BACKGROUND AND PURPOSE
Meniscal injuries are common, with an annual incidence of 79 injuries per 100,000 individuals aged 15–40 years, men and the medial meniscus (compared with the lateral meniscus), is most commonly affected.1–3 Although the diagnosis is made through history and clinical examinations, this lesion type is challenging and usually requires magnetic resonance imaging (MRI) for confirmation.4 Surgery is often the treatment of choice, and for many years, it has been a standard practice for surgeons, with total or partial removal of the affected menisci to mitigate the clinical symptoms arising from meniscal injuries.5–7 In 2014, 516,800 meniscectomies were performed in the United States alone, generating an annual cost of US $ 4 billion.8,9
These paradigms have undergone changes because surgical procedures do not present greater benefits than conservative treatment, when analyzed through surgical recurrences and development of knee osteoarthritis (OA) after meniscectomy.2,5 Therefore, surgery should not be the first option, and accordingly, in recent years, the number of surgical procedures has reduced.10–14 Englund et al.15 and Chirichella et al.16 pointed out that conservative treatment remains one of the pillars for the treatment of meniscal injuries, particularly in stable meniscus tears, to preserve this tissue whenever possible. Through a systematic review and meta-analysis, Swart et al.17 assessed the effectiveness of exercise therapy for the treatment of patients with meniscal injuries and concluded that exercises were comparable to meniscectomy in terms of pain, function, and knee performance outcomes. However, exercise therapy showed higher value related to short-term strength gain, making it more effective. In addition, patients who underwent exercise therapy showed better pain and knee function outcomes, both before and after meniscectomy surgery, than patients who did not undergo exercise.
Currently, the isokinetic dynamometer is an accepted resource for the conservative treatment of the locomotor system, and is useful for evaluation and strength training, especially for knee injuries.18,19 Isokinetic exercise for strength training is characterized by constant velocity that accommodates the individual’s muscular work throughout the range of motion (ROM).20 Testing can provide objective outcomes related to power, total work, and peak torque, which can be represented as a percentage when normalized to body mass.21 Another way to explore isokinetic results is to divide the ROM into three components: time to reach velocity, load range (LR), where the specific velocity set is sustained, and deceleration time. These distinct phases can provide additional information, such as reaction time and ability to maintain velocity, which may assist in the clinical evaluation and implementation of specific treatment protocols to optimize treatment.22
In a study by Belhaj et al.,23 patients with meniscal injuries received classical conservative and isokinetic interventions to increase muscle strength in the quadriceps and hamstrings. They reported improvements at the end of the treatment and the highlighted the importance of the intervention to conserve the meniscus, demonstrating the isokinetic dynamometer as a resource to be used not only for evaluation but also in treatment. However, no studies have investigated an intervention protocol “with emphasis” on the use of the isokinetic dynamometer for strength training in individuals undergoing conservative treatment after meniscus injury. Thus, this case report aimed to describe the effects of isokinetic training and neuromuscular/proprioceptive exercise program on muscle performance and physical function in an individual after a rupture of the posterior horn of the medial meniscus.
Subject Characteristics
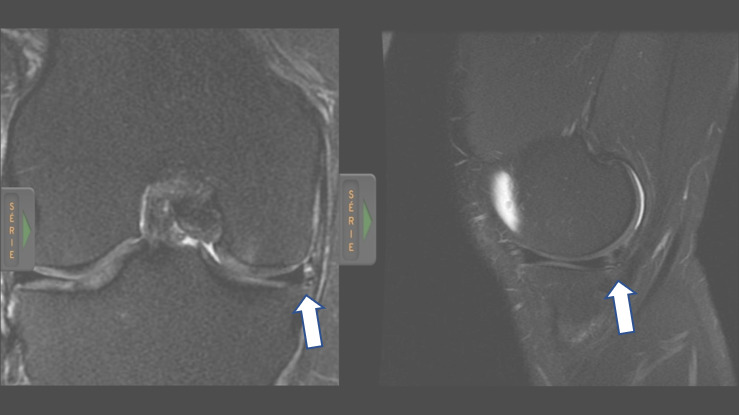
A 40-year-old man with a body mass index of 27.8 kg/m2 was referred for evaluation at the Laboratory of Biomechanics and Clinical Epidemiology of the University Hospital/UEL. During a soccer match, he suffered a contact injury of the right knee, clinically diagnosed as a meniscal tear. The MRI results indicated medial and lateral patellofemoral and tibiofemoral chondropathy, vertical/oblique rupture with a horizontal component characterized on the periphery of the posterior horn of the medial meniscus, and tendinopathy of the semimembranosus. From this, an exploratory meniscectomy was proposed by the surgeon responsible for the case; however, the patient opted for conservative treatment.
