INTRODUCTION
Rupture of the anterior cruciate ligament is a well-known sports injury, with a higher injury incidence in females and those who participate in Level 1 sports.1–4 Traditionally, anterior cruciate ligament reconstruction (ACLR) with a bone-patellar tendon-bone (BPTB) or hamstring tendon (HT) autograft has been the preferred surgical procedure for managing complete tears of the anterior cruciate ligament, with a surgeon-preference towards the BPTB as the standard of care.5–9 Recently, international utilization of the quadriceps tendon (QT) autograft for primary and revision ACLR has increased in popularity10–13; ACLR with the QT may yield less graft harvest site morbidity than the BPTB and better patient-reported outcomes than the HT.14–16 However, revision ACLR outcomes from the Danish Knee Ligament Reconstruction Registry suggests higher graft laxity and failure rates when performing primary ACLR with the QT than both the BPTB and HT17; these findings have been debated,18,19 along with other literature reporting similar graft survivorship between the QT, BPTB and HT.14–16,20
Justifying the increased utilization of the QT for ACLR, anatomic and biomechanical studies have highlighted the robust properties of the QT itself, with superior levels of collagen density, length, size and load-to-failure strength than the BPTB.21–25 However, due to the multiple muscular origins of the quadriceps tendon, the QT has the potential for more variation in laminar structure and fiber orientation than the BPTB and HT.26–28 This non-uniformity of the quadriceps tendon, along with variation in surgeon skill and reconstruction technique, has been suggested as a reason for the higher QT failure rates within the Danish Knee Ligament Reconstruction Registry.17–19
In addition to intra-graft characteristics, graft-specific considerations for ACLR should also include fixation technique, management of the graft harvest site and the overall graft ligamentization process. For example, graft fixation with an interference screw may facilitate better graft incorporation than suspensory fixation and reduce the incidence of bone tunnel widening.29–31 Regarding the graft harvest site, ACLR with the QT and BPTB may produce more postoperative quadriceps weakness than the HT,14,32–34 whereas a higher incidence of kneeling-related knee pain has been reported with the BPTB than both the QT and HT autografts.14,15 Lastly, the bone-to-bone healing of the BPTB within the bone tunnels facilitates graft osteointegration, which is a more efficient incorporation process than the fibrovascular healing of an all soft-tissue graft35; these considerations influence surgical decision-making and the rehabilitation plan-of-care, to which the rehabilitation specialist must tailor their exercise prescription in an effort to optimize outcomes after ACLR.
Although previous literature has described rehabilitation considerations for the BPTB and HT autografts,28,36–39 there is less published with respect to the QT.39–41 Therefore, the purpose of this clinical commentary is to present the graft-specific surgical and rehabilitation considerations for ACLR with the QT, as well as further highlight the need for graft-specific rehabilitation strategies after ACLR by comparing the QT to the BPTB and HT autografts.
ANATOMIC AND BIOMECHANICAL CONSIDERATIONS
The quadriceps and hamstring tendons are different than the patellar tendon in their innate function to connect muscle-to-bone, whereas the patellar tendon connects bone-to-bone. Considering this, differences in stiffness and elastic properties are known to exist between autograft tissue used for ACLR,42–44 with the quadriceps tendon producing more absolute stiffness than both the patellar and semitendinosus tendons but a lower elastic modulus and relative strain tolerance than the patellar tendon24,28,44–46 (Table 1).
While these findings reflect total-graft biomechanical properties, previous work has highlighted the fact that regional variation in tendon elasticity and stiffness may also exist; the tendon region closest to the myotendinous junction is less stiff than the tendon region adjacent to the enthesis.48 This is an important consideration, as biomechanically-induced graft failure studies have reported a difference in failure location for the QT harvested with a patellar bone block (B-QT) than that of the BPTB and multiple-strand HT autografts; failure of the B-QT was most common at the bone-tendon interface,28,44 whereas universal stretch/mid-substance failures have been reported with the all soft-tissue QT (S-QT), BPTB and multiple-strand HT.28,43–45,47 These observations suggest the B-QT has more within-graft variation in regional elasticity and structure, creating increased stress at the bone-tendon interface and the observed graft failure-location.26,44,49
Compared to the HT and BPTB, more variation in laminar structure is present with the QT. In contrast to the continuous structure of the hamstring and patellar tendons, the quadriceps tendon is typically described as a common tendon with a three-layered arrangement; a superficial layer derived from rectus femoris, an intermediate layer from vastus medialis and vastus lateralis, and a deep layer from vastus intermedius.26–28 Although the extent to which laminar structure contributes to graft fixation pull-through is unknown, a biomechanical study by Arakagi et al50 reported significant suspensory fixation pull-through with a 150-newton load on the S-QT relative to a bone-block control.
