INTRODUCTION
Concussion is a mild traumatic brain injury. Concussion occurs as a result of direct trauma, whiplash, or blast injury that causes the brain to move forward and backward. Symptoms associated with concussion include headache, dizziness, vertigo, nausea, fatigue, light and noise sensitivity, as well as altered mental status.1,2 The leading cause of head injury in adults occurs from car accidents, whereas in the younger population (15-24 years old), injury occurs from a sport related accident. Of the forty-four million children involved in various sports-related activities, around 3.8 million experience a concussion related to sport each year.2 Emergency department visits due to sport-related concussions increased by more than double between 2001-2012.1,3 The most common cause of sport-related concussion is player to player contact and happens frequently in football and ice hockey. Female athletes have a higher incidence of concussion compared to male athletes. Athletes who have had a prior concussion also have a higher rate of experiencing additional concussions.2,4 Adolescent athletes are at higher risk of suffering a concussion than adults and may also require a longer period of time to recover.5 If an athlete is diagnosed with a concussion, they must be cleared by a health care professional before returning to play.
Traditional treatment for concussion includes physical and cognitive rest.6,7 Unfortunately, individuals prescribed with rest can demonstrate withdrawal from life activities, deconditioning, and mental health issues.8 Research is emerging that shows the benefit of exercise and early physical activity after a concussion.2 Specifically, early physical activity is advantageous and lower rates of post-concussive symptoms are associated with higher levels of physical activity and this research states that patients suffering from concussion should be encouraged to exercise as tolerated 1-2 days after concussion and initial rest.2 Individuals with a concussion present with varying symptoms and presentations requiring patient-specific intervention strategies. According to a clinical practice guideline, recommended frequency, intensity, timing, and type(s) of intervention is dependent on the severity of a patient’s concussion, their level of irritability, and how they respond to treatment. Patients should also be educated on symptom reporting so that interventions can be adjusted resulting in earlier return to sport.9
Existing literature suggests that cervical and vestibular interventions as well as sub-symptom threshold exercise may be beneficial for individuals 24-48, hours after concussion. Aerobic exercise has been shown to improve autonomic nervous system function suggesting that sub-threshold exercise treatment could be a beneficial treatment for concussion. Systematic reviews have shown that exercise post-concussion can improve symptom scores after concussion and that sub-symptomatic aerobic exercise programs can be more effective in reducing post-concussion syndrome symptoms than traditional standard of care.10
There is a gap in the current literature regarding sports-related concussions in adolescent and young adult athletes and the appropriate interventions for treatment. The aim of this systematic review was to investigate the effectiveness of physical therapy interventions for adolescent and young adult athletes post-concussion.
METHODS
This systematic review was registered with Prospero and completed using guidelines from Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA). PRISMA is a 27-item checklist based on evidence that focuses on reporting the impact of interventions in systematic reviews and meta-analysis.11 Prospero provides the opportunity to determine if a similar review already exists or is in the process of being published to prevent unwanted duplication.12 The registration ID for Prospero for this systematic review is CRD42021256465.
Eligibility Criteria
In order to be included in this systematic review, articles had to meet the following inclusion criteria: be original research, a randomized controlled-trial, include participants that were athletes under the age of thirty, have an acute or chronic sport-related concussion, and include physical therapy intervention(s). Randomized controlled-trial articles were chosen due to high placement on the hierarchy of evidence and to strengthen the results of this systematic review. Articles were excluded if they were not of a randomized controlled-trial study design, not reported in English, or did not fit the inclusion criteria stated.
Search Strategies
The following databases were utilized for the search: PubMed, CINAHL, Proquest, MEDLINE, SPORTDiscus, and SCOPUS. The search strategy focused on three key concepts: athletes, concussions, and physical therapy interventions. After these concepts were identified, similar terms were noted, defined, and used in the searches. These terms were then utilized in each database and any database-specific terms such as Subject Heading (SH) or Medical Subject Heading (MESH) when relevant. Appendix 1 provides the specific search strategies utilized in this search. A hand search was completed by looking through the references of articles included in this systematic review. The initial search was started in March 2021 and the final search concluded in January 2022.
