BACKGROUND AND PURPOSE
Valgus extension overload syndrome (VEOS) is a condition that results from impingement of the posteromedial tip of the olecranon process on the posteromedial wall of the olecranon fossa. VEOS is common among overhead athletes such as baseball pitchers. During pitching, the elbow is said to be exposed to angular velocities up to 3000°/sec1 with valgus forces of 64 Nm, during late cocking, and compressive forces of 500 N experienced at the lateral radiocapitellar joint as the elbow rapidly moves from 120° of flexion to 25° at ball release.2
In 20-120° of flexion, the anterior bundle of the ulnar collateral ligament (UCL) is the primary restraint to valgus forces, when the elbow is moving into extension. Repeated valgus forces upon the UCL can lead to micro instability, resulting in excessive stress where the posteromedial portion of the olecranon contacts the olecranon fossa. This stress can create osteochondritis dissecans (OCD) of the capitulum, UCL injuries, and pathology at the posteromedial compartment of the humeroulnar joint (i.e. osteophyte formation, olecranon stress fractures, chondromalacia).3
Osteochondritis dissecans occurs at the anterolateral or central capitulum almost exclusively, comprising 97.5% of OCD lesions of the elbow and is correlated with valgus stress and axial loading. Stable lesions (those with patency of the articular cartilage and subchondral bone) often respond well to conservative treatment. Unstable lesions typically require procedures such as osteochondral autograft transplantation (OAT) or internal fixation. Return to sport is extremely variable after surgery, ranging from 62-100%.4
Conservative treatment for associated UCL injury focuses on restoring glenohumeral internal rotation and strength of the axioscapular, rotator cuff, and flexor-pronator musculature.5 Should conservative intervention be unsuccessful, UCL reconstruction (Tommy John) surgery is preferred with an approximate 85% return to play for adolescent baseball players.6
Little is documented on conservative treatment for posteromedial impingement without frank compromise of the articular cartilage, subchondral bone, or UCL. Surgical outcomes for adolescents with posteromedial impingement has not been documented. In adults, surgical outcomes for posteromedial impingement are mixed, with greater success rates (72%) for those with isolated posteromedial compartment pathology7 compared to those with combined lesions or UCL insufficiency (42%).8 There have been no case reports of adolescent baseball players with persistent VEOS symptoms and difficulty returning to hitting. Therefore, the purpose of this case report is to describe a movement-focused examination and treatment strategy for such an individual, emphasizing the role of the physical therapist as a movement expert.
CASE DESCRIPTION
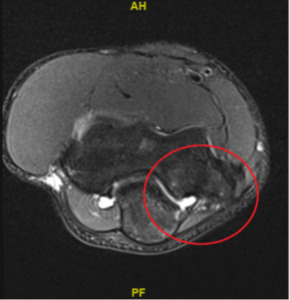
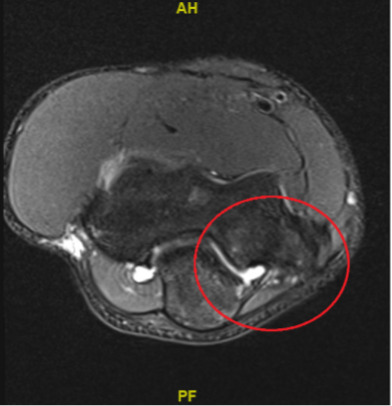
A 15-year-old right-handed male high school catcher presented to physical therapy with an approximate six-month history of medial elbow pain of gradual onset, having had an MRI with contrast (Figure 1). The accompanying radiologic report confirmed no presence of osteochondral lesion, fracture, or compromise of the anterior band of the ulnar collateral ligament. The report noted “marrow edema pattern of the distal humerus, medial epicondyle, olecranon, and proximal ulna involving the sublime tubercle and coronoid process most consistent with stress reaction in the setting of valgus extension overload.”