GRAFT COMPOSITION AND HARVESTING TECHNIQUE CONSIDERATIONS
The harvesting technique of the QT can vary, and along with this, different rehabilitation considerations for graft composition are warranted. The B-QT facilitates partial graft osteointegration as early as 4-6 weeks after ACLR through the bone-to-bone healing of the single bone block within the bone tunnel,51,52 but likewise, carries a 1.4-8.8% risk of patellar fracture due to bone block harvest.53–55 Conversely, the S-QT is harvested without a patellar bone block and mitigates the risk of patellar fracture,54 but will take a minimum of 10 to 12-weeks for the fibrovascular interface to form between the S-QT and the bone tunnels.28,56–58 This between-graft difference in integration, in conjunction with the findings of Arakagi et al,50 suggests accelerated rehabilitation approaches may be less appropriate for the S-QT fixated with suspensory fixation, especially as graft tension is highly dependent on fixation until biological integration of the graft within the bone tunnels has occurred. While this is an extrapolated suggestion, short-term increases in graft laxity have been reported with the early introduction of open-kinetic-chain (OKC) quadriceps resistance training after ACLR, to which slightly increased levels of graft laxity were reported with the HT relative to the BPTB when OKC quadriceps resistance training with distal tibial load was initiated between 0-45 degrees of knee flexion weeks 6-12 after ACLR.59
The theoretical advantage of graft osteointegration with the B-QT is not currently supported by the literature.28,56–58 Specifically, a higher incidence of postoperative rotatory instability (16% vs 0%) and atraumatic graft ruptures (24% vs 0%) have been observed after ACLR with the B-QT compared to the S-QT54; these findings suggest ACLR with the S-QT may yield better postoperative stability than the B-QT. However, evidence is still limited,54 and the full-thickness B-QT appears to be more biomechanically similar to the BPTB than the S-QT, as well as may better-replicate the tissue properties of the native anterior cruciate ligament42,44 (Table 1). Lastly, ACLR with the S-QT may not provide adequate quadriceps tendon graft-length in some populations,60 especially women,61 and cosmetic retraction of the rectus femoris is a known complication related to proximal QT harvest.28,53,55
Outcomes comparing the full-thickness QT (F-QT) to the partial-thickness QT (P-QT) are limited with only one direct comparison published within the literature.62 QT thickness does not appear to influence donor site pain, failure rates or patient-reported outcomes.63 However, the biomechanical properties of the P-QT appear to be less robust than the F-QT44 (Table 1).
