Introduction
The anterior cruciate ligament (ACL) injury is among the most frequent injuries in competitive games.1 The prevalence of ACL injury in Saudi Arabia is calculated at 31 injuries per 100,000 people.2 ACL injuries account for around 53% of all knee injuries and affect 60% of young active participants.2
ACL injury is usually managed surgically by ACL reconstruction (ACLR) followed by rehabilitation. As the ACL rehabilitation program progresses, determining the appropriate return to play (RTP) time is difficult and somewhat complicated.3 The RTP has to be strongly individualized to train the knee for competition and prepare the whole body for the next step.4 For optimal neuromuscular patterning and biomechanics, the knee needs to be stable and solid.5 The athlete, however, needs to be psychologically prepared for RTP.6
Psychological issues frequently are at play during both the acute and recovery phases following surgery and might be present for many years after the ACLR.7 Although an assessment of psychological readiness following ACLR was developed to predict the time of RTP, this has not been formally integrated in the rehabilitation protocols and has not been studied adequately.8 Moreover, the fear of movement might also contribute to re-injury and has been shown to affect RTP.9 Indeed, a lower psychological readiness and a higher score of fear of movement might be among the most relevant factors associated with re-injury after ACL, yet they are still not consistently considered during the rehabilitation phases.10
Some authors have examined psychosocial intervention and its effectiveness in improving RTP outcomes after ACLR.8 A systematic review was done by Coronado et al.,8 looking for the role of psychosocial intervention with regard to improving patient-reported clinical outcomes after ACLR. Their review suggests that there is limited evidence on the reduction of the fear of re-injury. Besides, there is little evidence of the effectiveness of psychosocial approaches in the post-surgical phase to improve functional rehabilitation following ACLR.8 In order to apply a high-quality experimental design in the conduct of research assessing the effectiveness of any novel intervention, first and foremost the assessment of the feasibility and acceptability of such investigation should be examined. Therefore, this study aimed to examine the feasibility and acceptability of adding a structured educational session to the rehabilitation program for soccer players post ACLR.
Method
Ethical approval was obtained from the Research Ethics Committee of the Faculty of Rehabilitation and Health Science at Prince Sattam University in Kharj, Saudi Arabia (IRB: RHPT/021/006). The study was registered in the Research Registry (ResearchRegistry.com) with registration number 6634.
Design
A feasibility double-blind randomized controlled study was conducted in collaboration with the sport rehabilitation center in Riyadh, from March 28, 2021 until April 6, 2021. Participants were randomly allocated to either the intervention group (Group A: usual care with a structured educational session) or the control group (Group B: usual ACL rehabilitation program).
Participants
Soccer players undergoing ACLR rehabilitation were invited to participate in the study. All the players included had to satisfy the inclusion criteria.
Inclusion criteria
Soccer players (professional and amateurs) were invited to participate if they satisfy these inclusion criteria:
-
Aged between 18 and 45 with an ACL injury.
-
Have undergone ACLR (any graft type; patellar or hamstring) and were at any rehabilitation phase of ACLR rehabilitation.
-
Were able and willing to give informed consent.
Exclusion criteria
Players with any additional surgical procedures other than ACLR and/or undergoing prevention programs (discharge phase from rehab services) were excluded.
Recruitment
A convenience sample of soccer players was recruited from the center. Potential participants were invited to participate. Information on the participant’s demographics (height, weight), dominant leg (as described by which side they preferred to kick a ball), average number of hours spent in a week for rehabilitation was collected. In addition, Tampa Scale of Kinesiophobia (TSK-17), ACL-Return to Sport after Injury (ACL-RSI), and International Knee Documentation Committee (IKDC) were completed electronically by all participants using google forms (https://docs.google.com/forms).
Masking
To minimize bias, the study was double-blinded. Thus, the outcome assessor and the clinicians involved in the rehabilitation had no information on group assignment.
Randomization
Each player had an equal chance of being assigned to either one of the study groups. The allocation was concealed, and the sequentially generated numbers were placed into opaque sealed envelopes.
Intervention
The control group
After randomization, participants in the control group continued their usual care in the same clinic. After one week, they were asked to answer the final survey.