The subject denied a specific mechanism of injury, but reported a gradual increase with throwing, after which he began to experience “sharp” pain at the medial elbow with right-handed hitting. He initially underwent an initial set of six weeks (12 sessions) of physical therapy with another clinician at the same clinic, approximately three months after onset, consisting of forearm pronator strengthening at 90° of elbow flexion, scapular stabilizer, trunk, and sagittal plane lower extremity exercise (e.g. squats). Throwing improved significantly with treatment without any recurrence reported during follow-up with his orthopedic surgeon approximately 2.5 weeks after discharge. However, he reported a return of his medial elbow symptoms when resuming hitting.
He followed up with his hitting coach for several weeks, hitting off a tee, while continuing his home exercise program from previous physical therapy treatment. However, pain continued to persist with ball contact during hitting. He elected to take a break from throwing and hitting. He consulted his orthopedist, who referred him for further physical therapy. The subject of this case report was informed the data of this case would be submitted for publication and consented to the release of information.
EXAMINATION
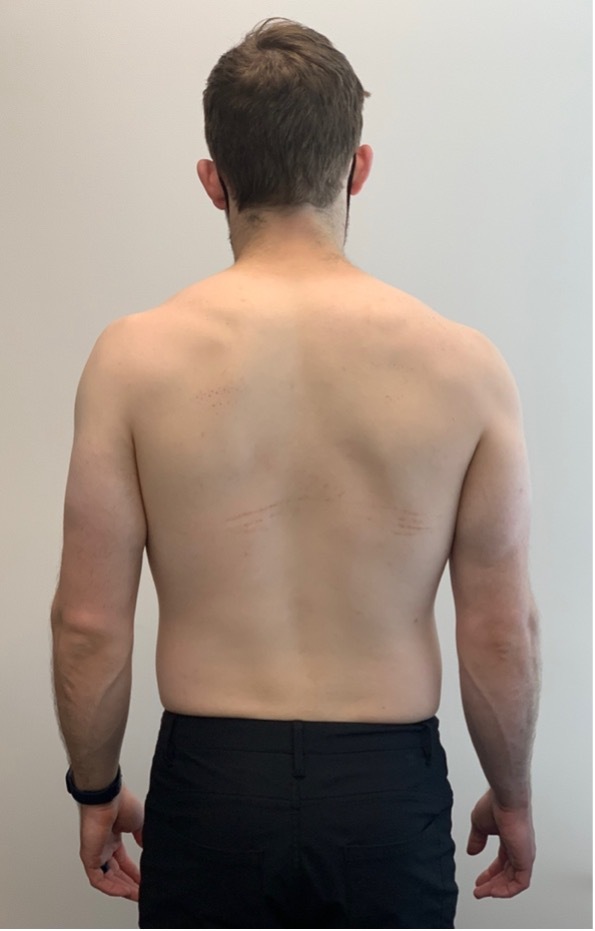
The subject was 5’10", weighing 155 lbs., with an ectomorphic body build. Subject’s static posture was significant for the discrepancy between the subject’s right humeral position in comparison to his scapula. The right scapula was relatively depressed and abducted in comparison to the left, which may have been expected given the subject’s right-hand dominance.9 However, despite greater right scapular internal rotation, the right humerus appeared to rest in greater external rotation and extension. The increased observed right scapular internal rotation suggested external humeral rotation was especially prevalent (Figure 2).10
Movement observation consisted of overhead elevation and simulation of subject’s hitting position in combination with single leg squat due to the gluteal demand required during optimal hitting.11 Overhead elevation demonstrated early right scapular upward rotation and greater internal rotation, a pattern associated with posterior shoulder mobility deficits.12 The subject’s hitting motion was simulated during the examination, with marked right humeral external rotation observed during the drive phase. The humeral alignment appeared to compensate for the expected forearm supination of the trailing upper extremity, with the medial and lateral epicondyle near-parallel to the predicted line of force that would occur during ball contact. Sudden valgus force applied to the elbow in this position to simulate sudden ball contact reproduced the subject’s symptoms. Manually internally rotating the humerus and then reapplying valgus force to the elbow made the motion pain free (Figure 3). No laxity was appreciated during valgus stress testing. At this point in the examination it was hypothesized the subject’s primary movement dysfunction was excessive humeral external rotation resulting in increased valgus force at the elbow on the trailing upper extremity during ball contact. Additional impairments that could contribute to the preference for this hitting strategy were also assessed.