The F-QT produces a larger diameter graft and causes deeper disruption of the tissue at the graft harvest site. With this, violation of the suprapatellar pouch with F-QT harvest can produce a suprapatellar hematoma,53 which is a known complication after ACLR with the F-QT.40 More postoperative quadriceps inhibition may also be theorized with the F-QT relative to the P-QT, as full-thickness quadriceps tendon harvest will disrupt the laminar layers associated with the vastus medialis, vastus lateralis and vastus intermedius.26,27,64 Along with the inevitable increase in suprapatellar scarring, the high collagen density and graft-specific stiffness of the QT are suggested reasons for the observed incidence of arthrofibrosis after ACLR with the QT,20,40,65,66 to which the F-QT may exacerbate.67
EXTENSOR MECHANISM CONSIDERATIONS
Harvesting the P-QT may reduce the tensile strength of the quadriceps tendon by as much as 34%, which is greater than the 25% reduction in patellar tendon tensile strength after BPTB harvest.23 These findings have implications for rehabilitation, as greater impairments in quadriceps strength have been observed after ACLR with the QT and BPTB than with the HT.14,32–34,68 Following QT harvest, reduced quadriceps activation and strength may initially create a more protective healing environment at the graft harvest site. However, long-term reductions in quadriceps strength are detrimental to knee function and are one of the reasons why it may take longer to achieve performance testing milestones after ACLR with the QT and BPTB than with the HT.33,38,39,68
Considering P-QT harvest reduces the tensile strength of the quadriceps tendon by more than a third,23 a greater initial reduction in quadriceps strength may be expected after ACLR with the QT compared to the BPTB and HT.68 Quadriceps weakness from extensor mechanism graft harvest appears most extreme during the first three months after ACLR,68 suggesting any difference in quadriceps strength between ACLR with the QT and BPTB may only be distinguishable during the first three to four months after ACLR34,68; this suggestion is supported by the fact quadriceps strength is not statistically different between the QT and the BPTB at six to 24 month follow-up.34,68,69
REHABILITATION CONSIDERATIONS
Early Phase (Postoperative Weeks 0-8)
After ACLR with the QT, the graft’s composition and fixation method should be communicated to the rehabilitation specialist, as these factors dictate the overall graft ligamentization process35,70–72; the amount of tissue trauma at the graft harvest site44; and the durability of the graft-bone tunnel construct.29–31,50,73 ACLR with the F-QT carries the risk of developing a suprapatellar hematoma55,63; pain and focal swelling at the graft harvest site is indicative of a hematoma and should be differentiated from a postoperative knee effusion.40 If a suprapatellar hematoma is identified, the surgical team should be notified as physician follow-up may be indicated.
The early restoration of passive knee extension is a crucial component of rehabilitation after ACLR, regardless of graft type.74 ACLR with the QT may carry an elevated risk of postoperative stiffness due to the larger graft size,67 presence of suprapatellar scarring and ongoing quadriceps inhibition.20,40,65,66 Interventions to improve patellar mobility, knee range-of-motion and soft tissue compliance should be implemented immediately after surgery. Failure to restore passive knee extension by postoperative week eight may indicate the need for a subsequent lysis-of-adhesions procedure.20,65
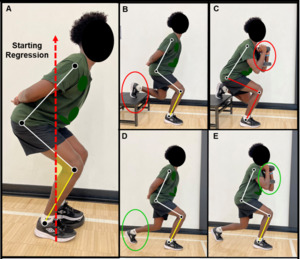
Like the BPTB, ACLR with the QT requires an isolated quadriceps training load-progression to be a cornerstone of the rehabilitation program.33,34,75,76 Early phase quadriceps rehabilitation should include quadriceps setting and other activation exercises into terminal knee extension (TKE), with the goal of restoring active knee extension as soon as possible (Table 2). The early implementation of neuromuscular electrical stimulation and/or blood flow restriction during quadriceps exercise may improve neuromuscular recruitment and help mitigate thigh muscle atrophy,77–80 as well as facilitate improvements in muscle size and strength throughout rehabilitation.81–83 The quadriceps muscle load-progression should start with quadriceps setting and straight-leg raises in non-weightbearing, and progress onto closed-kinetic-chain (CKC) positions which emphasize the restoration of knee control in weightbearing (Table 2).84 The CKC quadriceps load-progression should begin with the double-leg squat exercise and incorporate body-weight isometric and isotonic contractions in low levels of knee flexion (Figure 1A) (Table 2).85
Graft osteointegration with the B-QT supports the implementation of an accelerated resistance training approach within the first 4-6 weeks after ACLR,59 such as OKC quadriceps resistance training with distal tibial load between 0-45 degrees of knee flexion86; the combined utilization of the B-QT with interference screw fixation may further justify this clinical decision29–31,44,50,70,71,87 (Table 3). The S-QT fixated with suspensory fixation may warrant a more traditional approach to resistance training the first 10-12 weeks after ACLR59,72,73,87,88 (Table 2); healing time is needed to mitigate the risk of fixation slippage,50,73,85,89 graft laxity and bone tunnel widening with an all soft-tissue graft,17,29–31,50 as well as facilitate optimal fibrovascular integration of the graft within the bone tunnels72,87,89–93 (Table 3).