The intervention group
Participants in intervention group received the same rehabilitation protocol as the control group, and attended a virtual interactive structured educational session via ZOOM platform. The educational session included a series of topics related to the surgery and the rehabilitation process as well as simple answers to some frequently asked questions among players undergoing ACLR rehabilitation.
The structured educational topics were prepared and supplemented with graphs and pictures to ensure the clarity and understandability of the materials. The educational session materials were based on recent evidence, available literature, and advice from five expert sport physiotherapists.
After one week, the participants were asked to answer the final follow-up survey. In addition, they were asked to answer whether “the intervention and the randomization were acceptable”, with optional choice to add more details using open-ended questions (by both players and clinicians) regarding the acceptability of the intervention and randomization.
Estimated sample size
The sample size was based on the number of patients with ACLR attending the center. In the three months prior to recruitment, 45 ACLR players visited the center. The percentage of consenting eligible players was expected to be 50%, resulting in eight players randomized per month. This translated into an expected total of at least 24 players over the proposed three months of recruitment. Therefore, this feasibility study aimed to recruit at least 24 participants.
Outcome measurement
Tampa Scale of Kinesiophobia (TSK-17)
The TSK was originally employed to evaluate the fear of movement in patients with low back pain. It has also been used to assess fear of re-injury and pain in patients with different conditions, such as ACL injuries.11,12 It consists of a self-report checklist of seventeen domains using a Likert scale of four items. Total values from 17 to 68 indicate a high degree of kinesiophobia. The cut-off score has also been established by Vlaeyen et al.13 The Arabic version of the TSK showed high test-retest reliability between repeated measurements. It demonstrated an intraclass correlation coefficient (ICC) of 0.86 and a Cronbach alpha value of 0.87 for low back pain patients.14 For post-ACLR patients it showed an ICC of 0.93 and a Cronbach alpha value of 0.90, which represent strong internal consistency.15
ACL-Return to Sport after Injury (ACL-RSI)
The ACL-RSI scale was developed to assess a number of psychological factors associated with return to sports, such as fear and frustration, confidence, and self-efficacy.9 Twelve elements are tested on a scale of zero to 100, measuring three psychological frameworks: emotion, confidence, and risk perception.9 Higher ratings reflect a more optimistic view on RTP, 56 or more reflect the ability to RTP, and 76 and more indicate a return to maximum performance.9 The test-retest reliability of the Arabic ACL-RSI was high (ICC = 0.93).
International Knee Documentation Committee (IKDC)
IKDC consists of 18 questions in the regions of symptoms, working during everyday life, current function of the knee, and involvement in work and sport.16 The Arabic IKDC showed an excellent test-retest reliability between repeated measurements, as the ICC in patients post ACLR was 0.95.15
Data analysis
Feasibility study indicators
- Recruitment number:
- Set goal: 24 players
- Acceptability rate
- Set goal: at least 65% of eligible participants consent to participate in the trial.
- In addition, if most participants and clinicians reported that intervention and randomization were acceptable (open-ended questions).
- Retention rate
- Set goal: ≥ 80% at the follow-up survey
Statistics
The mean, Standard deviation (SD), absolute and relative frequency, were used to describe the data.
Chi-square test was used to examine the significant difference between the two groups.