The treatment plan consisted of 22 sessions of isokinetic and neuromuscular/proprioceptive training over the course of 11 weeks. Muscle performance and physical function were assessed before and after treatment, and at a six-month follow-up. The participants (the subject and the matched control) signed an informed consent form and the study was approved by the IRB (#00768812.0.5231). The use of uninvolved limbs after musculoskeletal injuries as a control is not desirable, as this limb may be compromised. In order to avoid any interference, the authors chose to invite an athlete with similar anthropometric characteristics to participate and serve as a control for strength data.
OUTCOMES
Initial Examination/Clinical Measures
Initially, an examination was carried out - one month after the injury (personal data, history of the injury, and physical examination), followed by the Apley and McMurray tests and ligament analysis: the Lachman, anterior drawer, Slocum, varus and valgus stress, and Pivot Shift tests. More information is available in the Supplementary Material (#1).
Physical Function
The Lower Extremity Functional Scale (LEFS) was used to assess functional activities. This questionnaire consists of 20 items with gradual responses from 0 to 4 points, with a maximum score of 80 points. The higher the score obtained, the better the participant’s reported function. The cut-off for clinically meaningful improvement is 11 (area under the receiving operator curve = 0.96; 95% CI [0.88;0.99]).24 The patient’s LEFS scores were 74 points at the initial examination, 72 points after treatment, and 76 points at the six-month follow-up, with no limitations on activities of daily living.
Muscle performance – Dynamometry
Muscle performance of the quadriceps and hamstrings was assessed using the Biodex System 4 (Biodex Medical System Inc., Shirley, NY, USA) in a concentric mode at angular velocities of 60, 120, and 300 °/s, with a sampling frequency of 100 Hz (Video Supplementary Material #2). The participant was instructed to not perform any physical activity on the testing day. First, the patient completed a 10-min warm-up on a cycle ergometer, without resistance, at a speed of 30 km/h. Then, a familiarization process was conducted which consisted of two sets of 10 repetitions (in each velocity).25 (Video Supplementary Material #2)
The individual was positioned on the dynamometer seat and stabilized with straps around the trunk, pelvis, and thighs per Biodex protocol. Hip flexion was adjusted to 85 °, the dynamometer axis was aligned with the lateral femoral epicondyle, and the ankle pad was positioned just above the medial malleolus.26 Active ROM (AROM) of 90 ° for flexion and 0 ° for extension was chosen for testing. However, the extension ROM was defined according to individual limits. All calibration and gravity correction procedures followed the manufacturer’s instruction manual.27 Five repetitions at each test velocity were performed with a rest interval of 90 s between sets. The participant was instructed to perform at maximum strength during all repetitions, and verbal encouragement and visual feedback were provided. For reliability purposes, a variation coefficient of <10 % for each series was considered acceptable.28
The peak torque/body mass (PT/BM) and Hamstrings:Quadriceps ratio (H:Q) were calculated only during the portion of sustained velocity (load range phase). The raw data were extracted using Biodex software and further processing was performed using a specific Matlab® algorithm to accomplish this calculation. Average values of the five repetitions were calculated for all variables at each velocity. The percentual of sustained velocity was calculated in relation to the total ROM.