Shoulder and elbow range of motion were evaluated. Primary deficits included loss of bilateral shoulder internal rotation, although significantly more limited on the right (L 30°, R 10°; measured at 90° of abduction). Although humeral retroversion is common in overhead athletes, the total arc of motion on the subject’s symptomatic side was 125°, well below previously established estimates (e.g. 160°).13 Forearm supination was more limited on the left (L 80°, R 90°), while pronation was more limited on the right (L 80°, R 60°).
Key muscles involved in scapulohumeral and elbow mechanics were tested (strength measures are noted in table) using manual muscle testing (MMT). The subject’s right serratus anterior, middle, and lower trapezius were graded equal or greater than the strength of the left. However, the subject’s humeral internal rotators including the subscapularis and pectoralis major were a full grade weaker (L 5/5, R 4/5). Muscles were all tested by the same examiner using MMT, which has been found to have acceptable intrarater reliability.14
Lower extremity and trunk movement patterns were also screened, as the gluteal and trunk musculature are crucial for force development during hitting. Rolling was chosen as a transverse plane trunk stability pattern based on prior implementation in athletes and the absence of an established gold standard assessment for transverse plane lumbopelvic control,15 which was symmetrical and negative for trunk and extremity dissociation. The single leg squat was chosen to functionally assess gluteal performance, as it has been shown to correlate to weakness of the hip extensors.16–18 Observational analysis during the single leg squat demonstrated greater hip adduction and internal rotation on the right.
ASSESSMENT
The subject demonstrated signs and symptoms consistent with valgus extension overload syndrome, confirmed on MRI and during physical examination. During both static standing and simulation of the batting position during the drive phase, the subject’s humerus (and therefore elbow joint) appeared to be in excessive external rotation. This external rotation appeared to be a significant contributor to the loads sustained at the right medial elbow. Symptom reproduction during the rapid applications of valgus force with complete resolution with medial rotation of the humerus assisted in confirming a movement diagnosis of excessive humeral external rotation and the interpretation of relevant impairments to kinesiopathology.
There exists a paucity of data regarding elbow forces sustained during hitting or ball contact during baseball. However, during a baseball swing, the rear forearm must supinate to optimize bat contact with a pitch while the elbow rapidly extends at approximately 1200 to 1500º/sec.19 If the humerus excessively externally rotates instead of forearm supination occurring, then the valgus moment at the humeroulnar joint significantly increases. Of significance was the subject’s posterior shoulder stiffness. During swing, the rear humerus horizontally adducts to make ball contact. Flexibility impairments of the posterior shoulder are more profound in horizontal adduction and would contribute to increased humeral external rotation during swing as the humerus adducts,20 driven by stiffness of the posterior cuff and external rotators.
Although very little is known about upper extremity muscle activation during baseball hitting, it is known key humeral internal rotators such as the pectoralis major and latissimus dorsi are active during ball contact.21 Strength has also been correlated to upper quarter alignment.22 The combination of excessive stiffness or shortness of the posterior shoulder with inadequate humeral internal rotator strength and activation during hitting would contribute to the excessively externally rotated humeral position and valgus stress at the elbow during ball contact. Although the lack of pronounced weakness (when tested via MMT) of the subject’s right scapular stabilizers and posterior cuff musculature was somewhat surprising, the subject had previously completed a six-week physical therapy program focused on improving strength of these muscle groups.
