INTRODUCTION
Shoulder pain affects approximately one-third of individuals in a lifetime, and 36-70% of those who experience shoulder pain are diagnosed with either subacromial impingement syndrome or subacromial pain syndrome (SAPS).1–3 Subacromial decompression (SAD) surgery is one of the most common orthopedic procedures utilized to address SAPS with rates increasing 117-254% between 1990 to the early 2000s in the United States.4,5 In the United Kingdom, 21,000 SAD procedures were performed in 2010 costing nearly £50 million.6 Individuals with shoulder pain who receive a SAD exhibit similar clinical outcomes in pain, function, and quality of life when compared to those who receive conservative management, yet the procedure is frequently performed when individuals fail conservative management.3,6–9
There is no accepted definition for “adequate nonoperative treatment.” This requires judgment by the medical team and patient to determine if conservative treatment was sufficient before progressing to surgery.10 Completing conservative care is a common inclusion criterion to receive a SAD in the literature; however, studies seldom describe the provided interventions. This omission does not assist clinicians or patients in determining if adequate care was exhausted, a common clinical challenge, prior to recommending SAD. Standard care for SAPS is outlined in a recent clinical practice guideline (CPG) suggesting the exhaustion of conservative interventions prior to performing a SAD, and recommending that individuals only receive a SAD if functional loss persists following completion of conservative care.3,6 The CPG recommendations include physical therapy (PT), a guided home exercise program (HEP), non-steroidal anti-inflammatory drugs (NSAIDs), education, and subacromial injections (SI).6
PT intervention has high-level supportive evidence to treat individuals suffering from SAPS.11 Several randomized control trials exist highlighting equivalent outcomes and cost savings when individuals receive supervised exercise compared to receiving a SAD.12,13 Additional authors have found enhanced benefits from combined manual therapy (MT) and exercise over exercise alone.14–17 However, to date, PT is not always delivered to individuals with SAPS prior to undergoing a SAD.11,18 Therefore, identifying the PT interventions offered to people with SAPS prior to undergoing a SAD is needed in the attempt to understand why individuals continue on to surgery.19
Based on the current evidence, it is unclear if adequate conservative management is provided to individuals with SAPS prior to considering a SAD. Therefore, the purpose of this review was to describe the conservative interventions received by individuals with SAPS prior to undergoing a SAD in the published research. This information will allow for future critical appraisals (e.g. systematic reviews) in attempt to define adequate management to prevent SAD as well as assist clinicians and patients to determine if adequate care was exhausted before advancing to surgery. A scoping review allows for data extraction without the need for a critical analysis, and it can provide an overview of the available evidence without producing an answer to a discrete research question.20
METHODS
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses - Extension for Scoping Reviews (PRISMA-ScR) Checklist guided the design for this scoping review.21 The question was registered with the Open Science Framework and OSF Registries (Identification:
https://doi.org/10.17605/OSF.IO/EUP9C).
Search Strategy
A librarian assisted with the creation of a database specific search strategy for MEDLINE, CINAHL, PubMed, and Scopus. Keywords, boolean operators, MeSH terms, and MeSH subheadings were used. The search was conducted on February 11, 2022. The search strategy for PubMed is as follows and was adjusted to support each database search criteria:
(((((((((shoulder[MeSH Terms]) OR (“shoulder impingement syndrome”[MeSH Terms])) OR ("shoulder pain[MeSH Terms])) OR (shoulder*[Title/Abstract])) OR (“shoulder impingement syndrome”[Title/Abstract])) OR (shoulder impingement syndrome)) OR (subacromial pain syndrome)) OR (“subacromial pain syndrome”[Title/Abstract])) AND (((subacromial decompression) OR (“SAD”)) OR (“subacromial decompression”))) AND (((orthopedics[MeSH Terms]) OR (surgery[MeSH Subheading])) OR (surgery[Title/Abstract]))
Eligibility Criteria
Peer-reviewed randomized control and cohort studies with subjects diagnosed with SAPS, subacromial impingement syndrome, or subacromial shoulder pain were included since these terms are interchangeable.13,22–24 Both open or arthroscopic SAD procedures were included.
Studies published between January 2000 and February 2022 were considered since literature from the early to late 2000’s began to highlight non-superior results associated with SAD outcomes.9,15,25 Other inclusion criteria consisted of studies: (1) evaluating conservative interventions for SAPS, subacromial impingement syndrome, or subacromial shoulder pain when compared to SAD, (2) including subjects listed as having completed conservative care but ultimately received a SAD, and (3) subjects who did not receive any conservative care prior to undergoing a SAD. There was no language restriction in order to maximize study inclusion. An attempt to identify a translated study was made if not published in English.