Middle Phase (Postoperative Weeks 8-16)
As goals related to joint homeostasis are achieved, the focus of rehabilitation transitions from resolving impairments in muscle activation and knee range-of-motion, to rebuilding the surgical limb’s functional capacity to manage load. Ongoing quadriceps weakness is expected after ACLR with the QT,14,15,33,34,75 and knee-specific load-progressions should be designed to best-manage the graft harvest site while stimulating improvements in quadriceps size and strength. Prior research has highlighted associations between knee position and extensor mechanism biomechanics,94–96 from which the quadriceps training load-progressions can be derived (Table 2).
As the knee moves into deeper knee flexion, preferential loading of the quadriceps tendon increases relative to the patellar tendon.94 This load-transition is the result of an improving patellar tendon mechanical advantage with a concurrent increase in passive tension within the quadriceps.94,95 Considering the laminar structure of the quadriceps tendon, variations in quadriceps length-tension can predispose the quadriceps tendon to greater levels of shear/compressive load, as well as non-uniform intratendinous force-transmission. Specifically, performing the prone knee flexion stretch will preferentially tension the superficial layer of the quadriceps tendon by maximally lengthening rectus femoris, compressing/shearing the deeper layers of the tendon95,97,98; this unique type of tendon loading can be prescribed in addition to strength training to mobilize the graft harvest site and may help stimulate quadriceps tendon remodeling (Figure 2).
Months 2-4 after ACLR with the QT, the CKC quadriceps load-progression should include isometric or isotonic contractions with a light to moderate external resistance. Initially, body weight isometric exercise in low levels of knee flexion may best manage graft harvest site irritability94,99 (Figure 1A) (Table 2). As exercise tolerance improves, the quadriceps load-progression should be advanced by monitoring the graft harvest site for any increase in pain/irritability with exercise while gradually progressing external resistance or the level of knee flexion95 (Figure 1A-D-E). The rehabilitation specialist should not advance too many variables at once, as simultaneously increasing external resistance and the level of knee flexion can exponentially load the quadriceps tendon and may provoke graft harvest site pain94,95 (Figure 1C).
Graft-specific load-progressions for the P-QT may also exist, in which more specific targeting of the superficial layer of the quadriceps tendon/rectus femoris with OKC exercise may be indicated.98,100 The long-arc-quad exercise should be advanced from active range-of-motion during the early phase of rehabilitation,85 to OKC quadriceps resistance training on a knee extension machine (Table 2); the rehabilitation specialist may elect to perform OKC quadriceps resistance training with the hip positioned in lower levels of hip flexion to preferentially load rectus femoris (i.e., performing OKC quadriceps resistance training with the trunk positioned in supine).95,97,98 External resistance should be thoughtfully progressed, as performing OKC quadriceps resistance training between 0-45 degrees of knee flexion will increase patellofemoral compartment stress and preferentially strain the reconstructed ACL graft85,86,101 (Figure 3A), whereas performing OKC quadriceps resistance training in deeper levels of knee flexion will preferentially load the quadriceps tendon and may provoke irritability at the graft harvest site94,95 (Figure 3B).
Late Phase (Postoperative Weeks 16+)
As the surgical limb develops the capacity to perform higher-load activities at slow contraction velocities, higher demand exercise progressions should be introduced. Patients participating in physically demanding activities, such as Level 1 sports, will benefit from exposure to plyometric and ballistic-type exercise progressions. The rehabilitation specialist should consider the quadriceps tendon a rate-limiting tissue for the introduction of plyometric exercise,23 as the QT harvest site must store and transfer energy during these progressions. Plyometric exercise should be initiated with knee-specific regressions that temper the demand for elastic energy-storage within the quadriceps tendon, such as running drills in triple-extension or frontal plane plyometric exercise94,102,103 (Figure 4).
As mentioned previously, specific consideration should be given for ballistic activities that require the quadriceps tendon to transfer load while in the combined position of hip extension and knee flexion, such as the wind-up phase of kicking or high-velocity running104,105 (Figure 2B); these activities combine high angular velocities and tendinous compressive/shear force by the selective-tensioning of the superficial layer of the quadriceps tendon running continuous with rectus femoris.95,97 Sagittal plane deceleration training will also preferentially load the quadriceps tendon. During deceleration, the combination of large external knee flexion moments, increasing knee flexion angles, and high-force eccentric quadriceps contractions can produce exponentially higher load-transmission within the quadriceps tendon (Figure 4); sagittal plane deceleration training must be thoughtfully progressed per exercise-tolerance and symptom-response at the graft harvest site.