Signs of weakness of the right gluteus maximus (e.g., during MMT and single leg squat)16–18 were also thought to contribute to decreased pelvic rotation induced through the rear limb during the swing. This would result in a need for increased humeral horizontal adduction, placing further strain on the subject’s stiff and short posterior shoulder musculature and exacerbating humeral external rotation induced through the flexibility deficits of the posterior glenohumeral structures.
Although the subject’s supination range of motion was slightly greater on the right, this could be explained through decreased pronator teres strength, which would also contribute to decreased dynamic resistance to valgus force.23,24 The discrepancy between sides was minor and falls within the standard error of measure for goniometry at the elbow, which has been reported up to 11.5°.25 As several thousand pounds of force occur during bat ball contact,26 the primary focus of treatment was to prevent excessive humeral external rotation placing the coronal axis of the humeroulnar joint in-line with ball contact rather than attempting to improve dynamic elbow stability through pronator strength alone.
The above findings suggested a final movement diagnosis of excessive humeral external rotation contributing to the subject’s symptoms and limitations during baseball.
INTERVENTION
The treatment plan for this subject was focused on improving posterior shoulder flexibility, increasing strength and stiffness of the humeral medial rotators, and progressively integrating the concept of slightly increased humeral medial rotation into hitting maneuvers to decrease valgus stress at the medial elbow. The subject was provided insight regarding the underlying hypothesis and singular goal of treatment based on the excessive humeral external rotation movement diagnosis throughout the examination process. This was intended to empower him early on to correct any daily habits that may contribute to excessive humeral external rotation. Recent literature suggests in regard to rehabilitation, activity performance changes result in longer lasting and more meaningful change than exercise alone.27
Kinesiology tape was applied in a novel method, originating at the right medial antebrachial and elbow regions, and then spiraling proximally across the humerus to the right scapular region (Figure 4). The purpose of this taping was primarily to provide medial elbow support while reducing external humeral rotation throughout the day. Only one study has investigated the use of kinesiology tape for medial elbow pain,28 which improved forearm control over that of sham taping. However, multiple studies have found benefits for the use of kinesiology tape for treatment of lateral epicondylitis regarding decreasing pain and improving grip strength.28,29 Multiple authors have that found the direction of kinesiology tape does not change outcomes.30,31
Soft tissue mobilization to the posterior shoulder musculature was also performed early within treatment to improve the subject’s ability to perform humeral internal rotation exercise through a larger range. Soft tissue mobilization has been shown to improve posterior shoulder flexibility in multiple populations32,33 including baseball players. Humeral internal rotation at 90° of abduction improved 30° after a single session of soft tissue mobilization. The subject was instructed on self-soft tissue mobilization to preserve these gains, an intervention which has been shown to be effective at improving humeral internal rotation.34
Manual therapy was combined with exercises to decrease posterior shoulder stiffness while concurrently increasing humeral internal rotator strength and stiffness. Prone (Figure 5) and supine (Figure 6) humeral rotation exercise in 90° of abduction was prescribed. Rotation with the humerus in 90° of abduction has been found to result in a relatively high percentage of subscapularis activation.35
Supine shoulder internal rotation with a dumbbell was also prescribed to eccentrically activate the humeral external rotators (Figure 6). Eccentric exercise was chosen to decrease actual stiffness and shortness of the posterior shoulder contributing to inadequate humeral internal rotation, as this contraction type has been shown to add sarcomeres in series.36 Although very short-duration stretching programs may improve stretch tolerance and ROM, their effects on changing the actual biomechanical properties of tissues is still being investigated.37
Strengthening of the pectoralis major and forearm pronators was also performed. The subject stood with a heavy band anchored to the side, while he horizontally adducted the humerus and pronated the forearm against resistance (Figure 7). The subject was cued to avoid internally rotating the scapula during this exercise to impart a stretch to the posterior shoulder. This exercise was aimed to optimize posterior shoulder flexibility by allowing the subject to assume a humeral position nearly identical to an across body stretch position38 while maximizing force generation of the pectoralis major.39