Study Selection
The total number of abstracts, titles, and full texts from the search strategy were divided in half and allocated to two teams of two authors. Each title, abstract, and full text for each article was assessed independently and screened by two separate authors to be reviewed for inclusion in the systematic review. If a tie breaker was needed due to a disagreement between team members, then a third author would serve as a tie breaker. Any duplicates found during the search were removed. Cohen’s unweighted Kappa was calculated for agreement during the title, abstract, and full text review. “Kappa is a measurement that is used to determine agreement among raters when scores are repeated.”13 Recommended values for Kappa include: <0.00 is poor agreement, (0.01-0.20) is slight agreement among raters, (0.21-0.40) is considered fair agreement, (0.41-0.60) is moderate, (0.61-0.80) is considered substantial agreement among raters, and (0.81-1.0) is almost perfect agreement."13
Risk of Bias in Included Studies
Risk of bias assessment for included studies was performed by two authors independently and was reviewed for each of the articles. If a disagreement was present, a third author would serve as a tiebreaker to reach consensus. Risk of bias assessment in the included studies was assessed using the PEDro scale. The PEDro scale is an appropriate tool to assess the quality of randomized controlled trials. A higher score on the PEDro scale indicates a lower risk of bias in an article, with the highest score possible being a 10 and lowest score of a 0. The PEDro scale has 11 criterion but is only scored using 10, thus has a score out of 10. One item, the item on eligibility, is not counted towards the score because it is related to external validity. The PEDro scale does not assess external validity or effect size of treatment.14
Data Extraction
Two authors performed data extraction independently. Consensus was reached after independent extraction. Data extraction included: Authors, subjects, gender, mean age, acute or chronic concussion, treatment for intervention group versus control group, and outcomes measured.
RESULTS
Study Selection
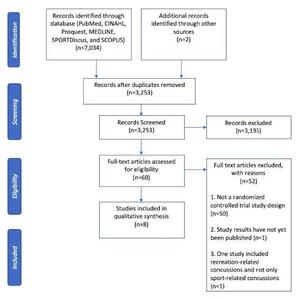
The initial search results produced 7,034 titles. There were 3,253 titles found after all duplicates were removed. Two authors screened titles and abstracts and 3,193 articles were excluded. A hand search was completed, and two additional randomized controlled trials were included. After title and abstract review, 60 articles were chosen for full-text review with an observed kappa value of one and confidence interval of one to one demonstrating perfect agreement between reviewers. Non-randomized control trials were excluded as well as one ongoing study, which resulted in eight articles that fit the inclusion criteria to be included in the systematic review. Details of the study selection can be seen in Figure 1.
Study Characteristics
Aerobic intervention for the treatment groups was used for four of the eight articles, and multimodal intervention for the treatment groups was used for the remaining four articles. The control groups for each of the articles either participated in education, rest, sub-therapeutic exercise, placebo, or sham treatment. The outcome measures varied throughout the eight studies and included: days from injury to recovery, PCSS, PCSI, Health Related Quality of Life, Beck Depression Inventory for Youth, Pediatric Quality of Life Multidimensional Fatigue Scale, the BESS, ImPACT, time to return to play, health and demographic questionnaires, Borg CR10, Rate of Perceived Exertion (RPE), and Post Ride Symptom Change Rating. See Table 1 for a description of the outcome measures that were used in the articles included in this systematic review. In total, there were 375 subjects that participated in the eight studies with 163 females and 212 males. The age range of participants included was 11.2-21.2 years old. Four articles included subjects who had acute post-concussion symptoms, one article included participants with chronic post-concussion symptoms, two articles included participants with both acute and chronic post-concussion symptoms, and one article did not indicate severity of concussion. Six of the eight articles included participants who have had one concussion or a recurrence of concussions while the other two articles did not indicate occurrence of concussion. Study characteristics can be found in Table 2.
Quality Assessment
Two reviewers assessed the risk of bias of the eight articles included in this systematic review using the PEDro Scale. Each of the articles was given a PEDro Scale score, shown in Table 3. To evaluate the level of agreement between the two reviewers, an unweighted kappa was calculated totaling one, (CI = 1:1), which demonstrates perfect agreement. Five of the eight articles were of a higher quality relating to risk of bias compared to the other three included articles, with scores ranging from a 5 to a 10 out of 10 items. Three of the five higher quality articles found significant improvements in the treatment groups compared to the control groups.20,21,24 Although only three articles demonstrated statistically significant results for the treatment group compared to the control group, all articles demonstrated improved symptoms with time and there were no adverse effects reported with early physical activity and therapy. Three of the eight articles had a lower quality relating to risk of bias scoring a 3 to 4 out of 10 items.19,25,26 Criterion 1, 2, 4 and 10 were met by all articles included in this study.
