Introduction
The World Health Organization Physical Activity Action Plan identifies that sport is an underutilized, yet important, physical activity contributor.1 However, sport participation has inherent injury risk,2,3 with 30% of all emergency department visits due to sport injury.4 Injury rates continue to rise, with a 35% increase in female soccer anterior cruciate ligament tears over 25 years.3 The rise in injury rates suggest that current approaches to estimating injury risk and risk management are not effective.5 One factor limiting progress is the inconsistency in screening, risk assessment, and risk management strategies to guide injury mitigation approaches. For example, individual potential risk factors are often times preemptively deemed important in all sport sub populations, when in reality, additional larger and repeated studies are needed to understand the generalizability of a specific risk factor.5 This spuriously concludes a ‘catch all’ risk factor at all competition levels, when this specific risk factor may only be influential in a sub-population, or worse, demonstrate no actual risk due to influence from another confounding variable, providing biased injury risk results.5,6
In order to improve our understanding of injury risk, and move towards effective injury mitigation in sport physical therapists and clinical researchers must apply lessons from other healthcare professions. One medical disease that has steadily demonstrated improved patient outcomes is breast cancer.7–9 The inclusion of both modifiable and non-modifiable factors when assessing risk,10,11 the transition to personalized medicine,10,12,13 and the systematic approach used to investigate individual risk factors14 have created a system that can be replicated in other fields of medicine. Therefore, the purpose of this commentary is to describe breast cancer risk research and risk management strategies and how these strategies can be implemented in sport, using baseball as a practical example, to improve athlete outcomes.
Current State of Baseball Injury Burden and Research
One sport that is highly researched for injury risk is baseball.15–18 A 2019 scoping review reported that 678 studies focused on baseball research.19 Baseball is played throughout the world, with 160 countries associated with the World Baseball and Softball Federation.20 Over 16 million people participate in baseball within the United States alone, with professional leagues throughout Australasia, Latin America, and North America.20,21 Baseball is considered a relatively safe sport but injury rates have more than doubled over the last two decades.15,17,22,23 Injury incidence ranges from 0.8 to 4.0 injuries per 1,000 athlete exposures.24–31 with the greatest incidence attributed to the shoulder,15,23 elbow,17,23,32 and trunk,23 with throwing overuse injuries being the most common.25,33 The number of injuries is greater compared to other throwing sports.28,29,31 Baseball players have a greater risk of injury (1.7 times greater odds) compared to softball players, and pitchers with a 4.57 greater odds compared to position players.29 Injury burden is high, with time loss, replacement, and health care costs continuing to rise at all baseball levels.34 The escalation in frequency,2,3,7,21,23,33–35 severity,28,29,36 and cost34 of injuries in baseball suggests that the approaches to understanding and preventing baseball injuries are not effective.
The available empirical evidence has identified only a fraction of the complex interactions of risk factors in baseball.19,37 A primary limitation of current baseball research is that there are no prospective studies examining multiple intrinsic and extrinsic risk factors to inform injury prevention programs. Previous studies do not control for non-modifiable confounders that can act as effect modifiers changing the impact of the study variables on the ultimate outcome .15,35,38,39 Further, the focus of previous research has often been on one specific physical factor in isolation,15–18 without attempting to control for or understand its relation to other modifiable and non-modifiable confounders. Therefore, the complex interaction of multiple risk factors and injury mechanisms are unclear and inhibit clinical examination, prevention strategies, and clinical decision making.
Improvement in Breast Cancer Outcomes, Personalized Risk Assessment, and Management
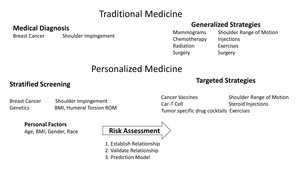
Breast cancer mortality has consistently decreased over the last 30 years,7,8 largely attributed to advances in personalizing the prevention and treatment strategies which include modifiable and non-modifiable factors when assessing risk,10,11,40 the transition to personalized medicine,10,12,13 and the systematic approach used to investigate individual risk factors (Figure 1).14 These key steps have seen decreased breast cancer mortality rates by 6.9% from 2002 to 2006 alone, with an average of a 2% decrease per year in Europe.41 Within the United States, breast cancer mortality has decreased by 38% from 1990-2003.9 These reductions in mortality trends have been observed across all age groups,9,41 and particularly in younger women.9
Besides advances in surgical42 and chemotherapy treatments,43 the improvements in breast cancer survival have been attributed to innovations in breast cancer screening, risk assessment, and risk management.10,12,13 Risk assessment is defined as a, “systematic approach to characterizing adverse exposures.”44,45 While risk management is defined as selecting strategies to reduce risk of the outcome.44 In order to improve attributable risk identification and management, the United States Preventive Services Task Force in 2009 changed their breast cancer mammography screening guidelines, stating, “screening should be an individual one and take into account patient context, including the patient’s values regarding specific benefits and harms (pg. 294).”46 These alterations were implemented due to specific changes in understanding of breast cancer risk, particularly in the advent of personalized medicine.