Results
Participant selection, enrollment, and allocation
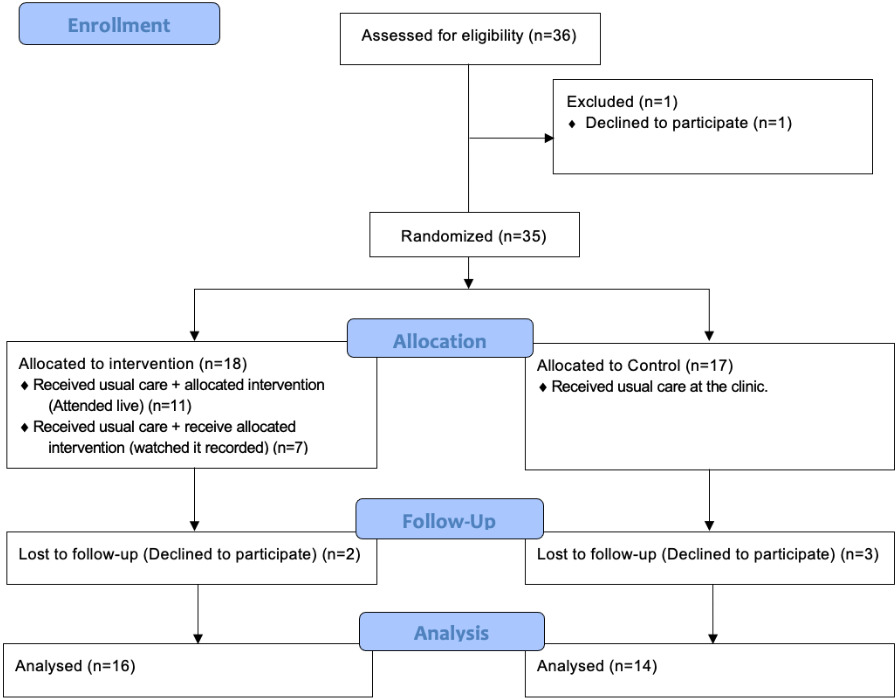
There were 36 players rehabilitating post-ACLR at the center at the time of the study. They were screened and all 36 (100%) satisfied the inclusion criteria. One participant (2.7%) of these 36 did not wish to participate in the study, providing the reason he did not have time to participate. The remaining 35 (97.2%) consented to participate and agreed to be randomized. Of these, 30 (85.7%) completed the study (the one-week follow-up).
After randomization, the 35 participants were randomly assigned to one of the two groups: the intervention group (n=18 at baseline, with two losses to follow up; n=16) and the control (n=17 at baseline, with three losses to follow up; n=14).
The intervention group received the online educational session (either live or recorded), with eleven (61.1%) of the intervention group receiving the educational session synchronously at the same time that the instructor performed it. The other seven (38.9%) could not attend the live educational session, therefore they watched the recorded lecture later on the same day. The latter group was instructed to ask and comment on any information needed. The progress of the RCT phases is depicted in Figure 1 (Flow Diagram).
Demographic data
The 35 participants included were ACLR male players with a mean (SD) age of 26 years (±6), an average mass of 78.6 kg (±13.8), and an average BMI of 25.8 (±3.8). Of these, 27 (77.1%) had suffered from an ACL injury in the right knee, and eight (22.8%) in the left knee. Additionally, 14 (40%) had received patellar tendon graft reconstruction for the ACL, ten (28.6%) had received hamstring tendon grafts, three (8.5%) had received allografts, and eight (22.8%) were unsure about the graft type.
Participants in both groups had similar physical characteristics (p>0.05). The intervention group had more patellar tendon-bone grafts than the control group (72.2% to 5.88%, respectively; X2 [2, n=35]=13, p= 0.0002).
The average time to rehabilitation start post ACLR was 3.1 days, ranging from zero to 14 days, with six (17.1%) starting their rehab immediately after the surgery. Table 1 presents the demographic and clinical characteristics of the participants in both the intervention and control groups.
Feasibility indicators in the RCT
In this study, the feasibility indicators were:
Recruitment number
- Set goal: 24 players
Overall, 36 players were screened over the one-day recruitment period. Of these, 36 satisfied the inclusion criteria. All the participants completed the questionnaire, and there was no missing data. The questionnaire completion typically took five to fifteen minutes, and according to the participants, none of the items were said to be complicated.
Acceptability rate
- Set goal: at least 65% of eligible participants consent to participate in the trial. In addition, most of the participants and clinicians report acceptability of the intervention and randomization.
One participant (2.7%) did not wish to participate in the study while 35 (97.2%) agreed to join the trial.
All the participants responded to the yes/no questions about the acceptability of the intervention and randomization, which were found to be acceptable by 100% of the participants. However, only two players and one clinician agreed to give a more detailed statement with regard to the intervention.
The participants’ responses suggest that an educational session at the beginning of the rehab is helpful regarding the awareness of the process; additionally, it might help players to overcome fear, thus enhancing psychological readiness post-ACLR.