Results of Individual Studies (Interventions)
Aerobic Intervention
Four of the eight studies included in the systematic review used aerobic interventions for the treatment group.19–21,26 Leddy et al.20 included aerobic exercise on a stationary bike or treadmill if available, or walking/jogging outdoors if they did not have access to exercise equipment. The aerobic exercise would last 20 minutes or until their symptoms increased by two or more points from their pre-exercise symptom level (based on a 10-point Visual Analogue Scale). Participants in the aerobic exercise group recovered in a median of 13 days compared to the control group who recovered in 17 days (p = 0.009). Leddy et al.21 included aerobic exercise such as walking, jogging, or stationary biking. The aerobic group would exercise for 20 minutes and up to 90% of their maximum heart rate achieved on the Buffalo Concussion Treadmill Test. They were instructed to stop when reaching 90% of their maximum heart rate or when they experienced concussion-like symptoms. Median days to recovery for the aerobic exercise group was 14 days compared to 19 days for the stretching group. Four out of 43 participants in the aerobic exercise group (9%) had persistent post-concussive symptoms, compared to 12 out of 39 participants in the stretching group (31%), (p=0.014 with Fisher’s exact test). Maerlender et al19 had participants ride on a stationary bike with an RPE of 0 - 6 for 20 minutes or until they felt uncomfortable. There was no significant difference between groups for days of recovery, with a median of 13 days to recovery for the standard group, and 15 days to recovery for the exertion group. Micay et al26 had participants complete eight sessions that progressed with duration and intensity using a stationary bike that was connected to a heart rate monitor. Each session started with a five-minute warm up and ended with a five-minute cool down. If symptoms worsened, intervention was terminated. The aerobic exercise group showed greater symptom resolution compared to the control group over time, however there was not a significant difference between groups. Independent t-tests were performed for or between-group difference in mean time to medical clearance which was 36.1±18.5 days for the aerobic exercise group and 29.6±15.8 days for the control group (t(13)=0.03; p=0.87).
Multimodal Intervention
Four of the eight studies included in the systematic review used multimodal intervention for the intervention provided to the treatment group.22–25 Chan et al.22 utilized an active rehabilitation program including submaximal aerobic training, light coordination, sport-specific exercises, visualization and imagery techniques, and a home exercise program. The active rehabilitation group had a mean ± SD change of -24.7±19.1 on the PCSS from baseline to follow-up. The control group had a mean ± SD change of -15.8±12.5 on the PCSS from baseline to follow-up. These results were associated with a significant difference between groups with a Cohen’s d treatment medium effect size of 0.55. Reneker et al.23 study’s treatment group received manual techniques including soft tissue release, mobilizations, and thrust manipulations, and vestibular rehabilitation techniques including habituation, adaptation, oculomotor control, neuromotor control, and balance exercises. The interventions provided were tailored to each specific patient’s needs and progressed over time as the patient’s symptoms would allow. The median number of days to post-concussion syndrome (PCS) recovery for the experimental group was 13.5 days and 17 days for the control group, with a log-rank of 0.13 representing no statistical significance between groups. Schneider et al.24 had participants in the treatment group receive cervical spine physical therapy interventions and vestibular rehabilitation accompanied by non-provocative range of motion exercises, stretching, and postural education. The cervical spine physical therapy interventions included manual therapy of the thoracic and cervical spine and therapeutic exercises including cervical neuromotor retraining exercises. The vestibular rehabilitation was individualized to each person and consisted of habituation, gaze stabilization, adaptation exercises, standing and dynamic balance exercises, as well as canalith repositioning maneuvers. There was a greater number of participants that were medically cleared to return to sport within eight weeks of treatment in the treatment group (11 of the 15 individuals), compared to the control group (one out of the 14 individuals). Individuals in the treatment group were 10.27 (95% CI 1.51 to 69.56) times more likely to be medically cleared to return to sport within eight weeks than the participants in the control group (p<0.001). Dobney et al25 had participants in both the treatment group and control group complete 15 minutes on a stationary bike or treadmill, 10 minutes of coordination and skill practice related to sport preference, 5 to 10 minutes of visualization related to sport preference, and education about recovery, coping with post-concussion symptoms, and the process of returning to school or sport. The only difference between groups was that the treatment group started two weeks post-concussion and the control started treatment four weeks post-concussion. Participants were instructed to discontinue activity if symptoms increased. Post-concussion symptoms improved over time for both groups, with no significant difference between the two groups.
