenous to be included in a meta-analysis, a best evidence synthesis was used to provide an overall rating for the body of information.34 Grading of the best evidence synthesis was completed using previously published criteria.28,35 They were graded as strong (≥2 studies with high methodological quality and ≥75% agreement of findings), moderate (≥2 studies including at least one with high methodological quality and ≥75% agreement), limited (≥1 low methodological quality study, with ≥75% agreement, or one high methodological quality study), conflicting (inconsistent findings <75% agreement), and no evidence.
RESULTS
The search yielded 5017 titles and abstracts for screening. Eighty-one full-text studies were screened, and 57 studies were excluded. There were 24 studies included in the final analyses. An overview of the study identification process is provided in Figure 1.
Methodological Quality
Supplementary Appendix 1 contains the results of quality appraisal using the modified Downs & Black checklist. Initial agreement between quality assessors was moderate (К=0.55).36 The methodological quality scores ranged from 39%37 to 88%,38 with an overall mean (SD) rating of 72% (13.2%). All the included studies clearly described their aims or hypothesis. Only five studies (21%) provided characteristics of patients lost to follow-up and four studies (17%) stated if the main outcome measures used were valid and reliable.
Participants
The 24 studies included 2412 participants, with 2190 of these participants undergoing PAO surgery. A proportion of these participants represent data-points that were published on multiple occasions. Sample sizes of the PAO groups ranged from nine patients39 to 1051 patients.40 One study contained only male participants,38 three studies contained only female participants,39,41,42 and the remaining studies contained both males and females. The mean ages for patients in the included studies ranged from 16 years37 to 39 years.39 Ten studies were cohort studies,7,8,22,23,37,38,43–46 three were case-control studies,47–49 eight were case series,24,25,39–41,50–52 two were of cross-sectional design,17,42 and one was a feasibility study.53
Outcome Measures
Ten studies assessed walking, nine assessed the impingement sign, six measured hip ROM, four assessed strength and one study assessed muscle-tendon pain. Study details are contained in Supplementary Table 1. Two studies provided no SD but did provide inter-quartile range scores.47,48 Using published methods, we approximated SD from the inter-quartile range scores.54
Pooled outcome data
Walking
Two high-quality studies compared biomechanics during walking in patients undergoing PAO to asymptomatic participants.8,42 Meta-analysis was performed at the pre-op timepoint (Figure 2). Peak hip extension angle during walking was greater in asymptomatic participants (SMD 0.65; 95%CI 0.21 to 1.10). In one study, this difference remained six months post-PAO, but not at 12 months post-PAO.8 Observational designs were used which means these results provide low-level of evidence that asymptomatic participants demonstrate increased peak hip extension angle when walking compared to patients with DDH undergoing PAO.
The same two studies also showed a higher peak hip extension moment in asymptomatic participants compared to patients undergoing PAO (Figure 3).
Meta-analysis showed no other differences between asymptomatic participants and patients undergoing PAO, including walking speed (supplementary Appendix 2), walking peak hip flexion moment (supplementary Appendix 3) and walking flexion pull-off power (supplementary Appendix 4).
Hip Impingement Test
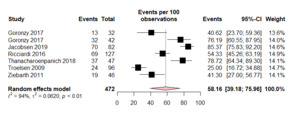
Six high-quality studies assessed the anterior hip impingement test.7,38,44,48,49,51 Prior to PAO, 58% (95% CI: 39% to 76%) of patients with DDH undergoing PAO had a positive hip impingement test (Figure 4). The result remained one to three years post-PAO (Figure 5).7,38 However, the proportion of positive impingement test reduced to 17% (11% to 24%) in patients five or more years after PAO (Figure 6).44,51 The results provided low-level of evidence that 58% of patients had a positive impingement test prior to and up to one to three years post-PAO with a reduction to 17% >5 years post-PAO.