As the subject advanced, neuromuscular reeducation during gripping was added to train the subject to allow for forearm supination without compensatory external rotation of the humerus (Figure 8). A two-pound bar was used, which the subject could simulate using his aluminum bat. The subject stood with the humerus flexed to 90° and observed his cubital fossa. He was instructed to grip the “bat” and then first rotate his humerus medially. He then rotated the “bat” outward, ensuring he did not also externally rotate the humerus during forearm supination. This was aimed to both teach control of the humerus during horizontally adducted positions that would be required during batting while also activating the flexor-pronator forearm musculature to assist in providing dynamic stability against elbow valgus.24,40
Integration of the gluteal musculature in a transverse pattern using a heavy resistance band was prescribed to improve pelvic and trunk rotation during batting, therefore reducing the requisite amount of horizontal humeral adduction (and therefore decreasing posterior shoulder flexibility demands that could induce external humeral rotation), during this movement. It is important to note the subject reported an improvement in symptoms prior to any specific intervention to address the trunk and pelvis, which were implemented at visit 4. The specific effect of the lower limbs on shoulder and elbow positioning and force are not well studied. However, it is known that the gluteus maximus is active during the earlier portions of swing41 and that pelvic rotation is crucial for generating force to achieve ball contact.42
The subject’s daily activities and existing exercise regimen were reviewed and modified to augment gains from the above program. For example, bench pressing was modified with cueing to adduct the scapula and avoid scapular protraction during the concentric phase of the press (Figure 9). This position would not only encourage humeral horizontal adduction for high-load pectoralis major activation, but also contribute to stretch of the posterior shoulder musculature under load. Exercises such as Pallof pressing were integrated into the subject’s standard gym routine to optimize transverse plane trunk stability while also encouraging humeral horizontal adduction for posterior shoulder flexibility.
After this time, focus was placed on returning to hitting while the subject continued the above exercises. Interval return to sport programs exist as suggested by Reinold et al.42 as well as return to hitting suggested by Monti in 2015.43 Similar guidelines were utilized for this subject’s return to sport. Return to hitting was conducted in three phases; hitting from a tee, soft toss, then from a pitch at moderate effort behind L-screen in batting cage. Swings were complete at subject perceived effort of 75-80%. Each phase consisted of progressive swing repetitions with at least 1 day rest in between to assess tolerance. The subject remained at one step in each phase until he could bat without symptoms before progressing, a similar methodology to those utilized in previously established return to play interval programs.
Two drills also were performed to specifically address the trailing elbow position to improve maintenance of the elbow posterior to the knob of the bat, and therefore to decrease the magnitude of external rotation of the humerus and during the acceleration and follow through phases of the bat swing.43 During the first drill, a 10 lbs. dumbbell was utilized while the subject moved the weight through the 1st half of the swing with an isometric hold at what would be the contact point of the swing (Figure 10). The second drill was completed with a PVC pipe, maintaining the same position as the first drill with the isometric hold, then carrying out the remainder of the swing (Figure 11). Video analysis with the subject’s phone was utilized as biofeedback.
OUTCOMES
After four physical therapy sessions, the subject had returned to practice and resumed all throwing activities. He denied any recurrence of symptoms with throwing and humeral internal rotation PROM at 90° of abduction had improved from 10° to 30°. After 9 physical therapy sessions, he reported a 100% alleviation of symptoms with hitting. At the conclusion of physical therapy treatment, he continued to be able to throw without any limitations and had returned to hitting from live arm without pain at full effort. Follow-up via phone at seven months after discharge revealed that the subject had returned to play at full-capacity without any symptom recurrence.
DISCUSSION
The subject presented to physical therapy with chronic medial elbow pain and confirmed MRI evidence of VEOS. Although he noted mild symptoms with throwing, he reported his primary aggravating activity was hitting. He had participated in 12 physical therapy sessions earlier during the year including traditional scapular stabilizer strengthening exercises (e.g. shoulder taps, Ys and Ts), but had experienced a recurrence of symptoms upon return to hitting. After completing nine physical therapy visits over five weeks, he was able to return to all activities such as hitting without any pain.
