INTRODUCTION
Injuries to the shoulder and elbow are commonplace in the athletic population and regularly occur in both contact and non-contact sports. In contact and collision sports such as American football, rugby, hockey and soccer, the shoulder accounts for up to 20% of all injuries, most commonly acromioclavicular joint sprains and glenohumeral instability.1–5 In college athletes attending the National Football League (NFL) combine, reported prevalence of previous shoulder injuries is 50-52%.1,6 In overhead sports such as baseball, softball, volleyball, tennis, swimming, and water polo, the shoulder accounts for 17-35% of all musculoskeletal injuries, most commonly involving labral and rotator cuff pathology.7–11 In baseball and softball athletes alone, elbow injury is also a significant source of disability accounting for up to 22% of injuries.12–14 Despite high upper extremity injury rates, athletes often seek care with the goal of returning to sport and pre-injury levels of performance.
The proportion of athletes who are successfully able to return to sport following upper extremity injury varies based on the injury type and surgical status. In athletes with shoulder instability, 40-88% of athletes managed non-operatively15–17 and 86-90% managed with surgical stabilization were able to successfully return to sport.18,19 However, only 50-73% of athletes return to sport at their previous level following surgical intervention.18,19 When considering overhead athletes with ulnar collateral ligament (UCL) injuries, 85-93% of athletes managed non-operatively and 75-100% of athletes managed with surgical reconstruction were able to successfully return to sport.20–22 However, only 84-93% of athletes managed non-operatively and 63-90% of those managed surgically returned to their previous level of competition.20–22
Recurrence rates for upper extremity injuries vary based on injury type and surgical status as well. The rate of reinjury after shoulder stabilization surgery has been found to be as high as 23%, but can be reduced to 10% with a comprehensive rehabilitation program.18,23,24 Following UCL reconstruction, revision rates are ultimately low (1-7%) but in a study following the outcomes of 147 athletes after UCL reconstruction, 26% of athletes returned to the injured list at some point in their career due to additional elbow injuries.25,26 These varied and less-than-ideal outcomes in return to sport and reinjury rates may be driven, in part, by the absence of an evidence-informed battery of tests used to determine an athlete’s physical performance and readiness for sport, ultimately resulting in athletes returning to sport before they achieve full physical performance of the involved upper extremity and kinetic chain.23,27
Physical performance tests, defined as assessments in which an athlete performs a physical task believed to be a component of a sports activity, can provide insight into an athlete’s readiness for return to sport.28 In athletes recovering from lower extremity injuries, the passing of physical performance tests (e.g., hop testing, agility testing) has been found to be effective in decreasing reinjury.29–32 However, current evidence on return to sport outcomes following upper extremity injury is comparatively lacking and limited to case series and clinical commentary.23,33 It is possible that this lack of outcomes research on the utility of upper extremity physical performance tests may be attributed to a lack of clinical use. If clinicians do not use upper extremity performance tests to make return to sport readiness decisions, there may be large variance in return to sport decision making and higher recurrence risk for upper extremity injuries in sports. Therefore, the purpose of this study was to explore the reported frequency of physical performance testing for return to sport readiness by physical therapists treating athletes with upper extremity injuries and the perceived potential barriers that may limit the use of these tests. A secondary aim of this study was to compare the practice patterns of clinicians with a sports physical therapy specialty certification to clinicians without this certification. The authors hypothesized that the majority of clinicians do not utilize upper extremity physical performance tests with their athletic patient population, and that the greatest barriers to their use would be a lack of awareness and understanding of current available evidence.
METHODS
Survey contents
A survey instrument was created to assess the frequency of use of physical performance tests by physical therapists treating athletes with upper extremity injuries, as well as the perceived barriers limiting the use of these tests. (Appendix) A team of three physical therapists highly experienced in the management of upper extremity athletes collaborated to develop the electronic survey using Qualtrics software (Qualtrics, Provo, UT). The development team reviewed and tested the survey among themselves, after which face and content validity were assessed by piloting the survey among a group of eight physical therapists. Feedback was gathered on the survey and modifications were completed in order to enhance survey clarity and functionality. The survey was designed to be completed in 5-10 minutes.