If one or more of the following conditions were present, the study was excluded: (1) subjects had a concurrent acromioclavicular or glenohumeral joint separation or dislocation, rotator cuff muscle tear(s), humeral head avascular necrosis, humerus or clavicle fracture, glenohumeral labral tear or insufficiency, calcified tendinopathy, or glenohumeral joint osteoarthritis, (2) subjects had a history of undergoing a prior SAD or rotator cuff repair, a surgical procedure other than a SAD for shoulder pain, a procedure to address either a complete or partial rotator cuff repair concurrently with a SAD, or a total or reverse shoulder replacement, (3) cadaver studies, (4) subjects with SAPS receiving conservative management but unclear if advancement to surgery occurred, (5) follow-up studies performed on the same study population as the initial publication, (6) pharmacological studies focusing on pain management for consecutively scheduled SAD procedure, or (7) the study design was a systematic review, protocol, conference abstract, case study, narrative review, treatment clinical practice guidelines, or was published in a non-peer reviewed journal.
Data Extraction and Analysis
Title/abstract and full-text screening was performed independently by two reviewers (JS and GT). Disagreements regarding inclusion were resolved by discussion, and a third reviewer (JY) resolved the discrepancy if no consensus occurred. A quality assessment was not conducted given the purpose of this scoping review.
The same reviewers independently extracted the data meeting the inclusion criteria and collaborated to organize and validate the findings. The data extracted from each included study were: (1) the types and number of conservative interventions (if provided) completed by subjects prior to undergoing a SAD, and (2) duration of care (months) and/or treatment sessions completed, if available. Details for each extracted intervention were collected, such as the number of SI and/or injected medications, NSAIDs dosage and frequency, interventions and exercises used during PT, and exercises prescribed in the HEP as the details were available.
PT specificity was captured since it is a common conservative intervention received by individuals with SAPS.12,13,18 PT was defined as an intervention or a group of interventions provided by a physical therapist or physiotherapist. Additionally, only a licensed physical therapist can offer PT services, and the PT provider was identified to ensure a licensed professional rendered PT services. An intervention including no specific provider was categorized as an independent intervention. For example, if PT and ultrasound were separately listed but the provider delivering these interventions remained absent, these were identified as two separate interventions. If there was or was not a specific description of the treatment provided during PT services, it was categorized into specific-PT or non-specific PT, respectively.
For the purposes of this review, a HEP was defined as an unsupervised exercise regimen prescribed by any healthcare provider. The HEP compliance rate, if available, was collected since intervention adherence is associated with improved outcomes.26 If a physical therapist delivered the HEP, it would be categorized as a part of PT. For example, if a study mentioned PT and a HEP separately but did not clearly state the HEP was provided during PT services, then these were classified as two separate interventions. If PT included a HEP, then it was combined with PT and considered one intervention.
The data were subsequently reviewed to identify intervention clusters. Intervention clusters were defined post hoc as the most common combinations of interventions (e.g. both PT and SI is one intervention cluster).
RESULTS
The electronic database searches identified 1,426 studies. The scoping review included 47 studies7,14,18,27–70 after duplicate removal, title/abstract screen, and full-text review (Figure 1). A hand search produced one additional study.38 Two protocol studies71,72 were excluded; the two primary results studies7,60 based on the initial protocol publications were included. Lastly, Haahr and Anderson73 was excluded as this was a follow-up study on the same subject population from Haahr et al.42 The reviewer interrater agreement for the title/abstract screen was strong (𝑘=.76) and moderate for the full-text review (𝑘=.66). The two reviewers discussed and resolved all discrepancies. See Table 1 for a summary of results.
