INTRODUCTION
The SARS-CoV-2 coronavirus and COVID-19 pandemic reached epic proportions at the start of the Spring and Summer sports seasons in 2020. In attempts to limit the spread of disease, intermediate schools, high schools, and colleges across the United States transitioned to remote learning strategies and suspended any formal interscholastic sports activities and extracurricular events.
The Center for Disease Control recommends that children participate in at least 60 minutes of vigorous activity daily.1 The maintenance of fitness and skill development is crucial for sports performance and injury risk reduction.2 However, in the Fall of 2020, six months following the sports shutdown, only 14 US states allowed full Fall sports participation, while the remaining states permitted either modified or no athletics due to the COVID-19 restrictions.3 Prolonged decreases in physical activity levels can result in adverse physiological consequences across multiple body systems, including the cardiovascular, respiratory, musculoskeletal, and endocrine systems.2 Recent evidence further highlight the adverse psychological consequences associated with the COVID -19 restrictions in both adult and youth athlete populations.4–6 Thus, enriching athlete motivation and adherence to prescribed training programs are of utmost importance to maintain physical activity, enhance emotional and mental health, and decrease injury risk.7 Currently, there is limited understanding of how youth athletes train while away from the traditional team environment during the COVID-19 sports interruption.
Additionally, the specific factors that increased motivation to maintain physical fitness and athletic performance during this time are currently unknown. This study aimed to determine the extent to which athletes maintained their training levels during the COVID-19 pandemic and understand the strategies that enhanced motivation and adherence to a training regimen while in physical isolation. A secondary aim was to further understand how youth athletes returned to activity and identify any secondary effects of the prolonged sports interruption as they resumed athletic activities.
METHODS
A team of two physical therapists and two orthopedic surgeons specializing in the treatment of youth athletes developed a two-part electronic survey in REDCap, hosted by The Children’s Hospital of Philadelphia. The initial survey aimed to determine activity changes, the current level of organized instruction, and athlete preferences for ongoing training support during the pandemic-related stoppage of in-person sports activity in the spring/summer of 2020. The initial survey contained six components: eligibility screening, general and sports demographics, current and previous training volumes, type of instruction received, individual training preferences, and perceptions of a future return to activity (Appendix A). After sports activities had resumed, a follow-up survey was distributed to the same cohort to understand athlete perceptions and experiences of sports resumption after the prolonged period of forced reduction in team-based activities (Appendix B).
The development of each survey instrument followed a similar process. Initial development identified key topics and consensus regarding survey structure and question format. The survey was pilot-tested and refined after consultation with a small group of youth athletes representing the population of interest. The final surveys consisted of multiple-choice questions and took approximately four to six minutes to complete.
To be eligible for this study, subjects needed to be between 14 and 21 years old and actively engaged in competitive sports at the onset of the pandemic-restricted in-person sports activities. The initial survey was distributed directly to athletes by email, using a snowball sampling methodology starting with the primary team of authors’ personal, professional, and community connections. The survey period began in June 2020 and remained open for eight weeks. The secondary survey was distributed in October 2020 to those individuals who consented to follow-up questioning while completing the initial survey. The subjects received a single email invitation and one reminder email to complete the follow-up survey. This survey remained open for a period of four weeks. This study was reviewed and approved by the Institutional Review Board at The Children’s Hospital of Philadelphia.
RESULTS
Initial Survey
The survey was accessed a total of 266 times. Ninety-eight individuals accessed the survey consent and/or eligibility screening portions but did not complete the survey. Thus, a total of 168 subjects met eligibility and were included in Phase I of this study. The mean age of the sample was 16.3 ± 2.1 years. Subjects were 62% female, predominantly white (95%), and mainly from Pennsylvania (54%), New Jersey (19%), and New York (10%). While subjects reported participating in a total of 22 different sports, the majority of subjects participated in soccer (38%), lacrosse (20%), and track and field (17%) (Table 1).