The survey was separated into three sections. Section I gathered information regarding the country the participant was currently practicing in, their years of experience, and specialty certifications as recognized by the International Federation of Sports Physical Therapy. Section II assessed the participant’s percentage of patient population that included patients with shoulder and/or elbow injuries, as well as those that had goals that included unrestricted return to sport. Specific clinical information grouped by the International Classification of Function, Disability, and Health (ICF) framework was assessed for utilization (Table 1). Participants were also asked if their testing battery changed based on the sport that the athlete was returning to and whether they would like to use more physical performance testing in their discharge planning. Section III of the survey investigated the participant’s reported barriers limiting the use of physical performance tests to assess activity limitations, the estimated percentage of patients who pass all pre-established physical performance tests prior to discharge, as well any reasons why patients are discharged prior to passing the physical performance tests. Categorical data were used for the frequency of patients passing all physical performance tests with responses of 25% or less considered “rarely,” 26 to 50% considered “sometimes,” 51% to 75% considered “frequently,” and greater than 75% of patients considered “consistently.” The survey instrument is available in APPENDIX 1.
The Consensus-Based Checklist for Reporting of Survey Studies (CROSS) guidelines were followed.34 All survey materials were approved prior to survey distribution by the Institutional Review Board at Baylor University (IRB# 1690573). Participants provided online consent before participating in the study. Inclusion criteria for survey participants were as follows: active, licensed physical therapist; currently treating in a sports or orthopaedic setting. All but three participants completed the survey in its entirety, failing to document their years of experience. However, all data captured was included in the data analysis.
Survey distribution
The study design was an international, cross-sectional survey using purposive sampling. The 19-question online survey was distributed via email and social media (Twitter) among sports physical therapists. The survey was sent to members of the American Academy of Sports Physical Therapy (sent to 6,797 members), International Federation of Sports Physical Therapy (14,350 members), American Society of Shoulder and Elbow Therapists (106 members), and the European Society for Shoulder and Elbow Rehabilitation (517 members). One reminder was sent to each membership organization one month after the initial email to maximize survey responses. The survey was written in English and was accessible between December 2020 and April 2021.
Statistical Analyses
Data were analyzed with SAS statistical software (JMP 16.3, Cary, NC). Participating physical therapist demographics were compared between those with and without sports specialization. Independent t-tests and Chi Square analyses were conducted to determine differences in practice pattern use of physical performance tests by physical therapists with and without specialization and the frequency of potential barriers that may limit the use of these tests. Significance was set at p=.05 with a Bonferroni adjustment to account for multiple comparisons.
RESULTS
Over the four-month collection period, 703 surveys were initiated with 512 being completed with consent (72.83% completion rate). Of those 512 participants, 498 were actively treating patients in a sports or orthopaedics setting (Figure 1). Of the 498 included participants, the mean years of clinical experience reported was 13.1(SD 10.6). The majority of participants (85.1%) were actively treating in the United States (n=424) and 14.9% were actively treating outside of the United States (n=74). Fewer participants (26.9%, n=134) had a sports specialization recognized by their respective country compared to 73.1% (n=364) of participants without. Of all participants, 70% (n=350) estimated that at least a quarter of their patient population present with shoulder or elbow injuries, and 56% (n=218) of participants estimated that at least a quarter of their patients with shoulder or elbow injuries have a goal of return to sport.