Personalized medicine is defined as when medical treatment is customized for an individual patient.47 Within breast cancer, personalized medicine has been implemented due to the understanding and inclusion of both modifiable and non-modifiable risk factors when assessing outcome risk. For example, the advent of genetic research, specifically investigations of the BRCA1 & BRCA2 genes and single nucleotide polymorphisms (SNPS),12,13 and their relationships to breast cancer have created a better understanding of non-modifiable risk.10,11 The inclusion of non-modifiable risk factors helps guide shared decision making between the clinician and patient on screening strategies and potential primary and secondary risk management approaches for modifiable factors.10 For example, if the 10-year breast cancer risk is higher for a specific 40-year-old, compared to the average 50-year-old, it may be advantageous to begin mammogram breast cancer screening 10 years prior to the nationally recommended screening age.10 The understanding of non-modifiable risk may also inform how intervening on modifiable risk factors will change breast cancer risk. Modifiable breast cancer risk factors include changes in weight after the individual reaches 18 years old to present age, physical activity habits, nutrition, and alcohol consumption.11,48 A clinician can calculate if intervening on these modifiable risk factors (through educational, lifestyle, and medical interventions), changes a particular patient’s breast cancer risk. This information helps apprise the clinician on the cost benefit of different screening measures (such as MRI versus traditional mammogram), the potential intensity and adherence needed to focus on modifiable risk factor interventions, and potential educational counselling on false positive tests (in case increased screening is required) to create a more individualized tailored medical approach.10,48
Application in Sport, Using Baseball as the Example
So far, we have briefly highlighted screening, risk assessment, and management strategies in breast cancer. The question of how this applies to sport, which does not deal with life and death, but at worst, career ending injuries needs to be answered? Currently, baseball injury risk and risk management does not account for non-modifiable risk factors, and assumes equal risk between all populations and subgroups. Within breast cancer, a systematic approach has been proposed to investigate potential risk factors and incorporate these risk factors into one comprehensive risk assessment.14 This systematic approach can be used as a template for improving baseball outcomes and more generally in sport.
Three critical phases have facilitated the identification and importance of individual risk factors and developing targeted, personalized strategies for breast cancer risk.14 First, level one studies establish the potential relationship(s) between factors and outcomes of interest, which generates future, testable hypotheses. These studies identify statistical relationships between a potential risk factor and the outcome, without controlling for confounders. Baseball research remains at this level. Level two studies prospectively investigate the strength and direction of the relationship between the risk factor and outcome, while controlling for confounding. These studies can also investigate potential sub group relationship differences between the risk factor and outcome. Within baseball, this is the next logical step in risk factor research and can be easily implemented through replicating past study designs and cohorts, while controlling for confounders. Level three studies can entail prediction model development and validation studies seeking to understand if intervening on a factor alters prognosis.14 Within baseball, randomized control trials on modifiable risk factors and the development and validation of prediction models is warranted to better calculate injury risk and improve risk management.
To use a hypothetical example for context, a clinician scientist wants to understand if shoulder range of motion is a risk factor for arm injuries in baseball pitchers. To initially investigate this issue, this clinician scientist performed a level one retrospective cohort study, in which shoulder range of motion was compared between injured and non-injured baseball pitchers. The clinician scientist could perform an analysis of variance (ANOVA) or a logistic regression to ascertain if there are differences in shoulder range of motion between injured and non-injured baseball players. In this hypothetical example, a 20º difference in total shoulder rotation (external plus internal shoulder rotation) was observed between injured and non-injured pitchers, which is beyond the standard error of measure and minimum clinically importance difference.49 From these findings, the clinician scientist surmises that shoulder range of motion might be an injury risk factor in baseball pitchers. However, the clinician scientist knows there are specific biases that need to be controlled for in order to help understand if this is truly a risk factor
Following the level one study results, the researcher decided to perform a level two prospective study on shoulder range of motion. Shoulder range of motion was measured in spring training, along with potential confounders, including hand dominance, body mass index,50 injury history,51 shoulder strength,52 lower extremity range of motion,53 balance,32,35 and pitch velocity.54 Each pitcher was followed for the entire season with injuries and total athlete exposures (in the form of pitching appearances and number of pitches) collected. The clinician scientist then performs a Cox survival analysis or a relative risk regression to compare injured versus non-injured pitchers. The clinician scientist also performs sub group analyses for left and right handers, as these sub populations have demonstrated different clinical phenotypes, including demonstrating different height,55 mass,50 humeral torsion,56,57 and pitch velocity.58 The clinician scientist observed that there is still a difference in total shoulder rotation between injured and non-injured pitchers, which after controlling for all confounders, is 12º. Further when analyzing left and right handers separately, left handers demonstrated a 9º difference and right handers demonstrated a 15º difference. These differences between left and right handers were beyond the standard error of measure and thus suggests there may be clinical differences in shoulder rotation injury risk between hand dominance. The clinician scientist hypothesizes that shoulder range of motion can be used to help ascertain injury risk and should be intervened upon. However, before interventions can be recommended, these risk factor needs to be assessed for efficacy in relation to modifiable and non-modifiable risk factors, and if there is a causal relationship between shoulder range of motion and injury. Examples of a non-modifiable risk factors include age, humeral torsion,56,57 and previous arm surgical history.