Physical Therapy
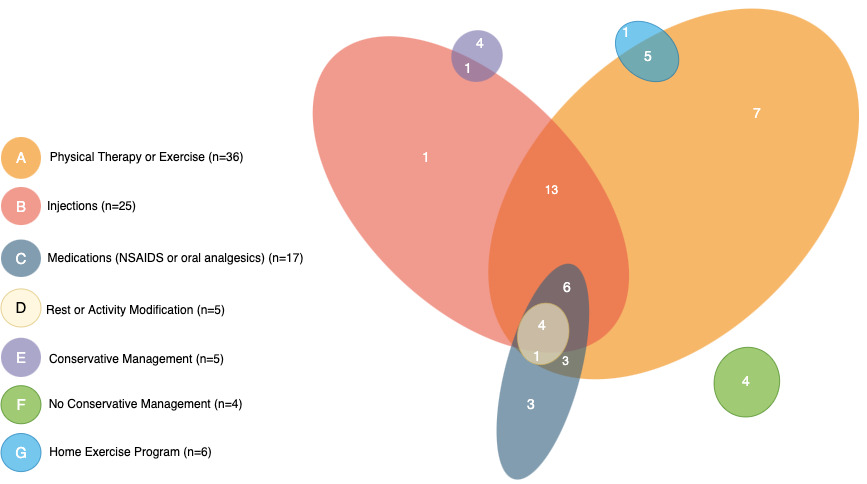
Thirty-six studies7,14,18,27,30–37,39–42,44,46,47,50,51,54,55,57–60,63–68,72,75–77 (76.6%) included PT/physiotherapy or supervised exercise. Twenty-four studies7,30,31,34,36,37,39,41,44,46,50,55,57–59,63–68,70,72,77 (51.1%) identified non-specific PT and did not provide details for the provided interventions. Twelve studies14,18,27,32,33,35,40,42,47,51,54,60 (25.5%) explicitly described specific-PT interventions. The specific-PT interventions commonly included eccentric or isometric strengthening of the rotator cuff muscles, scapular stabilization activities, modalities, joint mobilizations, pain-free range of motion, or a prescribed HEP. (Figure 2)
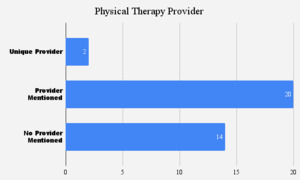
Fourteen studies7,32,34,50,55,57,59,63,65–68,70,77 (29.8%) did not identify if a physical therapist provided the interventions (Table 1). Twenty studies14,18,27,30,31,35–37,39–42,44,46,47,51,58,60,64,72 (42.6%) specifically mentioned that a physical therapist/physiotherapist provided the PT service. One study54 (2.1%) provided PT services from either a physical therapist or a physician, and one study33 (2.1%) rendered services in the Physical Therapy Department. (Figure 3)
Eight studies14,18,32,35,39,42,51,54 (17.0%) included MT. MT, soft tissue treatment, or massage were common terms. Only Holmgren et al.14 gave a specific description of the manual therapy method, technique, or targeted body region.
Seven studies29,32,35,42,51,66,67 (14.9%) included thermotherapy, and one study39 (2.1%) provided radial extracorporeal shockwave therapy. Several studies included electrotherapy,51,54 ultrasound,46,54 and taping.54,58 One study noted physical modality application within PT.18
Medication and Injections
Fifteen studies27,29,36,37,39,41,46,51,56,59,63,66,67,70,72 (31.9%) mentioned NSAIDs, and two studies39,50 (4.3%) provided oral analgesic medications. One study65 noted “analgesics” while another study70 mentioned “steroidal anti-inflammatory medication” without specifying application methods.
Twenty-six studies7,14,30,31,34,36–39,41,44,46,47,51,54–59,62,64,66–68,72 (55.3%) provided SI. Ten studies7,30,31,34,37,38,54,58,62,68 (21.3%) included subjects receiving at least one SI or more while 16 studies14,36,39,41,44,46,47,51,55–57,59,64,66,67,72 (34.0%) mentioned an unspecified amount of shoulder-related injections. Three studies47,51,57 (6.4%) mentioned receiving glucocorticosteroid injections, 17 studies7,30,31,34,36–38,41,46,55,56,58,59,62,64,67,68 (36.2%) noted steroid, and four studies14,39,66,72 (8.5%) described corticosteroid or cortisone injections. Eleven studies31,36–38,51,54,56,58,59,64,66 (23.4%) mentioned providing an injection directly into the subacromial space while the remaining studies were non-descript. See Table 1 for a summary of results.
Home Exercise Program
Six studies29,32,42,47,51,60 (12.8%) included a HEP prescribed by an unknown healthcare provider or a physical therapist. Five studies32,42,47,51,60 (10.6%) used a prescribed HEP within PT services while one study29 (2.1%) included a HEP without PT. Basharat et al.29 provided a HEP with specific exercise descriptions and dosages; all other studies32,42,47,51 provided no HEP detail. Four studies29,32,42,47 (8.5%) provided performance frequency associated with the prescribed HEP. Frequency was given as daily,42,47 five times per week,29 or a two to three times per week.32 No study mentioned compliance tracking or adherence to the HEP. See Table 1 and Figure 2 for a summary of results.