Information used in return to sport decisions
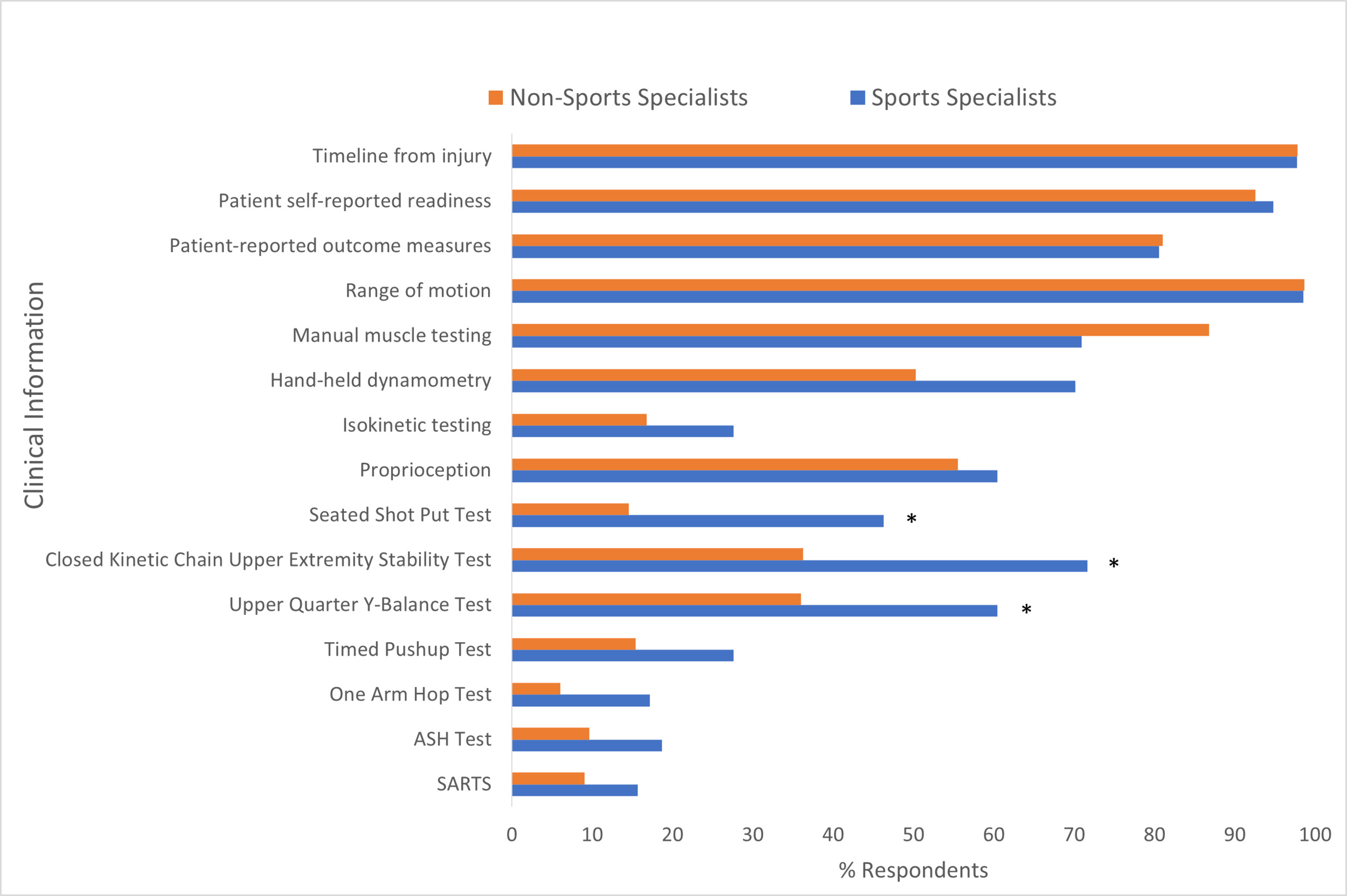
Using the ICF framework, results for the frequency of items used to make return to sport decisions are shown in Table 2. The most commonly reported factors used by physical therapists to make return to sport decisions using the ICF framework were: 1) impairments identified with range of motion and manual muscle tests, and 2) contextual factors such as patient subjective readiness to return to sport and patient reported outcome measures. Nearly all participants used time from injury to make return to sport decisions, while few participants reported using activity limitations with upper extremity physical performance tests when making return to sport decisions. Almost all participants stated that they tailored their battery of tests based on the sport to which the athlete is returning, and expressed the desire to use more physical performance tests in their return to sport assessments.
