INTRODUCTION
The patellofemoral joint (PFJ) consists of the posterior patella and the distal femur. The joint is widely studied due to the high prevalence of patellofemoral pain. While the etiology of patellofemoral pain (PFP) is multifactorial, patellar malalignment has been identified as one of the possible causes.1,2 The patella achieves the greatest stability beyond 45° knee flexion, where it is fully engaged in the trochlear groove.3 The joint capsule, patellofemoral ligament, iliotibial tract (ITB), and lateral patellar retinaculum all help to maintain the stability of the PFJ.4 Surrounding muscles, especially the distal portion of the vastus medialis, i.e., the vastus medialis obliquus, are important in the dynamic stability of the joint.5 Weakness or damage to these stabilizing structures may lead to patellar displacement,6 and hence, to patellofemoral pain.7
Ultrasound (US) is an inexpensive and non-invasive imaging modality that has been widely used to investigate the knee joint.8–12 Results have been found to be consistent, and valid in comparison with magnetic resonance imaging (MRI).10 Ultrasound has also been found to be accurate and reliable when investigating patellar abnormalities13 and diagnosing fractures.14,15
Previous real time US studies on asymptomatic subjects have shown that 20° hip adduction results in lateral displacement of the patella, compared to the neutral position.9,12 Although the results in these studies were statistically significant, the validity of the US method in assessing patellar position in relation to hip adduction was not reported. Consequently, it cannot be guaranteed that the patellar position measured by US was equivalent to the results that would have been obtained by direct measurement.
The aim of this study, therefore, was to validate the use of US to measure lateral displacement of the patella, by comparing the position of the patella as measured by US, and then by direct measurement.
MATERIALS AND METHODS
Nine soft-fixed cadavers (1 male, 8 females) donated for anatomical education and research under the UK Human Tissue Act (2004) were used in this study. Soft-fixed cadavers retain free movement of the joints and preserve a more life-like appearance. The mean age was 82.4± 6.02 years (range: 71-90). None of the cadavers had any noticeable lower limb pathology or deformity, and cause of death was unrelated to musculoskeletal pathology. However, three limbs had to be excluded from the study due to previous dissections of the knee area.
A SonoSite Edge II ultrasound machine (SonoSite, Bothell, USA) with a SonoSite HL50x 15-6MHz linear-array probe (6 cm) was used for US imaging. The cadaver was positioned in the anatomical position with a block under the knee to maintain 20° flexion.9,12 The borders of the patella were palpated. The width and height were measured with a digital caliper, then a vertical line was drawn between the superior and inferior borders, and a horizontal line was drawn between the medial and lateral borders. The anterior superior iliac spine (ASIS) was palpated, and a steel ruler was placed on the cadaver, with one end on top of the ASIS and the other end on the mid-point of the patella. A straight line was then drawn from the mid-point of the patella to the ASIS. A standard 360° goniometer was used to position the lower limb. One arm of the goniometer was aligned with the left and right ASIS, while the other was aligned with the line drawn from the mid-point of the patella to the ASIS. Initial measurements were taken in the neutral position. The limb was then moved into 20° adduction and maintained in position using a block.
Ultrasound Protocol
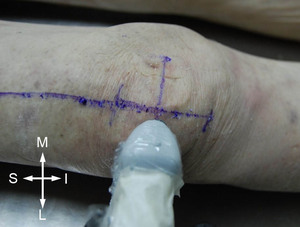
The ultrasound probe was covered with cling film for hygiene purposes. Water-soluble transmission gel was placed between the scanner head and the cling film, and on the skin of the knee. It has been shown that this method does not affect the measurements or the physical characteristics of the probe.16 The probe was positioned perpendicular to the skin, on the lateral side of the knee, in line with the previously marked horizontal line (Figure 1).
Minimal pressure was applied when placing the probe on the subject, sufficient to obtain a clear image without distorting the image or displacing the patella. Brightness mode (B-mode) real-time ultrasonography was then used to measure the patella-condyle distance in the neutral position and in 20° adduction (Figure 2). Three measurements were taken for each position. To minimize operator variability, all measurements were taken by the same operator, who had received US training from the Clinical Physics Department of the institution.
Direct Measurement Protocol
Following ultrasound measurement, a scalpel was used to make a small, superficial, skin incision between the lateral condyle of the femur and the lateral edge of the patella along the previous marked transverse line. Care was taken not to incise deeper than the superficial fascia. A self-retaining retractor was used to maximize visualization and access to the area. A digital caliper (resolution of 0.01 mm) was used to measure the patella-condyle distance at the apex of the lateral margin of the patella and the superior apex of the lateral femoral condyle (Figure 3). A measurement was first taken in the neutral position, then in 20° adduction. Again, three sets of measurements were taken in each position.
Intra-rater reliability study
One subject was randomly selected for an intra-rater reliability study. This subject’s knees were assessed nine times over three different days for both US and DM measurements. All measurements were taken by the same investigator, using the same equipment, in order to standardize measurements.
Statistical Analysis
Measurements obtained were analyzed using Microsoft Excel. A paired t-test was used, with the significance set at p<0.05. Data points were plotted on a scatter graph, and the Pearson correlation and the coefficient of determination R² were calculated. A two-sample t-test was used to compare results obtained in this study with data previously reported from an ultrasound study on young, asymptomatic volunteers.12 Intra-rater reliability was assessed using the coefficient of variation (CV) and variance.