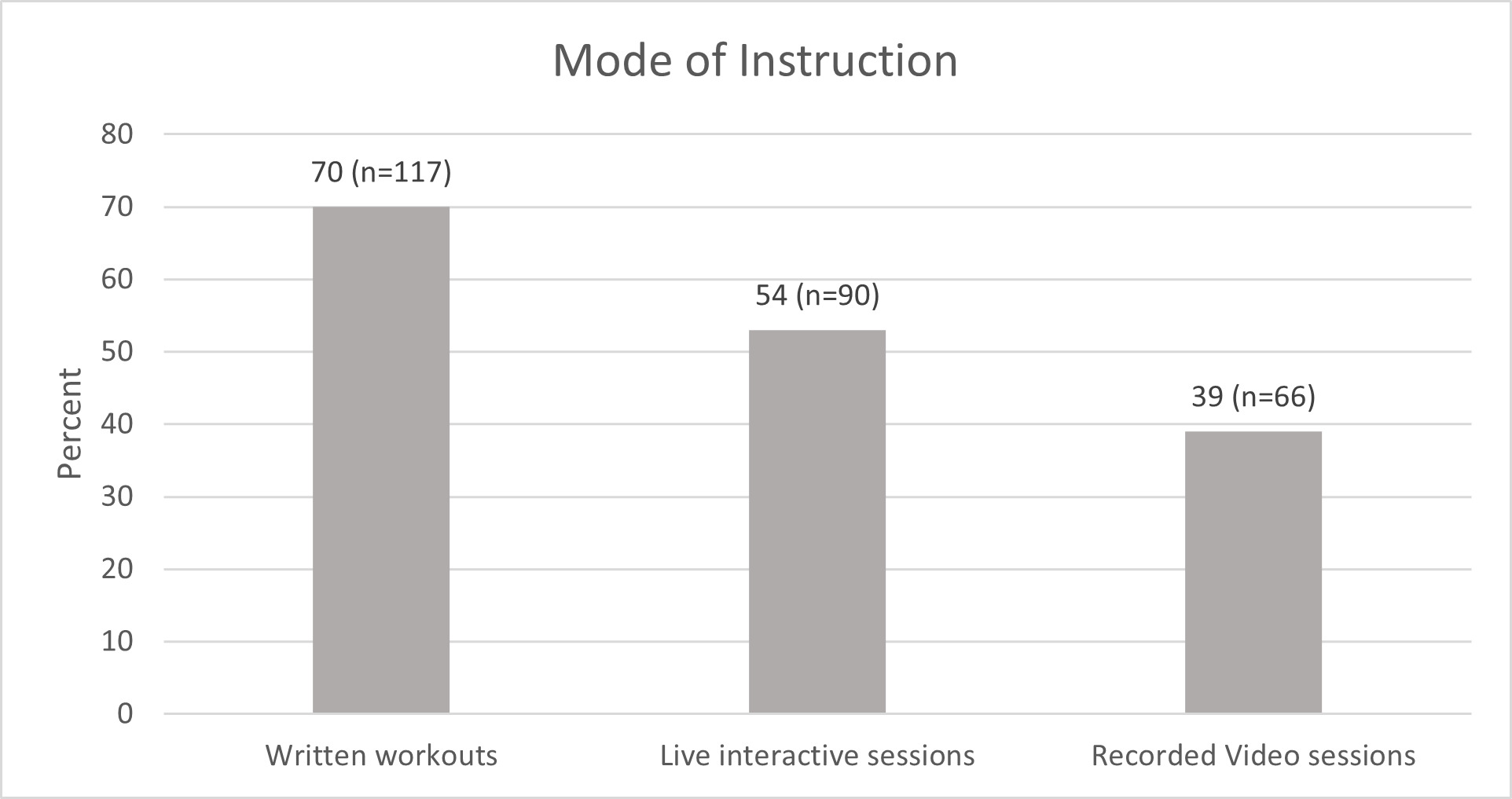
Nearly all (98%) of subjects reported that in-person practices and sports-related activities were canceled due to the COVID-19 pandemic. Most athletes (86%) reported receiving sports-related training instructions from their coaching or training staff during this time. Written workouts represented the most common method of instruction (70%). However, “live” online sessions via Zoom or similar platforms represented 53% of instructions, and pre-recorded videos accessed through YouTube or other platforms were also commonly utilized modes (33%) (Figure 1). A large proportion of athletes (73%) reported supplementing team-based training recommendations with individually designed workouts, most frequently jogging (62%), strength training (54%), and sports-specific drills (51%). Despite team-based training suggestions and individual supplemental workouts, only 21% of the sample reported their weekly training hours remained similar to their pre-pandemic levels. Most subjects (67%) reported a decrease in their overall weekly training volumes, with 40% of athletes reporting their training volumes decreased by more than half of their pre-pandemic levels. Along with reduced training volumes, many youth athletes (40%) indicated they would not feel physically prepared to resume in-person sports-related activities.