Results comparing responses reported by physical therapists with and without sports specialization in the criteria used with upper extremity athletes in return to sport decisions are shown in Figure 2. There were no significant differences (p>0.05) in the use of time from injury or contextual factors. However, sports specialists reported greater use of quantitative evaluation of muscle performance with hand-held-dynamometry (70.5%) than non-specialists (50.3%) (p<0.001). Although commonly used by both groups, non-sports specialists also rely on more frequent use of manual muscle testing (p<0.001) in return to sport decisions. Due to the low reported frequency of use isokinetic testing (<20%) overall, there were no significant differences between sports specialists than non-specialists. Most remarkably, sports specialists reported greater use of activity limitation assessments with physical performance tests. Specifically, 71.6% of sports specialists compared to less than 37% of non-sports specialists use the Closed Kinetic Chain Upper Extremity Stability Test. This was similar with the Upper Quarter Y-Balance Test that was used by 60.5% of sports-specialists compared to 36.0% of non-sports specialists (p<0.001). All the other physical performance tests were used infrequently (<28%) by sports specialists and non-sports specialists (<16%).
Barriers to the use of physical performance tests
As shown in Table 3, reported barriers to the use of physical performance tests included a lack of time (44.2%) and equipment (51.8%), a perceived lack of evidence supporting the use of upper extremity physical performance tests (38.0%), and a clinician’s lack of understanding of available evidence (50.2%). Lack of patient interest (7.6%) and lack of referral source interest (19.5%) were less commonly cited barriers. There were a few differences between barriers reported by sports specialists and non-sports specialists. Sports specialists were more likely (p<0.001) to cite a perceived lack of evidence supporting the use of upper extremity physical performance tests compared to non-specialists (48.5% versus 34.1%) and less likely (p<0.001) to cite a lack of understanding of available evidence (26.9% versus 58.8%). No other differences in perceived barriers were found between sports specialist and non-specialist groups.
The frequency of use of physical performance tests in discharge/return to sport planning
Overall, less than 25% of participants reported that their patients consistently passed all physical performance tests before discharge (Figure 3A). More than a third (36.6%) of sports specialists report patients consistently pass physical performance tests (Figure 3B) compared to less than a quarter (20.6%) of non-specialists (Figure 3C) (p=0.001).
The most cited reason participants report patients with return to sport goals being discharged prior to full physical performance was insurance visit limitation (68.9%), followed by patient self-discharge (67.9%), financial reasons (54.5%), clearance from another healthcare provider (52.8%), and external pressure for the athlete to return to sport (34.5%). Despite the infrequent use of physical performance tests, very few of the participants (2.2%) felt that physical performance tests were not important in discharge planning patients with return to sport goals, suggesting that most therapists believe physical performance tests should be used.
DISCUSSION
The overarching purpose of this study was to explore the reported frequency of physical performance testing in assessing return to sport readiness by physical therapists treating athletes with upper extremity injuries, and the perceived potential barriers that may limit the use of these tests. The hypothesis that the majority of participants do not use these tests was confirmed as fewer than half of participants reported using any physical performance test in making return to sport decisions for athletic patients with shoulder or elbow injuries. Similarly, the hypothesis that the greatest reported barriers to the use of physical performance tests would be a lack of understanding and awareness of current available literature was partially confirmed as lack of equipment was the most commonly reported barrier, followed by lack of understanding of the literature, lack of time, and perceived lack of literature supporting these tests. The secondary aim of this study was to compare practice patterns of clinicians with sports physical therapy specialty certification to clinicians without this certification. This hypothesis was confirmed as sports specialist clinicians were significantly more likely to use physical performance tests than non-specialist clinicians.
Information used in return to sport decisions
A particularly striking finding was that fewer than half of all participants (45.2%) utilized any physical performance tests to determine if a patient was appropriate to be cleared for sport, thereby neglecting to assess an athlete’s activity limitations. This percentage is even lower in non-specialist clinicians with only 36.2% of participants using physical performance tests compared to the 71.6% of sports specialist clinicians utilizing physical performance tests. This disparity may be partially explained by the advanced training sports specialists receive in return to sport assessment. However, in addition to assessing impairments, participation, and contextual factors, evaluating activity limitations is considered an entry-level skill by the American Physical Therapy Association (APTA) per their Guide to Physical Therapy Practice.35 The data suggests that, regardless of a clinician’s sports-specialization status, the physical therapy profession is overlooking a significant opportunity to assess activity limitations in this population.