Among the responses collected, we report the following representative ones:
-
“If I had received such an intervention from the beginning, it would have helped me understand more about my situation and have a reasonable expectation regarding RTP timing and readiness.” A23
-
“This is a unique way of helping ACLR patients with their understanding of the plan of treatment; my clinician had discussed the information provided in the lecture with me before, but not in an organized and structured way like the one we had in the lecture. I think it will be a great addition to the rehabilitation plan. Still, I think it will be much better if it provided onsite, rather than online, so it will be easier to interact with the lecturer and participate.” A35
One of the clinicians also responded as follows:
- “The lecture is a great way to help the patients wonder and answer most of their questions. However, I think it will be of great value for the patients to have it at the beginning of their rehab and also to have a repeated section addressing their current phase, at the end of each phase.” Clinician 1
Retention rate
- Set goal: ≥ 80% at follow-up.
In the follow-up (one week after the randomization), 30 (85.7%) participants completed the questionnaires, and five (14.3%) declined to participate in the reassessment, two reported they were not interested to participate in the follow up, and three reported that they did not have time to answer the survey.
Outcome measures
The baseline measurements showed similar levels of fear of re-injury in both groups based on TSK-17 scores (mean of 41.7 for the intervention and 41.8 for the control). However, ACL-RSI was slightly higher in the intervention group at baseline (mean of 65.3; SD ± 23.7) compared to the control (63.7; SD ± 20.4). Similarly, this was also the case with the IKDC measure (73.2; SD ± 14.3 for the intervention compared to 68.7; SD ± 15.6 for the control). Table 2 shows the outcome measurement scores of the participants in both the intervention and control groups.
In the follow-up measurement, the intervention group shows improvement from the educational session after one week with a lower TSK-17 mean score =37.6; SD ± 4.8), and an improvement in readiness as shown by an increased ACL-RSI mean score =83.4; SD ± 15.8). However, there was no change in knee function as measured by the IKDC.
Discussion
This study indicates that conducting an RCT examining the effectiveness of adding a structured educational session to the rehabilitation program for soccer players post ACLR is both feasible and acceptable. This was based on achieving the recruitment number, acceptability, and retention rate indicators.
Patient education is an essential part of physical therapy intervention. It is widely used in most musculoskeletal conditions, such as back pain,17 and shoulder pain.18 In addition, patient education is considered to have some psychological aspects when treating the patient.19–21 Besides, no known adverse events are associated with education in physical therapy interventions. All of this makes education an important constituent to be included in other parts of the intervention.
In the intervention and control groups, the ACLR players were healthy, active men undergoing rehabilitation post-ACLR. Participants in both groups were mostly similar in terms of age, weight, height, BMI, and injured leg. However, the results showed more patellar tendon-bone grafts in the intervention group than in the control group (72.2%:5.88%). Nevertheless, the results regarding the strength outcomes and patient experience were similar after patellar tendon-bone grafts or hamstring autograft bone, and both exceeded the strength outcome following other types of surgeries for ACLR.22,23 Additionally, the question on the surgery type was self-reported; thus, it could be affected by recall bias. Indeed, almost half of the participants in the control group reported they did not know or could not remember the surgery type. Therefore, it is recommended that surgery type data be gathered in future studies directly from the medical/surgical record for each player.
The study’s main goal was to examine the feasibility of conducting an RCT to examine the effectiveness of adding a structured educational session to the ACLR rehabilitation.
Several indicators were set in this study to assess the feasibility of conducting a full-scale RCT.
The initial objective was to recruit at least 24 players with ACLR. This was calculated based on 45 ACLR players having visited the center in the previous three months (August to October 2020). The expected percentage of consenting eligible players was 50%, suggesting eight players could be randomized per month. This would result in at least 24 players over the three months, as proposed for the recruitment. This study was able to recruit and randomize up to 35 participants. This was possibly due to the fact that recruitment took place in a major private center specialized in rehabilitating such cases.
The second index addressed in this feasibility study was the acceptability of the intervention and randomization. The goal was to have at least 65% of the eligible soccer players willing to participate, in addition to the acceptability of the study by most of the participating players and clinicians involved. Only one player (2.7%) declined to participate in the study, thus ending up with 35 (97.2%) willing to participate in the study and to be randomized.