To answer these level three questions, the clinician scientist performs a multiyear prospective study, including both modifiable and non-modifiable risk factors, to develop a prediction model. The developed prediction model demonstrated good prediction performance following best practice guidelines and improved with the inclusion of shoulder range of motion as a predictor.59 The clinician scientist then performs a clustered randomized control trial performing manual therapy to the shoulder in the treatment arm and standard care (not including manual therapy) performed in the control arm for an entire season. The research determines that there is a 30% reduction in arm injuries in the treatment arm compared to the control arm. When assessing the intervention effectiveness in left and right handers, it is observed that left handers demonstrated a 20% reduction in injury rates and right handers a 40% reduction in injury rates. The clinician scientist concludes that intervening on this modifiable risk factor, using the prediction model to identify pitchers at risk for injury, can help decrease arm injury risk in pitchers. Further, modifying shoulder range of motion has different injury risk management effectiveness (20% difference) between left and right handers.
How Current Injury Risk and Management is Employed in Sport and is Suboptimal
The proposed approach is not reflected in the current state and progression and sport injury risk screening, assessment and intervention strategies. To use a baseball clinical example, current best evidence-based practice suggests that baseball pitchers are at a higher risk for injury when a pitcher’s dominant (throwing) shoulder total range of motion is 10º less than the non-dominant (non-throwing) shoulder.17,60 Current clinical decisions would recommend that this at-risk pitcher would receive specific shoulder range of motion interventions (such as stretching and manual therapy), until the pitcher’s dominant shoulder total range of motion was below 10º different than their non-dominant shoulder.61 The current best practice recommendation implies that this will effectively mitigate this particular pitcher’s injury risk through this specific intervention. A current limitation with this approach includes assuming that all populations and subgroups demonstrate a similar risk relationship between the proposed risk factor and injury. Further, it is ambiguous if this particular injury risk would be managed through this intervention, due to lack of specific understanding as to how this particular risk factor relates to other modifiable and nonmodifiable risk factors and if there is a causal relationship between shoulder range of motion deficits and arm injuries in baseball pitchers.
The sports medicine and research community could gain insight from the lessons learned and implemented in breast cancer. These experiences could help improve a particular pitcher’s current injury risk assessment and allow for personalized interventions. Improved injury risk assessment would be ascertained by accounting for non-modifiable risk factors such as the pitcher’s injury history,51 previous pitching exposure,62 pitching mechanics,37 and osseous adaptation.63 Understanding how these non-modifiable risk factors interplay with the modifiable shoulder range of motion risk factor,17,60 along with other modifiable risk factors such as shoulder strength52 and balance,32,35 could be enhanced though controlling for confounders in prospective injury risk studies from previous level one studies. Development of an injury prediction model would be a logical progression within the tiered level three study paradigm. This information could then be used in shared decision making between the clinician and athlete concerning risk management. Specifically, calculating current injury risk could determine if individualized screening schedules throughout the season are warranted, beyond the traditional preseason screening. One could also calculate only non-modifiable injury risk, which would illuminate how intervening on all modifiable risk factors would potentially impact risk mitigation strategies. Another option would be to calculate the influence of each intervention on the athlete’s injury risk, providing a better plan for creating a personalized approach to their risk management.
These are only a few of the potential next steps that could improve sport injury research and inform clinical practice across body regions, specific injuries, and athlete groups. It should be noted that current practice suggests taking detailed patient histories should be followed by performing a thorough and comprehensive physical exam. However, each of these pieces are not amalgamated into one comprehensive injury risk assessment nor risk management strategies (such as understanding casual factors or a comprehensive prediction model), and considered in isolation from a risk assessment and management perspective. Learning and implementing lessons from medical research and services for diseases such as breast cancer, would only improve patient care in the sports medicine setting.
Conclusion
Current research, athlete screening, risk assessment, and risk management are ineffective in sport, demonstrated by the continued rise in injury rates and severity over the last twenty years.15,17,22,23 As demonstrated through breast cancer screening strategies,10,11,48 an improved understanding of risk is not ascertained without the inclusion of both modifiable and non-modifiable risk factors. Until the sport community applies the lessons learned from other health care professions, sport injury outcomes will be suboptimal, continuing to provide a disservice to athletes.