Best evidence synthesis
Walking
When comparing patients pre-operative and 18-months post-PAO, Pedersen et al.39 found an increase in walking peak joint moment for extension (SPD 0.84; 95%CI 0.08 to 1.6) and flexion (0.91; 0.14 to 1.69), with no difference in peak hip joint extension angle (0.41; -0.27 to 1.09). Similar findings were reported by Jacobsen et al.,8 demonstrating increased peak hip flexion moment 12 months post-PAO compared to pre-PAO. One-year post-PAO, another high-quality study reported increased walking velocity (0.42; 0.02 to 0.81) and stride length (0.46; 0.06 to 0.85), with no difference in cadence (0.23; -0.15 to 0.61).50 These studies provide limited evidence that walking peak hip flexion and extension moment improved 18-months post-PAO, also at one-year post-PAO, walking velocity and stride length both increased, without change in cadence.
Hip Range of Motion
Hip flexion ROM
Four high-quality studies investigated pre- to post-PAO changes in hip flexion ROM.38,41,48,52 Maldonado et al.52 found a reduction at minimum five years post-PAO (SPD -0.71; 95%CI -1.26 to -0.16), as did Ziebarth et al.55 three years post-PAO (-0.5; -0.83 to -0.16). Data from Novais et al.41 was not estimable but, also favoured reduced hip flexion ROM three years post-PAO, whilst Ricciardi et al.48 found no difference when comparing pre- to six-month post-PAO changes (-0.39; -0.88 to 0.11). These studies provided limited evidence of reduced hip flexion ROM following PAO.
Two high-quality studies compared hip flexion ROM between groups of variable DDH depending on their LCEA, pre-operatively.40,47 Ricciardi et al.47 found no difference in hip flexion between patients with mild and severe DDH (SMD -0.09; 95% CI -0.62 to 0.43). When dividing patients into three groups (mild, moderate, severe), Fabricant et al.40 also found no differences in hip flexion ROM. These two studies provide moderate evidence that hip flexion ROM is not different in patients with variable degree of DDH, as defined by the LCEA. One high-quality study provided limited evidence that hip flexion ROM was not different between males and females with DDH (0.7; 0.34 to 1.05).22
Hip internal rotation ROM
Four high-quality studies compared hip internal rotation ROM pre- and post-PAO.38,41,48,52 Maldonado et al.52 found no difference at minimum five years post-PAO (SPD -1.09; 95%CI -1.71 to 0.47) as did Ricciardi et al.48 at six-months post-PAO when measured in flexion (0.04; -0.45 to 0.53) and extension (0.2; -0.3 to 0.69). However, three years post-PAO, Ziebarth et al.38 found less internal rotation ROM when measured in flexion (-0.37; -0.7 to -0.04), this was also reported by Novais et al.,41 however, data was not estimable. These studies provided conflicting evidence that hip internal rotation ROM was reduced following PAO.
Two high-quality studies compared hip internal rotation ROM in patients with DDH grouped by their LCEA, pre-PAO.40,47 Ricciardi et al.47 found no differences between patients with mild and severe DDH when internal rotation ROM was measured in either flexion (SMD 0.0; 95%CI -0.52 to 0.52) or extension (0.08; -.63 to 0.48). When dividing patients into three groups (mild, moderate, severe), Fabricant et al.40 found no increased internal rotation ROM in flexion in patients with severe compared to moderate DDH (-0.07; -0.22 to 0.09). Also, no difference between mild and severe or moderate, nor any of the groups when internal rotation ROM was measured in extension.40 These two studies provide conflicting evidence that hip internal rotation ROM is different in patients with variable degrees of DDH, as defined by the LCEA.
Hip external rotation ROM
Three high-quality studies compared hip external rotation ROM pre- and post-PAO.41,48,52 Maldonado et al.52 reported a reduction in external rotation ROM at minimum five years post-PAO (SPD -0.58; 95% CI -1.11 to -0.05). Six months post-PAO, Ricciardi et al.48 found no differences when external rotation was measured in flexion (-0.13; -0.65 to 0.4) or extension (0.4; -0.96 to 0.16). Data from Novais et al.41 was not estimable, however, three years post-PAO, the results favored an increase in external rotation when measured in flexion, and a decrease when measured in extension. These studies provided conflicting evidence that hip external rotation ROM was changed following PAO.