Improving athletic skill and performance was the primary motivator (66%) to independently train while not participating in in-person activities, followed by being healthy (50%), and improving their physical appearance (30%). Interestingly, a small number of athletes indicated they trained due to coaches’ (18%) or parents’ (6%) expectations.
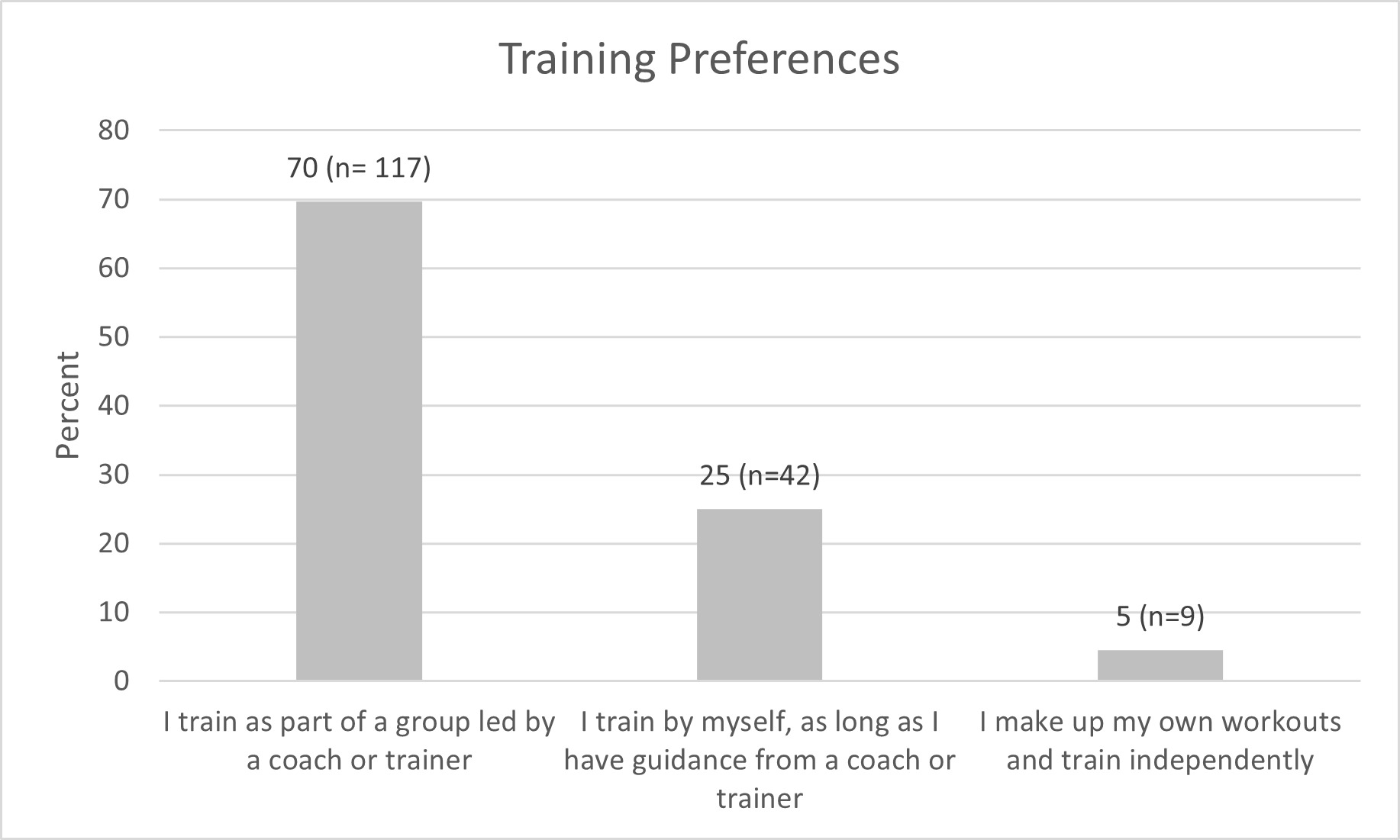
When asked about their preferred remote training methods, a large majority of athletes felt their performance was best when training in an online “live” group setting led by a coach or trainer (70%). Only a small subset of athletes felt at their best while training with a written-guided workout (25%) or independently designing their workouts (5%) (Figure 2).