Duration of Conservative Treatment
Three studies37,40,41 (6.4%) provided conservative measures for a range of three to six months. One study75 (2.1%) delivered services for 12-16 months and another 15 studies27,29–31,34,36,46,48,55,57,59,66–68,70 (31.9%) provided interventions for six months. Ten studies7,28,33,39,42,44,47,52,64,72 (21.3%) provided three months of conservative care. One study56 (2.1%) ranged from two to sixteen months, one study38 delivered treatment for 4.5 months, and another provided intervention for 1.5 months.54 Two studies35,60 (4.3%) provided interventions for 15 conservative care sessions, one study32 (2.1%) completed 16 sessions, and one study18 (2.1%) provided more than five visits before undergoing a procedure. Holmgren et al.14 provided conservative measures for three months followed by two months of a HEP. See Table 1 for specific details.
Conservative Intervention Clusters
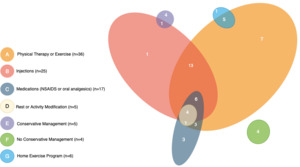
Interventions were clustered based on the most common combinations of interventions as reported in the reviewed studies (Figure 4).7,14,18,27–60,62–70,72 Four studies43,45,49,53 (8.5%) listed no conservative interventions, and four studies28,48,52,69 (8.5%) mentioned “conservative treatment” without description; one study mentioned conservative treatment in addition to receiving at least one steroid injection.62 Thirteen studies7,14,30,31,34,44,47,54,55,57,58,64,68 (27.7%) reported subjects received at least one or more injections combined with PT. Six studies36,37,41,46,59,67 (12.8%) included PT, NSAIDs, and injections. Four studies51,56,66,72 (8.5%) included PT, NSAIDs, injections, and rest or activity modification. One study38 (2.1%) included only injections, and three studies27,50,65 (6.4%) included combined PT and NSAIDS or oral analgesics. One study70 (2.1%) included PT, NSAIDs, and activity modification. Three studies29,39,63 (6.4%) included conservative care interventions unique to that study. Seven studies18,32,33,35,40,42,60 (14.9%) included PT only. (Figure 4)
DISCUSSION
This scoping review highlights the variability in the conservative interventions provided to individuals with SAPS before undergoing a SAD, further emphasizing the need for a standard of what is deemed “adequate conservative management.” Few studies provided specific intervention descriptions, such as dosage, type, frequency, medication, or duration of care. Additionally, the interventions received by individuals were provided by physical therapists less than half of the time. The findings from this review call attention to the need for specific criteria that should be met in individuals with SAPS, including maximizing the use of conservative management, before advancing to a SAD.
The majority (76.6%) of subjects in this review received some form of PT service. This finding aligns with research indicating PT, including MT and exercise, can positively impact outcomes for individuals suffering from SAPS17; however, it questions why individuals continue to undergo surgery. It brings into question whether the PT services rendered are “adequate.” The next most commonly delivered interventions included SI (55.3%) and NSAIDs (31.9%). This further brings into question if the standards of care as suggested by Vandvik et al.6 is sufficient to limit progression to SAD. This finding should be taken lightly as many conservative measures may be underreported; therefore, not allowing for a full comparison to recommended standards of care. Lastly, only one quarter of the studies offered specific details related to PT intervention, and less than half indicated that a physical therapist rendered PT services. This lack of transparency does not allow for the determination of whether or not adequate PT was provided.
It is concerning that non-invasive interventions are not consistent or exhausted despite being safe, beneficial, and cost effective since SAD procedures produce similar outcomes to conservative care.3,6–9 Furthermore, no conservative interventions were reported in 8.2% (n=4) of the included studies.43,45,49,53 This finding supports the inadequate attempts to offer effective conservative intervention prior to undergoing a SAD, and aligns with prior research on rotator cuff related pain conducted by Naunton et al.12 However, caution in making this conclusion is important as operative studies are not typically focused on detailing conservative measures prescribed prior to undergoing a SAD.