Two high-quality studies compared hip external rotation ROM between patients pre-PAO surgery grouped depending on their LCEA.40,47 Ricciardi et al.47 found no difference between people with mild and severe DDH when external rotation ROM was measured in either flexion (SMD -0.13; 95%CI -0.65 to 0.4) or extension (-0.4; -0.96 to 0.16). When dividing patients into three groups (mild, moderate, severe), Fabricant et al.40 found reduced external rotation ROM when measured in extension in patients with severe compared to mild DDH (-0.33; -0.49 to -0.18), and severe compared to moderate DDH (-0.20; -0.36 to -0.04). The study found no difference between mild and moderate DDH when external rotation was measured in extension (-0.13; -0.27 to 0.01), or between any of the groups when external ROM was measured in flexion. These two studies provided conflicting evidence that hip external rotation ROM is different in patients with variable degree of DDH, as defined by the LCEA.
Hip abduction ROM
Three high-quality studies compared hip abduction ROM pre- and post-PAO.38,41,52 Maldonado et al.52 found no difference at a minimum five years post-PAO (SPD -1.47; 95%CI -2.18 to 0.76). Ziebarth et al.38 found a decrease in abduction ROM three years post PAO (-0.41; -0.74 to -0.08). Data from Novais et al.41 was not estimable but favoured a decrease in abduction three years post PAO. These studies provided conflicting evidence that hip abduction ROM changed following PAO.
Two high-quality studies compared hip abduction ROM between groups of variable DDH depending on their LCEA, pre-PAO.40,47 Ricciardi et al.47 found no difference between patients with mild and severe DDH (SMD -0.27; 95%CI -0.81 to 0.26). When dividing patients into three groups (mild, moderate, severe), Fabricant et al.40 also found no difference in hip abduction ROM. These two studies provided moderate evidence that hip abduction ROM is not different in those with variable degrees of DDH, as defined by the LCEA.
When dividing patients with DDH into three groups (mild, moderate, severe), Fabricant et al.40 found significantly increased hip adduction ROM in those with severe versus mild DDH (SMD 0.26; 95%CI 0.1 to 0.41). No difference was found between patients with severe compared to moderate DDH (0.12; -0.04 to 0.28) or moderate compared to mild DDH (0.13; -0.01 to 0.27). This study provided limited evidence that patients with severe DDH had increased hip adduction ROM compared to those with mild DDH, as defined by the LCEA.
Hip muscle strength
Four studies assessed strength as an outcome measure.25,37,43,53 Two studies likely used the same cohort of patients,25,37 the data from the older study was not estimable and therefore only results from the more recent study were used.25 De La Rocha et al.43 compared patients undergoing PAO who had undergone previous pelvic surgery with patients who had not.
The high-quality study by Sucato et al.25 provided limited evidence that hip abduction strength was unchanged one (SPD 0.07; 95%CI -0.35 to 0.48) and two years post-PAO (0.36; -0.07 to 0.79). Another high-quality study by De La Rocha et al.43 compared patients undergoing PAO with who had other previous pelvic surgery to patients who had not had any other previous pelvic surgery. The results of the study provided limited evidence that no differences in hip abduction strength existed pre-PAO (0.59; -0.19 to 1.38). However, six months (0.86; 0.05 to 1.67) and one-year post-PAO (1.03; 0.02 to 1.85), patients with no previous pelvic surgery had higher hip abduction strength compared to patients with previous pelvic surgery.
Sucato et al.25 provided limited evidence that there was no change in hip flexion strength one-year (SPD -0.22; 95%CI -0.65 to 0.20) and two years post-PAO compared to pre-PAO (0.03; -0.38 to 0.45). De La Rocha et al.43 provided limited evidence that compared to patients with previous pelvic surgery, patients without previous pelvic surgery (i.e. PAO as their first pelvic surgical procedure) were stronger in hip flexion pre-PAO (1.03; 0.21 to 1.86) and one-year post-PAO (1.04; 0.22 to 1.87), but not six months post-PAO (0.7; -0.1 to 1.49).