Follow-up Survey
One hundred forty-four subjects indicated consent to participate in Phase II of this study. A total of 49 subjects (response rate 34%) accessed the follow-up survey. Six athletes had not resumed in-person sports activities yet, leaving 43 subjects who completed the follow-up survey.
The demographics and subject characteristics were similar between the initial and secondary survey participants (Table 1). A majority of athletes felt either moderately (60%) or extremely prepared (21%) for in-person sports activities. Approximately 30% of athletes reported initially resuming in-person activities with more than one sports team. When practices initially resumed, athletes indicated a nearly even split of practice frequency between 1-2 days per week (35%), 3-4 days per week (30%), and 5-7 days per week (35%), however at the time of survey completion, the frequency of practices increased to 5-7 days per week for 63% of the sample (Figure 3). Despite this increase in practice frequency, 63% of the sample reported they still supplemented team-based practices with jogging (51%), sports-specific skill work (47%), and strength training (40%) on an individual basis. A return to competitive game activities was reported to occur within the first month of resuming in-person practices for 34% of the sample.
Since the resumption of in-person sports activity, 28% of the sample reported experiencing “aches or pains that limited their ability to participate in sports.” Notably, nearly 25% of the sample reported they sustained an injury requiring them to visit a doctor, urgent care, or another medical provider, with muscle strains (70%) and torn ligaments (20%) making up most of the diagnoses.
DISCUSSION
Infection mitigation precautions adopted in response to the COVID-19 pandemic created a rapid change in the sports environment for youth athletes. The results of this study are the first to present specific information related to activity changes, athlete perception of training effectiveness, and self-reported injuries during the period of organized sports restriction and following return to in-person sports activities.
There was a substantial reduction in youth athlete training and sports conditioning amidst COVID-19-related sports restrictions, with nearly 40% of the sample reporting participating in less than half of pre-pandemic weekly hours of sports activity. These data expand upon previously published reports demonstrating decreased physical activity due to social distancing prevention protocols in response to the COVID-19 pandemic across various populations. The reduction in training volumes experienced during the pandemic poses an interesting situation. Excessive sports volumes, competition congestion, and limited rest intervals have all been suggestive of creating an increased risk of musculoskeletal injury in youth athletes.8,9 Therefore, the reduction in training volume brought about by the pandemic may have served as a much-needed break from sports-specific training for these young athletes. This suggestion is further supported by data from a multi-center study finding a decrease in sports-related musculoskeletal injuries amongst youth athletes during the COVID-19 pandemic.10 Though this change in activity may have been protective in the short term, these behaviors may become problematic as COVID-related sports restrictions decline. While this survey cannot quantify specific relationships between acute and chronic workloads, the subjects indicated a significant decrease in overall training hours during socially distant sports protocols, followed by a rapid resumption of in-person athletic activity (Figure 3). In addition, approximately 30% of subjects reported immediately returning to play for more than one sports team, which may contribute to overall increased sports-related workloads. Several studies have demonstrated an increased risk of injury with acute spikes or rapid alterations in an athlete’s acute workload compared to their chronic workloads and current fitness levels.11–13 This concept may help explain why 25% of the sample required medical attention for an injury within a mean time of 79 days after resuming in-person sports activity. While a small number of follow-up respondents limits the strength of these conclusions, these findings are consistent with previous studies that found an increased rate of injuries and earlier time to injury within older groups of athletes upon returning to competitive sports after COVID-related sports interruptions.14–16 Though it is unknown whether maintenance of physical activity workloads during time away from organized sports could have mitigated this injury risk, future studies should seek to evaluate these factors more specifically. This information could help inform more effective youth fitness programs during ongoing and future pandemic mitigation strategies. These findings may also inform coaches, parents, athletes, and healthcare practitioners about injury prevention efforts after a prolonged absence from team-based sports activity, such as after recovering from significant injury, surgery, or other circumstances necessitating a particularly inactive period between sports seasons.