RETURN TO ACTIVITY CONSIDERATIONS
Regardless of the graft type used for ACLR, most individuals expect to restore knee joint stability and function to a level that supports the return to their pre-injury activity level.106 However, only 65% of individuals may return to their pre-injury level of sports participation,107 with knee re-injury rates between 20-30% within higher-risk cohorts.108–110 Equally troubling is the unclear association between return-to-activity testing batteries and the subsequent risk of knee re-injury within various cohorts,111–117 and although the restoration of limb function on objective performance tests appears to improve return-to-sport rates,118–120 the use of performance testing cut-points as strict, medically-required, return-to-activity criteria remains controversial.112,121–123 Recent literature has highlighted the importance of shared decision-making after ACLR,124,125 to which the use of a decision-making framework may improve the return-to-activity decision-making process.124,126–129
To best inform shared decision-making, serial physical examinations and performance testing batteries should be completed throughout rehabilitation.130,131 Physical examinations should include the assessment of knee homeostasis (effusion and irritability), stability and range-of-motion.132 After ACLR with the QT, quadriceps strength testing should be a fundamental component of the performance testing battery, as quadriceps strength appears most affected by QT harvest,33,34,68 and quadriceps strength deficits are common 9-12 months after ACLR.34 Other components of a performance testing battery may include jump/hop testing and the assessment of movement quality; these tests should include both qualitative and quantitative measurements.132 Collectively, this information can be utilized throughout rehabilitation to confirm the effectiveness of exercise interventions, adjust the exercise prescription(s), and inform return-to-activity decision-making.133
Of the various data synthesized for return-to-activity decision-making, some information may be more important than others. The timeframe between ACLR and return-to-activity has been observed to be a modifiable risk factor for knee re-injury,111,134 with the suggestion that most individuals should wait a minimum of nine months before returning to unrestricted sports participation.111,122,132 Risk calculator algorithms formulated to predict the risk of revision ACLR have been recently validated for clinical use135,136; these algorithms are based upon data that is specific to the individual of interest, including age, body mass index, preoperative knee laxity, activity level and graft type.135,136 The ACL-Return to Sport after Injury (ACL-RSI) is a validated psychometric scale, and should be used to assess an individual’s psychological readiness for sports participation after ACLR.132
Comprehensive rehabilitation and return-to-sport programming can facilitate improved limb function on objective performance tests,133,137 achieve higher return-to-sport rates and reduce the risk of knee re-injury.133,138–141 Comprehensive programming should include formal strength and conditioning sessions, as well as the integration of jumping/hopping, cutting and sport-specific load-progressions. Late phase load-progressions should include a period of on-field rehabilitation with all relevant stakeholders (e.g., athlete, coach, guardian, and rehabilitation specialist) in agreement with the return-to-practice and competition progressions.131,133,142 On-field rehabilitation should follow the control-chaos continuum and facilitate graded exposure to sports participation.133,135,142,143
Prior to commencing unrestricted activity, a final physical examination and performance testing battery should be completed with all relevant information clearly synthesized for analysis within the shared decision-making framework.124–129,133 If the individual is returning to an activity with a high risk of knee re-injury, such as Level 1 sports, secondary injury reduction strategies should be implemented regardless of performance testing status.144 Pre-activity neuromuscular warmups, such as the FIFA 11+, appear highly effective at mitigating known biomechanical risk factors for anterior cruciate ligament injury,145–148 and can significantly reduce the overall injury incidence rate.149
Funding
No grant support was provided to aid in the development and publication efforts of this manuscript
Conflicts of Interest
The above authors have no financial disclosures or conflicts of interest related to the development and publication efforts of this manuscript
Acknowledgements
We extend a special thank you to Dr. George Davies, DPT, and Dr. Steven Stovitz, MD for their gift of time, mentoring, and teaching within their respective sports medicine communities.
Thank you to the physical therapists, sports scientists, and licensed athletic trainers at Training HAUS for their ongoing teamwork and support, as well as the research department at Twin Cities Orthopedics for their support with ongoing research projects.