One consideration is whether return to sport testing itself is an assessment that should be employed only with specialized training. The relative paucity of physical performance tests used in return to sport testing coupled with the reported lack of understanding of relevant evidence often results in a knee-jerk reaction to push physical performance tests into entry-level curriculum. However, it is important to first ask whether return to sport testing is truly an entry-level skill or that of an advanced practitioner. If it is the latter, this suggests the focus should not be on changing entry-level DPT curriculum but improving post-professional opportunities instead. For US-based specialists, the Description of Specialty Practice (DSP)36 for sports lists the implementation of “functional tests to determine athlete’s ability and readiness to return to sports activities” and implementing “sport-specific criteria and recommendations regarding the athlete’s readiness to return to sport” as activities performed by the board-certified specialist. The Description of Residency Practice (DRP)37 also notes that a residency program must utilize a curriculum that is inclusive of all the learning domains as noted in the Description of Specialty Practice, suggesting that the skills associated with return to sport decision-making are indeed better suited for residency-level education as opposed to entry-level, and that return to sport decisions are in line with specialty practice. Thus, in order to improve the utilization of physical performance tests in return to sport decision-making, barriers and challenges associated with accessing quality post-professional education should be explored.
Barriers to the use of physical performance tests in return to sport planning
A final takeaway from these findings is the distinct need for guidance on the clinical use of upper extremity physical performance tests. There has long been a call for higher quality research on upper extremity physical performance tests in both the healthy and injured athletic population,38 and sports specialists who participated in this study echoed this call as nearly half responded that a perceived lack of quality evidence is a significant barrier to their use of physical performance tests. However, the most cited barriers for the use of physical performance tests for upper extremity injuries from all participants were a lack of understanding of the current research, a lack of time, and a lack of equipment. These barriers are intricately linked, as a large percentage of physical performance tests currently available require minimal time and equipment to perform. With new literature providing guidance on how to utilize existing physical performance tests, each of these barriers can be considerably lessened. Considering these responses, the authors believe that the need for literature providing guidance on the use of upper extremity physical performance tests may be greater than the need for literature validating their use.
This study is not without limitations. First, while the study was distributed through the mailing lists of several professional organizations, it was also shared via social media limiting the ability to calculate an overall response rate. Second, in distributing through the mailing list of sports rehabilitation-specific organizations, there may have been somewhat of a selection bias as this clinician population may be more inclined to use physical performance tests than clinicians that do not belong to these sports rehabilitation organizations. That said, based on the current data comparing sports specialists to non-specialist clinicians, it is very possible that including a greater population of non-specialist clinicians would result in an even lower percentage of individuals reporting the use of upper extremity physical performance tests. Finally, while the survey was distributed internationally, most participants were US clinicians. As a result, these practice patterns may be generalized to physical therapist practice within the United States, but not necessarily indicative of practice patterns globally.
CONCLUSION
The results of this survey suggest that the vast majority of clinicians are not using physical performance tests in making return to sport decisions for athletes with upper extremity injuries. By omitting these tests, and neglecting to assess an athlete’s activity limitations, physical therapists are “missing the forest for the trees” and may be returning athletes to sport before full physical performance. While sports specialist clinicians are more likely to utilize these tests to assess an athlete’s activity limitations, all participants highlighted a perceived lack of supporting research, a lack of understanding of current research, and a lack of time and equipment to perform these tests in the clinic. Strategies recommended to overcome these barriers include increasing the emphasis on assessing activity limitations for return to sport clinical decision making in entry-level and post-professional education, reducing the barriers and challenges associated with accessing post-professional education, and developing clinical guidelines for the utilization of physical performance tests in athletes with upper extremity injuries.
Conflicts of interest
Authors have no reported conflicts of interest.

_before_dischar.png)

_before_dischar.png)