In addition to the potential role in mitigating injury risk, the direct relationship between physical activity and mental health is well established.17–19 Recent studies have highlighted the adverse consequences on mental health and quality of life for youth athletes during this pandemic.6,20,21 Collectively, the data from the current study and these previous reports highlight the relationship between exercise and training in maintaining an athlete’s physical and psychological well-being.
To maximize youth athlete compliance with recommended training activities, athlete preferences of instruction mode should be considered. While coaches and training staff attempted to maintain physical activity using various methods, the primary means was via written handouts. While this instruction method offers several benefits regarding ease of administration and adaptability, it did not match athlete preferences for virtual “live” or recorded instruction. Exercise instruction that matches athlete or patient preferences may improve maintenance of physical activity through enhanced motivation and exercise participation. Issues of compliance with recommended physical activity levels or home-exercise prescriptions are problematic amongst healthy and injured populations.22 Inadequate exercise amongst children may contribute to sub-optimal athletic performance and future health consequences.7,23 Thus, the utilization of effective and motivational exercise communication strategies should be of high priority. Previous studies have shown improved compliance to prescribed exercises using video-based exercise instruction.24,25 Youth athletes in the current world are technologically savvy and highly digitally connected through smartphones and other devices and, not surprisingly, indicated a preference for synchronous and asynchronous web-based exercise instruction. In addition, youth athletes indicated they were most motivated to exercise or train to improve their athletic performance and health. Though future studies examining instruction mode on compliance are needed, coaches, healthcare practitioners, and other sports-related professionals should consider employing the more preferred video-based exercise instruction.
Approximately 75% of youth athletes indicated they supplemented coach-supplied training instructions with independent workouts during the forced hiatus of in-person activities. While this was not unexpected, the authors found it surprising that 63% of athletes continued to supplement in-person sports with their routines once in-person activities had resumed. Coaches and medical staff typically base exercise or training volume progression decisions on the assumption that they understand their athletes’ current training volumes. The data from this survey suggests that a large proportion of youth athletes are pursuing further training than what is provided during monitored training sessions. Medical staff and coaches should consider questioning their athletes about independent training habits or use automated technology-based workload monitoring methods to understand their athletes’ training habits more accurately. This information would help guide prescriptive workload decisions and may help reduce the potential for overuse injuries among youth athletes.
Limitations
There are several limitations to this study that should be recognized. The survey questionnaires were not previously validated, and although efforts were made to ensure clarity and accurate interpretation during development and pilot testing, individual variations in the interpretation of questions may exist. Nearly all of the sample came from the Northeastern United States and were predominately white; thus, the results of this study may not be generalizable to a broader population. The sample size for the follow-up survey was smaller than the original survey and may create bias thus, the results of the follow-up survey should be taken with caution. Finally, the snowball, electronic sampling methodology could have led to a sampling bias by sharing this survey within groups of athletes with similar social, demographic, or physical characteristics, which may limit the generalizability of these results.
CONCLUSION
In-person sports activity restrictions brought about by the mitigation efforts to reduce the spread of Covid-19 created an acute decrease in youth athlete training and exercise volumes. Athletes preferred using online video platforms to engage in remote training instruction. Though most athletes supplemented training activities with individualized training, many significantly declined physical activity during the time of pandemic-related sports restrictions. These reported changes in training habits and volumes may have contributed to a high injury rate among study participants following the resumption of organized sports activities. By understanding youth athlete training preferences, the results of this study can help professionals working with youth athletes maximize compliance with home-based exercise instruction, enhance youth physical fitness, and mitigate the adverse physical and psychological health sequelae of inactivity.
Conflict of Interest Statement
We, the authors, affirm that we have no financial or commercial affiliations related to the performance or outcome of this manuscript.
Grant Support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
IRB Statement
Institutional Review Board of The Children’s Hospital of Philadelphia approved this study. Protocol #: 20-017595


_of_participants_during_the_covid-19_sports_shutdown_and_follow.png)
_of_participants_during_the_covid-19_sports_shutdown_and_follow.png)