Furthermore, all participants responded they found both the intervention and the randomization as acceptable. In addition, the responses to the open-ended questions suggest that adding a structured educational session at the beginning and after each phase is also thought to enhance the awareness of the player about the rehabilitation process. Raising rehabilitation process awareness and covering most of the rehab phases is expected to help with the players’ fear of re-injury and their psychological readiness post ACLR.
Further, this study shows that it might be helpful to deliver the educational part through online recorded educational sessions, since 38.4% of the study participants in the intervention group could not attend the live online educational session and they had to watch it recorded. Sending the recorded lecture to be watched by every participant in the experimental group will help in standardizing the intervention and examining the effect. Despite some responses indicated that an onsite lecture would help in terms of better communication and interaction, future studies could include a special live event to discuss the educational session after watching it recorded. In the end, it is still an acceptable way to go further with a full RCT, and it should be remembered that the inclusion of patient satisfaction indicators is encouraged into the complete RCT, if this is to be conducted.
The third dimension addressed by this feasibility study was follow-up. In the study, 80% of the included players were maintained in the follow-up until the final assessment. The loss of follow-up in this study was 14.3% (n=5). A follow-up loss of 5% or less is typical.24 Conversely, a loss of 20% or more suggests that researchers should be worried about the risk of bias.25 Since 14.3% is closer to 20% we should be concerned and this should be looked at in future studies and intention to treat analysis may be considered to avoid any potential bias.
The study’s outcome measure results suggest that adding a structured educational session to the rehabilitation program for soccer players post ACLR might help reduce the fear of re-injury (using the TSK-17) and improve the level of psychological readiness (using the ACL-RSI) for players one week following the intervention. According to Ardern et al.,10 lower psychological readiness and a higher fear of movement score might be among the most important factors associated with re-injury. Yet, they are still disregarded during the rehabilitation process.
The results also showed no change in knee function in both groups one week after baseline as assessed by IKDC in patients post ACLR. This might be due to the short study’s follow-up and more theoretical intervention, with no change in the exercise program provided to the participants. Other studies used and observed an IKDC difference for knee function, when reassessed at a follow-up of more than six weeks.26,27
In conclusion, the main results of this study provided support for the feasibility of a novel RCT examining the addition of a structured educational session to the rehabilitation plan for players post-ACLR. In addition, multiple factors emerged from the players’ and clinicians’ responses to the open-ended questions that could improve the efficiency of future studies.
Limitations
A variety of factors limited the findings in this study and need to be taken into account when interpreting the results.
The significant differences observed in the two outcomes (TSK-17 and ACL-RSI) are questionable since this study was not powered to examine the significance of this difference. It is important to acknowledge the limited sample size (less than 35 per group is not ideal) when thinking of such difference in the outcome measures.28 Moreover, some factors may introduce confounding bias related to the participants’ characteristics and surgical type. It was also surprising that seven of the participants from the control group reported not knowing or remembering their surgical procedure, while none from the intervention group reported this. However, after looking back at the data collection procedure, we found a standard procedure regardless of the group assignment and therefore this can be only attributed to random error. In future studies, this can be mitigated using stratified sampling techniques and collecting information on the type of surgery directly from the medical/surgical files of the participants. Moreover, the relatively short follow-up of the study might have affected its results.
While the intervention was a live online version, more than a third of the target participants could not watch it synchronously, but had to watch it recorded; this may have impacted the standardization of the educational session.
Furthermore, using only one center to recruit the study sample is inherently linked with selection bias. A larger trial with multiple recruitment centers and on a larger sample would ensure more diverse groups and more robust results.
Conclusion
The results of this study indicate that conducting an RCT examining the effectiveness of adding a structured educational session to the rehabilitation program of soccer players post ACLR is both feasible and acceptable. However, several factors need to be considered before conducting a full-scale RCT, such as, longer follow-up time, multiple recruiting centers, larger sample size, and stratified sampling techniques to ensure similar groups. Finally, using recorded educational sessions would provide more standardized intervention, which is also deemed to be preferable.
Declaration of Conflicting Interests
The authors have no conflict of interest to declare.
Acknowledgments
We would like to thank the Researchers Supporting Project number (RSPD2023R647), King Saud University, Riyadh, Saudi Arabia, for supporting this research.