INTRODUCTION
Patellofemoral pain (PFP) is one of the most common knee problems experienced by young adults.1 Individuals with PFP complain of retro- or peri-patellar pain during activities requiring weight bearing on a flexed knee like running, squatting, or stair ambulation.2 Powers3 has theorized that increased hip adduction, hip internal rotation, and knee abduction can cause increased knee valgus loads that stress patellofemoral joint structures.4,5 He has referred to these combined lower extremity kinematics as the dynamic quadriceps angle (Q-angle).
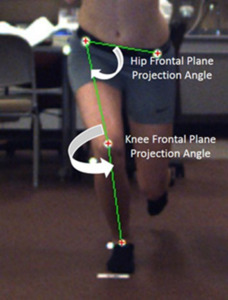
Clinicians have quantified the dynamic Q-angle by measuring the knee frontal plane projection angle (FPPA) via 2-dimensional (2-D) video analysis (Figure 1).6–8 An increased knee FPPA would suggest greater knee valgus loading.6 A limitation of this approach has been a sole focus on knee kinematics. Increased hip adduction from excessive contralateral pelvic drop relative to the femur also can increase patellofemoral joint loads.9 However, the knee FPPA does not directly account for this faulty hip movement pattern. To address this concern, Scholtes and Salsich9 developed the dynamic valgus index (DVI), a comprehensive measure combining the hip and knee FPPA. They also have reported differences in the DVI during a SLS in females with and without PFP.
Gwynne and Curran10 examined the ability of the knee FPPA during a SLS to identify subjects with and without PFP. Their findings showed that the knee FPPA had fair sensitivity and specificity. A more comprehensive measure, like the DVI, may better discriminate between those with and without PFP. Therefore, the first purpose of this study was to compare the knee FPPA and DVI during a SLS between females with and without PFP. The second purpose was to determine if the DVI better identified females with PFP than the knee FPPA. We hypothesized the following: 1) females with PFP would demonstrate a higher knee FPPA and DVI during a SLS and 2) the DVI would be more accurate than the knee FPPA in discriminating between females with and without PFP.
METHODS
Participants
An a priori power analysis was conducted using G*Power 3.1.9.711 based on published data.9 Using an effect size of .90,9 α = .05, and β = .20, a minimum of 16 subjects was required for each group. Subjects were recruited in the greater Central Savannah River Area by placing flyers on two campuses of a local university, at area fitness clubs, and at an academic medical center sports medicine clinic. Sixteen females with PFP and 16 controls participated (Table 1). Subject’s age ranged from 18 to 34 years. This age range was selected because of an increased prevalence of osteoarthritis onset after age 40.12 Inclusion and exclusion criteria were based on prior works.10,13 All subjects were recreationally active, defined as exercising at least 30 minutes three times a week for at least the prior six months. Subjects with PFP met additional criteria regarding their anterior knee pain: a) rated at least a 3 on a 10-cm visual analog scale during activities of daily living or recreation (e.g., running, walking, squatting, stair ambulation) over the previous week, b) insidious onset for at least four weeks, c) provoked by at least three of the following: during or after activity, prolonged sitting, stair ambulation, or squatting. None of the subjects with PFP had sought rehabilitation or undergone any prior movement retraining program to improve SLS mechanics. Individuals with the following were excluded from study participation: a) previous lower extremity surgery or significant injury, b) recurrent patella dislocation or subluxation, c) patella tendon or iliotibial band tenderness, and d) hip or lumbar spine referred pain. The most painful knee was tested for subjects with PFP13; controls used the limb that was determined in a random fashion. Five subjects with PFP reported bilateral symptoms. Subjects were enrolled consecutively as they met the inclusion criteria and signed an informed consent document approved by the university Institutional Review Board.
Pilot Testing
Prior to data collection, pilot testing was conducted for measuring the knee FPPA and DVI in 10 individuals who did not participate in the current study. For this purpose, these individuals were measured on two separate occasions, three to five days apart, by different examiners. Using procedures outlined below, measurement reliability was acceptable14 based on intraclass correlation coefficients (ICC [2,5]) of .88 and .89 for the knee FPPA and DVI, respectively.