Regional interdependence has been discussed for two decades44,45 and adapted to encompass the general interactions between various physiologic systems.46 The prevalence of scapular dysfunction in overhead athletes47 and comprehensive rehabilitation programs for the elbow that include exercises for the rotator cuff, lower and middle trapezius, and serratus anterior48 may contribute to a profession-wide assumption that these exercises will address the underlying movement problems in this population.
This case exemplifies the importance of a systematic movement examination and assessment of potential relevant contributing impairments for individuals who do not fall in the majority regarding common movement dysfunctions that lead to a given condition. For example, the subject did not present with any findings suggestive of remarkable scapular stabilizer (serratus anterior, middle, and lower trapezius) weakness or dyskinesis49 that could contribute to his elbow dysfunction. Grip strength, tested to determine function of the medial elbow stabilizers such as the flexor digitorum superficialis and profundus measured at 100-110 lbs. of force (symmetrical between hands) in multiple positions and elbow angles, well above the 75th percentile for a 15 year-old male.50 The subject had previously participated in a strengthening program consisting of exercises to address the scapular and medial elbow stabilizers with little success, and thus determining an underlying aberrant movement cause of continued pain was the focus upon the subject’s return to physical therapy.
Although medial elbow pain in relation to throwing is relatively well researched,51,52 there exists a paucity of literature regarding its incidence with hitting. Furthermore, unlike throwing, the contribution of the lower extremities,53 trunk,54,55 the scapula,56 and the humerus57 to forces at the elbow during hitting have not been studied. Dissimilar to pitching, batting is a reactive movement pattern that changes significantly in response to the pitcher.58–60 This makes the study of an optimal movement pattern for batting difficult, as multiple strategies may be ideal based on the location and velocity of the ball.
However, the general phases of batting have been well-defined43,61 and include preparatory, stance, stride, drive, bat acceleration, and follow-through phases.43 The preparatory phase describes the initial batting stance preferred by each hitter. This transitions into the stance phase, during which the batter lifts their front leg, shifting their weight to the rear leg while coiling their trunk and upper extremities in reverse of the pitcher. This coiling continues as the batter then brings the front leg forward (stride phase) and then makes lead leg contact with the ground (drive phase). During drive phase, maximal energy storage is achieved through a further 12° of reverse arm motion.43 At the end of the drive phase, the trailing elbow should be flexed with the shoulder adducted. The goal of these initial phases is to capitalize on the stretch-shortening cycle to generate optimal force during the swing. This kinetic energy is transferred during the bat acceleration phase through rapid uncoiling beginning at the lower extremities, and then transitioning to the pelvis, trunk, shoulder, and elbows.61 The final follow-through phase allows the batter to optimize pelvic rotation.
The moment of ball contact during the bat acceleration phase in relationship to the subject’s pattern of humeral rotation is of specific relevance to this case. Bat velocity is assisted through rapid elbow extension just prior to ball contact, previously estimated at 948º/sec.61 The rapid elbow extension to accelerate the bat combined with excessive humeral external rotation would increase valgus force on ball contact and replicate forces that occur during VEOS often seen in pitchers.62
Based on these phases of batting, a reasonable comprehension of movement requirements (e.g. rapid pelvic rotation, rear upper extremity horizontal adduction, rapid elbow extension) can be established by a physical therapist and systematically tested. The importance of beginning a physical examination with movement observation and tests confirming specific hypotheses of an underlying movement cause cannot be overstated. For example, for this subject, excessive right humeral external rotation was noted both at rest and with functional movements. The valgus stress test was positive for symptom reproduction when the subject replicated upper extremity position simulating ball contact and rapid valgus force was applied manually by the physical therapist. This test was implemented to simulate forces experienced by the subject during ball contact.