Mortensen et al.53 compared strength in affected and non-affected limbs pre-PAO, isometrically and isokinetically (concentric and eccentric) in hip flexion and extension. No differences were found isometrically (SMD -0.07; 95% -0.76 to 0.62), concentrically (-0.14; 0.84 to 0.57) or eccentrically (-0.07; -0.78 to 0.63). The authors also compared hip extension strength in affected with non-affected limbs.53 No differences were found isometrically (-0.25; -0.95 to 0.44), concentrically (0.13; 0.57 to 0.84) or eccentrically (-0.03; -0.74 to 0.67) between limbs. This study provides limited evidence of no differences in hip extension strength between affected and non-affected limb in patients pre-PAO.
Hip muscle-tendon pain
In one high-quality study by Jacobsen et al.,7 muscle-tendon pain in the hip and groin region was assessed clinically pre- and one-year post-PAO. Iliopsoas- (SPD -32%; 95%CI -46 to -17%) and abductor-related pain (-22%; -36% to -8%) decreased from pre- to post-PAO. No changes were found for adductor- (-5%; -16% to 6%), hamstring- (-5%; -12% to 2%) or rectus-abdominus-related pain (-4%; -9% to 2%). This study provided limited evidence that iliopsoas- and abductor-related pain decreased one-year post-PAO.
Functional tasks
Scott et al.17 found better performance in functional tasks in asymptomatic participants compared to symptomatic patients undergoing PAO. This study provided limited evidence that asymptomatic participants were faster in timed stair ascent (SMD -1.44; 95%CI -2.11 to -0.78), five sit-to-stands (-1.33;-1.98 to -0.68) and four-square step test (-0.64; -1.24 to -0.04), compared to patients undergoing PAO for DDH.
Running
One high-quality study by Jacobsen et al.8 provided limited evidence comparing running in patients undergoing PAO with asymptomatic participants. Asymptomatic participants ran faster (SMD -0.57; 95%CI -1.10 to -0.03) and had higher peak hip joint extension moment (-0.58; -1.12 to -0.05), but no differences existed for peak hip joint extension angle (-0.31; -0.84 to 0.22) and peak hip joint flexion moment (-0.74; -1.0 to 0.07).
DISCUSSION
This systematic review aimed to investigate physical impairments in adults undergoing PAO for DDH. Prior to PAO, there was low level of evidence that people with DDH had (i) reduced peak hip extension angle, (ii) reduced peak hip extension moment, and (iii) reduced peak hip flexion moment, during walking, compared to asymptomatic participants. One year following PAO there were no longer differences in walking between the groups. A positive hip impingement test was found in 58% of patients with DDH both pre-operatively and at 1-3 years post-PAO, then from 5-years onwards this reduced to 17%. Best evidence synthesis of non-pooled data revealed limited evidence of reduced hip flexion ROM, but conflicting evidence for internal and external rotation ROM, following PAO. There was limited evidence demonstrating no change in hip abduction or hip flexion strength following PAO. There was also limited evidence to support poorer running and functional task performance in symptomatic patients undergoing PAO compared to asymptomatic participants.
Limited evidence was found that patients with DDH walk faster, with a longer stride length 12-18 months post-PAO compared to pre-PAO, with larger peak hip joint extension and flexion moments. Clinically, reduced peak hip extension angle during walking pre-PAO likely reflects an avoidance of terminal extension, which appears to be restored post-operatively. Compared to asymptomatic participants, patients undergoing PAO did not run as fast and had a reduced peak hip extension moment in running. These findings suggest adaptations occur in people with DDH in both walking and running, seen as reduced speed, hip extension angle, and hip extension and flexion moments. Reduced anterior acetabular coverage commonly associated with DDH may contribute to less stability and/or apprehension when the hip moves into end range extension.56 These adaptations may represent an attempt to minimize apprehension by generating less force through the hip joint42 and/or reduce stress on painful anterior structures. Painful structures could include the iliopsoas muscle which sits immediately anteriorly to the hip joint and has been found to be painful in almost half of people with DDH pre-PAO7 and/or the anterosuperior aspect of the hip capsule and labrum which have been found to have dense nociceptive innervation.57 Future studies need to confirm whether these changes can be modified, and whether improvements in these impairments are related to improvements in pain and the progression to hip OA and total hip joint replacement.