Motion Analysis
Twelve-mm spherical retroreflective markers were placed on the anterior surfaces of the following landmarks9: left and right anterior superior iliac spine (ASIS), midpoint of the knee on the test extremity (midpoint of the distance between lateral and medial epicondyle measured using a tape measure), and the midpoint of the ankle (midpoint of the distance between lateral and medial malleoli measured using a tape measure) on the test extremity. Markers also were placed on the greater trochanter, lateral knee joint line, and lateral malleolus to measure knee flexion. For testing, subjects stood 2.5 m away from two cameras, one positioned in the sagittal plane and the other in the frontal plane. Subjects performed the SLS barefooted. The investigator instructed subjects to cross their arms over their chest and to squat as low as possible; they received no instruction on hip, knee, or foot position. Subjects squatted at least 50˚ of knee flexion (determined by visual inspection) to the beat of a metronome set at 40 beats per minute.15,16 They performed 3 practice and 5 test trials of the SLS. A video-based 2-D motion capture system (Simi Motion®, Unterschleinβheim, DEU), operating at 100 Hz, recorded all data.
Data Processing and Reduction
Video data were tracked and smoothed with a 2nd-order low-pass filter, using a 6 Hz cutoff frequency. Knee FPPA and DVI were measured at the point of peak knee flexion (the angle between the greater trochanter, lateral knee joint line, and lateral malleolus). The knee FPPA (Figure 1) was 180˚ minus the angle between the ASIS and mid-point of the knee and the mid-point of the knee to the mid-point of the ankle on the test limb.9 The DVI (Figure 1) was 90˚ minus the angle between the ipsilateral and contralateral ASIS and ipsilateral ASIS and the mid-point of the distal femur plus the FPPA.9 The average of the five trials for peak knee flexion angle, peak knee FPPA, and peak DVI was used for statistical analysis.
Statistical Analysis
Means, standard deviations, and 95% confidence intervals (95% CI) were calculated for average peak knee flexion, peak knee FPPA, and peak DVI. Separate independent t-tests were used to determine if significant differences existed between females with PFP and controls. Receiver operating characteristic (ROC) curves were used to determine the area under the curve (AUC) for sensitivity and 1-specificity for the knee FPPA and DVI.10 We also compared the AUC between the knee FPPA and DVI using methods described by Hanley and McNeil.17 AUC scores ranged from 0 to 1.0; a 1.0 signified perfect discrimination.10 Obuchowski18 interpreted the AUC as follows: weak (< .50), fair (.60 to .70), good (.80 to .90), and excellent (.9 to 1.0). The AUC data also had various cut-off scores with their associated sensitivity and 1-specificity values. An optimal cut-off score to distinguish between females with and without PFP was the one that would maximize the true positive and minimize the false positive rate.19 To make this determination, we used Youden’s index20 by calculating (sensitivity + specificity – 1) for each cut-off score from the knee FPPA and DVI ROC curves. The optimal cut-off score for the knee FPPA and DVI was the one with the highest Youden’s index.20 Next, we used the sensitivity and specificity for the knee FPPA and DVI optimal cut-off score to calculate positive likelihood ratios (LR+). A LR+ greater than 1 implied a positive test result would be associated with disease presence; tests with a higher LR+ would provide even greater evidence for disease presence with a positive finding.21 All analyses were conducted using IBM SPSS Statistics for Windows, Version 28 (IBM Corp, Armonk, NY, USA) with the level of significance established at the .05 level.
RESULTS
No between-group differences existed with respect to peak knee flexion. Subjects with PFP demonstrated 2.0 times higher peak FPPA and 1.3 times greater peak DVI than controls. Table 2 summarizes these data.
The AUC scores from the ROC analyses (Figure 2) for the knee FPPA and DVI were .85 [95% CI (.71, .98); p = 0.001] and .76 [95% CI (.58, .94); p = 0.01], respectively. These findings suggested that the knee FPPA had good sensitivity and specificity for discriminating between females with and without PFP.18 The DVI had a lower AUC, which can be interpreted as fair-to-good sensitivity and specificity.18 However, paired-sample area difference under the ROC curves was .07 (95% CI (-.02, .19); p = 0.10), suggesting similar AUC between the knee FPPA and DVI. The optimal cut-off score was 8.2˚ (Youden index = .56; sensitivity = 87.5%; specificity = 68.8%) for the knee FPPA and 33.6˚ (Youden index = .63; sensitivity = 81.3%; specificity = 81.0%) for the DVI. LR+ were 2.8 and 4.3 for the knee FPPA and DVI, respectively.