RESULTS
A total of 15 lower limbs from nine soft-fixed cadavers were examined. The mean and variance of the 3 repeated measurements for both methods showed close similarity, with low CV and variance (Tables 1 and 2).
The mean difference between the neutral and adducted positions in both left and right limbs combined was 0.24 cm. A paired t-test showed no significant difference in the measurements taken from the two different methods (p=0.83). A strong correlation between the methods was found (Pearson correlation=0.97, R²=0.9446) showing that the measurements obtained with US were valid and reliable (Figure 4). A two-sample t-test using the data reported here (mean difference 0.24 cm) compared to previously published ultrasound data obtained from an asymptomatic, in-vivo population (mean difference 0.18 cm)12 showed no significant differences between the mean patellar-condyle distance in the neutral and adducted positions, indicating that the data obtained from soft-fixed cadavers were comparable to that of a patient population.
The coefficient of variability (CV) for the intra-rater reliability test was 0.008 (0.8%) for US measurements and 0.045 (4.5%) for direct measurements in the neutral position; and 0.0057 (0.57%) and 0.003 (0.3%), respectively, in 20° adduction. These values were all <5%, indicating that the results were reliable.
DISCUSSION
Ultrasound has previously been used to evaluate patellar position,8–12 morphology,13 and fractures.15 However, the validity of the US method in assessing patellar position was not reported, and hence, it has not been confirmed that US is a reliable method of assessment of patellar position in comparison with direct measurement. It is important, therefore, to validate the methodology before its application in vivo to subjects in research, or in the clinic. This study fills the gap in the literature by comparing ultrasound results with direct measurements. It has previously been shown that good quality US images can be obtained from soft-fixed cadavers,6 therefore, this type of cadaver was used in this study.
To the authors’ knowledge, the study reported here is the first to demonstrate, by direct measurement, the validity of using US to measure the position of the patella in the neutral position and then in 20° of passive adduction. The current results showed a very small mean difference between the US measurement and the direct measurement (0.02 cm in the neutral position and 0.05 cm in 20° hip adduction, respectively), suggesting that the two methods produce very similar results. There was also a high level of correlation between the two methods (R²=0.9446, Pearson correlation=0.97), and there was no statistically significant difference in the results obtained (p=0.83). Therefore, the US technique used to measure patellar position is valid and can be used with confidence in clinical assessment of the position of the patella.
For both US and direct measurement, the intra-rater reliability test showed that the CV was <5%, which indicates that the results were reliable. The standard deviation (SD) of the US measurement and direct measurement was 0.01 and 0.06, respectively, in the neutral position, and 0.006 and 0.003, respectively, in hip adduction. The low SD also suggests that the measurements were reliable, and unlikely to be due to measurement errors.
It was found that in both US measurements and direct measurements (DM), hip adduction consistently produced a smaller patella-condyle distance than in the neutral position, and caused lateral displacement of the patella. The mean difference obtained by US and DM was 0.24 and 0.25, respectively. This is consistent with the in vivo study carried out by Herrington and Law,9 where 12 healthy males were recruited, and Kwan et al.'s study of a larger cohort of both males and females.12
While axial x-ray or CT images are currently used clinically to assess patellar tilt,17 real time US of lateral patellar displacement as described by Herrington et al.9 and Kwan et al.12 may present a potential alternative modality that could be easily applied in the clinic, although, since this was a cadaver study, more work will be necessary to validate the method in symptomatic patients.
Although the current results have shown US to be a valid method for measuring patellar position relative to the femoral condyle, some limitations must be taken into consideration. The sample size was relatively small, and the use of cadavers imposed its own limitations, as preserved tissue may not be completely comparable to living tissue. Also, the mean age of the cadavers was 82.4 ± 6.02 years, so it is likely that osteoarthritis, which affects more than 80% of the aged population,18 was present, which could have affected the results. Out of the nine cadavers used, eight were female, which may also have skewed the results. Although limbs with obvious damage or pathology were excluded, there is a possibility that the subjects had underlying knee or hip pathology that was not detected. Unfortunately, the donors’ medical records were not available, so the reliability of the results reported here could be compromised. However, the mean difference from both methods between the neutral and adducted positions recorded here (0.24 cm), is similar to the in vivo result (0.18 cm) reported in a much larger study of young, asymptomatic subjects,12 and furthermore, data analysis suggested that the results reported here are not significantly different. It should, however, also be borne in mind that these measurements were all non-weight-bearing and carried out after passive movement of the limb, so any direct comparison with patellar displacement in a living, weight-bearing subject should be treated with caution.
Conclusion
This study shows a high level of correlation between US and direct measurement of the position of the patella in neutral and adducted hip positions. This suggests that US is a valid method of assessing lateral displacement of the patella in vivo.
Conflict of Interest Statement
The authors confirm that they have no conflicts of interest to declare. The study was internally funded by St George’s, University of London
Acknowledgements
The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind’s overall knowledge that can then improve patient care. Therefore, these donors and their families deserve our highest gratitude.


_and_direct_meas.png)



_and_direct_meas.png)