Overall
When looking at physical therapy interventions, whether it be aerobic interventions or a multimodal approach, the included studies show improvements in outcomes of time to recovery and reduction of post-concussion symptoms in patients who have had a concussion. Four of the studies had significant between-group differences. The other four did not have significant between group differences but did show improvements overall with no significant adverse effects.
DISCUSSION
The aim of this systematic review was to investigate the effectiveness of physical therapy interventions for athletes post-concussion. There is a gap in the current literature regarding sports-related concussions in athletes and appropriate interventions for treatment. This review aims to reveal physical therapy interventions to address post-concussive symptoms. Overall, this review demonstrates decreased time to recovery and reduced post-concussion symptoms when patients receive active physical therapy interventions post-concussion. None of the studies demonstrated any significant adverse effects from early physical activity and physical therapy intervention, indicating that this treatment approach is safe for adolescent and young adult athletes post-concussion. Physical therapists should incorporate physical activity and physical therapy interventions earlier to optimize post-concussion recovery.
One limitation of this systematic review is that three articles were at high risk of bias according to PEDro, including Maerlender,19 Micay,26 and Dobney.25 Another limitation is that all studies included a small sample size that ranged from 15 to 118 total participants. This could result in larger effect sizes, decrease the power of the data, and be unrepresentative of the population. One article included only male participants decreasing the generalizability of the results.26 Another limitation of this systematic review is that the articles reviewed incorporated both acute and chronic concussions. By including both, the variation in time to resolve symptoms and return to play following the concussion may impact the overall validity and generalizability of the results. Because some of the articles included a combination of treatment interventions for athletes post-concussion, this made determining which treatment was most effective and beneficial for the participant difficult to determine.
One strength of this systematic review is that only randomized control trials were included. Kappa statistics were calculated among authors and resulted in perfect or near perfect agreement and this review was conducted following PRISMA guidelines. Lastly, available articles for this systematic review are from the year 2014 to present, and attempt to provide the most up to date research on athletes with post-concussion syndrome.
A weakness of this review is the results from the search strategy captured physical therapy interventions that were similar in nature being either aerobic or multimodal, as opposed to a broader spectrum of potential interventions. Also, limited evidence is available regarding athletes post-concussion resulting in only eight randomized control trials available for this review.
There are multiple published systematic reviews that present similar findings. One included 14 articles comparing rest and exercise and concluded that exercise was beneficial at improving PCSS score, decreasing symptoms, and decreasing the duration of lingering post-concussion symptoms.27 A systematic review that included five articles assessing athletes post-concussion with aerobic training demonstrated improvements in post-concussion symptoms.3 Along with these, a systematic review by Makdissi et al28 also found evidence supporting the importance of including physical therapy and aerobic exercise in the treatment of a sports related concussion. This review specifically assessed athletes with persistent symptoms, but they found evidence that treating the patient’s specific persistent symptoms that was beneficial and safe. Lastly, a systematic review that assessed mode and intensity of treatment post sport-related concussion found that light, moderate, and high-intensity levels of exercises can be safe and beneficial for patients during treatment.
The results of this systematic review suggest that physical therapists should incorporate early physical activity and physical therapy interventions into their treatment for adolescent and young adult athletes with post-concussion syndrome. Practicing therapists should determine the individualized impairment(s) present, treat the impairment(s), and use symptom reporting as a guideline to return the athlete to sport to ensure proper timing of interventions.8,9 Due to limitations of this current study, future research should investigate the impact of physical therapy interventions for adolescent and young adult athletes status post chronic versus acute concussion rather than mixing the two and research should be conducted with a larger sample size to allow for a more accurate effect size to be calculated. Future research should also investigate the superior intervention for adolescents and young adults suffering from post-concussion syndrome and determine if single treatment is more beneficial or if multimodal approach is more beneficial to the participants’ recovery. Lastly, future research should include more randomized controlled trials to improve validity and enhance professional decision making.
Conclusion
The results of this systematic review indicate that there is evidence supporting the use of physical therapy interventions including aerobic or multi-modal treatments in the treatment of adolescent and young adult athletes post concussion. The evidence included in this systematic review suggests that aerobic exercise or multi-modal interventions may lead to quicker recovery and return to sport in adolescent and young adult athletes with post-concussive symptoms when compared to traditional treatments such as physical and cognitive rest. Physical therapists should consider incorporation of these interventions into their plan of care for this population to allow for quicker recovery and return to sport.
Conflicts of Interest
The authors indicate no conflicts of interest in the reporting of this systematic review.