This systematic review examined clinical outcomes including hip muscle strength, hip joint ROM, and functional performance. People with DDH are commonly considered to have increased hip joint ROM.58 The finding that hip flexion ROM is reduced following PAO is likely the result of improved femoral head coverage by the acetabulum. Hip muscle strength was found not to change following PAO, despite improvements in walking. In contrast, the results of a recent study (published after our data collection) showed improved isometric hip flexion and abduction strength one-year post-PAO compared to pre-PAO in 82 patients with DDH.59 The variation in findings may exist due to the low power of included studies, as the study populations were below 30 patients,25,53,60 whereas paired analyses were done in 82 patients with DDH in the study by Jacobsen.59 Also, of relevance, an included study in this systematic review, showed that strength increases in pre-PAO patients with a resistance training program.53 This study found that progressive resistance training was safe and feasible in patients with DDH, and may improve pain, strength, and functional performance. A resistance training program is likely advantageous both before and after PAO, but further research is required in this space and should also compare the effect of PAO versus a resistance training program on hip strength in patients with DDH.
The hip anterior impingement test is also commonly known as the Flexion, Adduction, Internal Rotation (FADDIR or FADIR) test. The FADIR test is widely known as part of the criteria for diagnosing femoroacetabular impingement syndrome (FAIS),61 and a positive test may commonly lead a clinician toward this diagnosis in a young adult with hip pain. Our findings show that patients undergoing PAO for DDH have a positive ‘impingement’ test more often than not. Inaccurate and delayed diagnosis are common in those with DDH,62 and clinicians should recognize this as a common impairment finding in those with DDH.
Preliminary evidence from De La Rocha43 shows poorer hip abduction and hip flexion strength post-PAO in those who have had previous pelvic surgery, compared to those who have not had previous pelvic surgery. Performing a PAO for a patient who has residual DDH following previous pelvic surgery may be more difficult due to scarring from initial surgery and distorted anatomy.63 Patients with previous pelvic surgery undergoing PAO may not experience the same level of improvement as those without, modifying expectations in these patients may be warranted.
Limitations
This review has several limitations. There were no randomised controlled trials, and a large proportion of included studies were retrospective in design. This has potential for introducing selection, detection, and performance bias. Many included studies did not provide characteristics of patients lost to follow-up or report on the validity and reliability of the outcomes used. There was significant variability in the post-operative assessment timepoints, and the type of outcomes measures used which limited opportunities to perform meta-analysis. The above factors made it impossible to obtain findings with ‘high’ level evidence and certainty ratings. Prospective longitudinal cohort studies are vital to better understand what causes physical impairments in those with DDH undergoing PAO.
This review did not explore whether impairments seen post-PAO were related to common surgical complications that might impede physical performance, such as delayed bony union or neuropraxias. Future research should examine these outcomes, and their potential on physical performance post-PAO. This review also only investigated physical impairments in those who were awaiting, or had undergone, PAO surgery. Exploring outcomes in those with DDH who are not at this point, potentially earlier in the disease progression, should also be a focus of future research.
Conclusion
Prior to PAO, patients with DDH demonstrate physical impairments during walking, which improved from one-year after PAO. The majority of patients with DDH had a positive hip impingement test (58%) prior to PAO, and initially after PAO, this drops to 17% from 5-years onwards. Hip abduction and flexion strength did not change pre- to post-PAO. Clinicians should be aware that patients with DDH have physical impairments that should be considered pre- and post-PAO.
Conflicts of Interest
Prospero international prospective register of systematic reviews ID: CRD42020180571
The authors report no conflicts of interest.
_flow_diagram.png)




_flow_diagram.png)