DISCUSSION
The purpose of this study was to 1) compare the knee FPPA and DVI during a SLS between females with and without PFP and 2) determine if the DVI better identified females with PFP than the knee FPPA. It was hypothesized that females with PFP would demonstrate a higher peak knee FPPA and peak DVI during a SLS and that the DVI would better discriminate between females with and without PFP. Findings from this study supported our hypotheses. Subjects with PFP exhibited a higher knee FPPA and DVI. The DVI also had a higher LR+ for identifying females with PFP than the knee FPPA.
Kinematics
The current findings aligned with other studies that have reported an increased knee FPPA during a SLS in those with PFP.6,7,9,10 The 13.7˚ magnitude of knee FPPA also agreed with values from prior works with values ranging from 11.5˚ to 16.8˚.7,9,10 Regarding the DVI, Scholtes and Salsich9 were the only ones to compare the DVI between females with and without PFP. Like the current study, females with PFP in their study demonstrated a significantly higher DVI than controls. Subjects with PFP in the current study exhibited an average DVI of 38.1˚ compared to 31.1˚ reported by Scholtes and Salsich.9 Although a small discrepancy existed between values, subjects with PFP had a higher knee FPPA and DVI than controls.
Gwynne and Curran10 used a ROC analysis to examine the sensitivity and specificity for using the knee FPPA during a SLS to identify subjects with PFP. They reported an AUC equal to .73, which was lower than the AUC (.85) found in the current study. Gwynne and Curran10 did not report their optimal cut-off point, which prohibited our ability to compare sensitivity, specificity, and LR+. Although the AUC for the DVI (.76) was lower, the paired-sample area difference under the ROC curves test showed equal AUC for the knee FPPA and DVI. The DVI had a higher LR+ (4.3) than the knee FPPA (2.8) in the current study.
Clinical Implications
Clinicians have used the knee FPPA to distinguish between individuals with and without PFP.6–8 Findings from the current study suggest that the DVI may be another viable approach than the more commonly used FPPA. However, caution must be taken using results solely from hip and/or knee kinematics during a SLS to diagnose those with PFP. Thus, clinicians should consider other sources of anterior knee pain like patellar tendinopathy, patellar instability, and plica syndrome.22
The current results show that females with PFP exhibit a higher DVI during a SLS, which may reflect decreased hip and knee neuromuscular control. Recent findings have shown improvements in the DVI for those with PFP following a movement retraining intervention.23,24 Assessing the DVI may be better than the FPPA when deciding to implement movement retraining because it incorporates both hip and knee movement. However, this conclusion is speculative and additional investigations are needed to make this determination.
Limitations
This study has limitations that deserve attention. First, only females participated, which limited extrapolation of results to males. Second, the knee FPPA and DVI was only assessed during a SLS. Subjects with PFP who did not exhibit a higher knee FPPA and DVI during a SLS might have done so during other dynamic tasks like sit-to-stand transitions and stair ambulation. Finally, PFP is a multifactor problem with various impairments; not all individuals with PFP may exhibit an increased dynamic Q-angle. Clinicians must consider other impairments such as strength, flexibility, and overuse when examining this patient cohort.22
CONCLUSION
In summary, 2-D motion analysis is useful for identifying females with PFP who exhibit altered lower extremity kinematics. Although clinicians have primarily used the FPPA, the DVI may be useful because it accounts for altered hip and knee movements, both of which can contribute to increased knee valgus loading. Additional studies are needed to further examine the usefulness of the DVI in discriminating between multiple sources of anterior knee pain.
Funding
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R15AG063105. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Human Subject Approval
This study was approved by the Augusta University Institutional Review Board #1480126.
Conflicts of interest
The authors report no conflicts of interest.
_curve_for_identifying_females_with_patellofemoral_.png)

_curve_for_identifying_females_with_patellofemoral_.png)