The hypothesis that excessive humeral external rotation was resulting in the subject’s pain and pathology viewed on MRI was supported by then manually rotating the humerus into slightly greater internal rotation and repeating the same valgus stress test. For many subjects, multiple movements that are symptom provoking could be used with systematic modification of the movement to establish a pattern suggesting an underlying movement dysfunction. This is analogous to prior research that has found a battery of tests in physical examination is generally more useful in establishing a diagnosis than a single test.63,64
Impairments were then systematically assessed based on the movement diagnosis and movement observations. Factors relevant to their contribution to excessive humeral external rotation with batting were examined. For example, inadequate participation or stiffness of the humeral internal rotators such as the subscapularis, pectoralis major, and latissimus dorsi, or excessive stiffness of the humeral external rotators (especially those which would be placed in tension with forward humeral flexion) could contribute to the subject’s preferred but painful hitting strategy. These impairments were all tested based on the initial standing static postural, movement, and functional testing examination. For example, during forward reaching and shoulder elevation, excessive early scapular upward rotation was noted. This is a pattern suggestive of inadequate mobility of the glenohumeral joint12 and therefore, posterior shoulder stiffness contributing to excessive humeral external rotation was hypothesized to be a relevant contributing factor to the movement syndrome. This was then tested in more isolation during measures such as humeral internal rotation mobility and palpation to the posterior shoulder musculature. Using this strategy, the clinician was able to systematically establish relevant impairments to the subject’s movement dysfunction.
This case exemplifies the unique role of physical therapists as movement experts who are well equipped to address specific kinesiopathology based on physical examination. Although the profession has more recently transitioned to various classification models that match intervention to specific presentations in regions such as the lumbar spine,65 programs in the upper quarter trend toward consistently addressing the rotator cuff and axioscapular musculature.48,66 The prevalence of scapular dysfunction in overhead athletes47 and comprehensive rehabilitation programs for the elbow that include exercises for the rotator cuff, lower and middle trapezius, and serratus anterior48 may contribute to the assumption that these exercises are beneficial for all subjects with elbow or shoulder movement conditions. For the above subject, previous treatment including traditional scapular stabilization exercise was not effective in reducing his symptoms upon return to hitting, suggesting the importance of customizing intervention to specific patterns of movement dysfunction.
LIMITATIONS
The presented case report has notable limitations, including the inability to generalize and non-experimental nature of this study. Furthermore, due to a lack of normative data regarding humeroulnar rotation during batting and subject privacy logistics, actual video analysis of upper quarter position throughout the hitting maneuver was not obtained. Pelvic and lower quarter normative data exist for batting,61,67 and therefore video analysis may have revealed whether the integration of specific pelvic and trunk retraining during physical therapy was actually needed. Additionally, certain physical examination measures such as manual muscle testing in the shoulder possess questionable interrater reliability and reproducibility68 and should be interpreted with caution.
CONCLUSIONS
This case report exemplifies the importance of a systematic movement examination to establish an underlying movement diagnosis with which to efficiently guide treatment. The subject presented with continued signs of VEOS and limitations with baseball batting despite prior participation in physical therapy including exercises typically cited in a regional interdependence model. A systematic evaluation established an atypical movement diagnosis of excessive humeral external rotation contributing to valgus force during ball contact. This diagnosis guided all subsequent intervention. After nine physical therapy visits over five weeks, the subject was able to return to soft toss hitting, confirming a 100% return to play without recurrence at seven month follow-up. These outcomes demonstrate the successful implementation of a movement-based intervention program. Furthermore, they imply the importance of a specific application of human movement knowledge rather than generally implementing the concept of regional interdependence.
Disclosures
The authors of this case report have no conflicts of interest.

_vs._painless_varus_stress_test_(right)_with_a_red.png)








_vs._painless_varus_stress_test_(right)_with_a_red.png)