Vandvik et al.6 recommended that individuals with SAPS receive a guided PT program, including a supervised exercise program and patient education, before undergoing surgery. A majority of the included studies offered PT services to subjects prior to receiving a SAD, which aligns with conservative treatment recommendations3,6,12; however, over half of the studies lacked an exercise description and purpose for the intervention. Only a quarter of the studies included exercise specifications, such as exercise protocols to the rotator cuff musculature or general information about posture improvements. Additionally, few of the PT interventions included MT while only a third of the studies incorporated modalities. Less than a quarter of the studies included a well-designed HEP despite the potential benefits from prescribing a HEP with adequate dosing and frequency.78 No studies measured exercise compliance or compliance to attending PT appointments.79 These findings highlight the literature is not descriptive enough to define if adequate PT intervention was conducted.
Treatment provided by physical therapists should include specific exercise to the shoulder muscular, thoracic spine, and scapular stabilizers, along with information on psychosocial factors, pain neuroscience education, and behavior change.7,14–17,35,80 Future research should provide specific PT intervention details, if rendered PT services prevented SAD, and who provided the PT services since about a third of the studies did not list the provider of PT services. Providing specific intervention details allow for a better understanding of the completed services. Omitting intervention descriptions consequently limits outcome reproducibility in future research or in a clinical environment. Clinicians do not know the specific intervention type or dosage to use to enhance patient outcomes. Therefore, it is recommended to use a set structure to improve the recreation of a study’s result. The Template for Intervention Description and Replication (TIDieR) or Consensus on Exercise Reporting Template (CERT) can guide exercise intervention description81,82; the modified CERT could guide MT intervention and dosage.83 Enhanced intervention description, including exercise and MT, will allow for treatment efficacy to be measured and act as a valid comparator to surgery.81
SI served as the second most provided conservative intervention. Despite the high prevalence for this intervention in the reviewed literature, few studies mentioned the site of the injection, medication, or dosage. Approximately one-third of the included studies in this scoping review did not provide the injected medication or specify the number of injections, which aligns with prior research findings.84 Sun et al.84 observed irregularities in treatment protocols including the maximum number of injections to administer to a patient with SAPS prior to determining if they failed treatment. If SI are considered for an intervention to address pain associated with SAPS, the anatomical structure to receive the injection is to the subacromial bursa.85,86 The outcomes following SI do not appear to be significantly impacted if performed with ultrasound guidance or with anatomic landmarks when conducted by a trained clinician.86,87 A 21 gauge needle can be used to inject a methylprednisolone 40 milligrams and one milliliter one percent lidocaine mix directly into the subacromial bursa but recognize individual medical providers may alter the mixture based on experience and the treatment goal.85,86,88
Clinical management for SAPS often includes a multimodal approach. Combined PT and SI accounted for the most common (27.7%) conservative intervention grouping prior to undergoing surgery. These interventions were typically provided over a wide range of time (1.5-16 months). Unfortunately, an effective duration of conservative care prior to considering advancement to surgery remains unclear. Additionally, the timing of when conservative care is delivered remains unknown. For example, it is unknown if receiving PT and SI concurrently leads to an optimal outcome, or if sequential intervention prescription may work best (e.g. PT followed by SI, or vice versa). Several unknowns remain to best define adequate conservative management for SAPS to limit advancement to surgery.
Limitations
Only studies in the English language were included in the review despite attempts to identify translated studies. Also, no quality assessment was performed, which may limit the impact of the findings but can guide future systematic reviews. Lastly, there is a lack of high-quality PT CPGs for the treatment of nontraumatic shoulder pain. This makes determining exercise type, dose, duration, timing, and expected outcomes recommendations difficult.13,89
CONCLUSION
Conservative management for SAPS offers an equally advantageous outcome when compared to SAD. Many individuals continue to receive a SAD despite conservative care, bringing into question what is “adequate care” for individuals with shoulder pain. The findings from this scoping review indicate that typical interventions to conservatively manage pain, such as PT, NSAIDs and SI, are underreported or not offered to individuals with SAPS prior to undergoing a SAD. PT intervention shown to positively impact outcomes was underutilized in many studies, further highlighting that adequate care may not be utilized. The inadequate level of conservative care offered does not allow for a valid comparison to surgery. There is a significant need to investigate successful conservative interventions to prevent SAD.
FUNDING
There was no funding associated with this research.
ACKNOWLEDGEMENTS
Thank you to Cindy Reinl, Bellin College librarian, who assisted with the electronic searches.
AUTHORS DISCLOSURES
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the study.