To create the torque-angle-velocity relationship or surface maps (TAV3D), the mathematical “surf” function of Matlab® was used. All five repetitions of each velocity were interpolated according to the phase duration. The algorithm estimated the intrinsic geometry considering the torque (z axis), the joint angle (x axis), and the speed (y axis) in the same time interval. The z axis defined the height of the map in relation to the force intensity, while the x and y axes formed the surface boundaries. Qualitative analysis with TAV3D surface maps improves the interpretation of the test results, making it possible to observe the interaction between torque, velocity, and range of motion. This interpretation can be added to the other results of isokinetic tests, as the assessment of movement or functional activity could contribute to the decision making and treatment (Supplementary Material #3).29,30
INTERVENTION
Based on the history of the injury, isokinetic measures, and functional status of the lower limb, new neuromuscular/proprioceptive training and an isokinetic strengthening program were considered the ideal treatment for this patient. It was expected that there would be improvement in neuromuscular control after the proposed training.
Innovative Intervention
The treatment plan and regimen were distributed among 22 sessions, over 11 weeks. Each treatment session was divided into three components: 1) re-assessment and analysis of the clinical condition; 2) warm-up and strength training with the isokinetic dynamometer, according to the stipulated weekly program, based on the evolution and clinical signs presented; and 3) proprioceptive and stretching exercises on Flymoon® (Figure 2) as described in Table 1. The Flymoon® proprioceptive training intervention consisted of eight proprioceptive and two active stretching exercises (table 2). All movements were performed in three sets of 30 s each.
The velocity-specific training at 300 °/s was used as a warm-up and power training. It started with 70 % of the maximum force (according to initial evaluation – using visual feedback from the isokinetic screen), with 25 repetitions. In addition, the 120 °/s angular velocity was used in the first weeks for explosive power, with 15 repetitions. This first stage continued until week 3.
From week 4 on, the load was increased to 80 % of maximum force for both velocities. From week 8, the velocity of 300 °/s was used only for the warm-up, 120 °/s was maintained (with 90 %), and 60 °/s was introduced with 60 % of the maximum force. Contractions at slower velocities were applied to align with near maximum tension development.31 At week 9, there was a 10 % increase in strength (to 80%) at 60 °/s velocity, which continued in weeks 10–12. The patient finished the protocol performing 15 reps at 90 % (120 °/s) and 10 reps at 80 %, for three sets (60 °/s).
The training program carried out with Flymoon® followed the exercises described in Table 2, consisting of proprioceptive exercises and active stretching (Video - Supplementary Material #2). All movements were performed in series with activities per minute or for a number of repetitions during all treatment sessions. Sessions were supervised by a licensed physical therapist. In addition to proprioception, Flymoon® encourages neuromuscular control by creating an unstable surface that challenges the proprioceptive system to respond and adapt to the changing conditions; it can be adjusted in degrees of difficulty and can be used in different planes of movement. The equipment allows the challenges of ROM in the ankle, in addition to working the fascia in multiple directions. When standing on the Flymoon®, the principle of biotensegrity is triggered: putting tension on the feet and maintaining this tension while performing movements seems to provide a stimulus for stability in the knee.32 The greatest support occurs between the hallux and the first metatarsals, which activates the anterior deep line. By keeping this line activated, hyperextension (recurvatum) can be avoided.
RESULTS
The anthropometric characteristics of the patient were: 40 years-old and BMI of 27.8 kg/m2 and the individual used as a control: 40 years-old and BMI of 21.8 kg/m2. Table 3 shows the % of sustained velocity (LR) normalized by ROM, values of PT/BM, range of motion, and agonist/antagonist ratio at angular velocities of 60, 120, and 300 o/s for extension and flexion of both knees, involved and uninvolved, of the patient with meniscal injury in the pre, post, and follow-up period and in the control individual. The TAV3D figures are available in the supplementary material #3A and 3B.
DISCUSSION
The results demonstrate a lower PT/BM value in the extensors pretreatment at all velocities, 60, 120, and 300 °/s in relation to the control, while the same was not observed for flexion. This muscle weakness in the knee extensors is expected in patients with medial meniscal lesions because after an injury, the quadriceps muscle can be affected by neural inhibition, commonly described as arthrogenic muscle inhibition, which results from changes in sensory information related to pain, inflammation, and damage to mechanoreceptors. This reduces strength, which negatively affects movement patterns, contributing to the reduction in joint and postural stability.33–38 Therefore, it has been suggested that intervention be initiated early because the association between meniscal changes combined with knee extensor muscle weakness results in more severe joint changes, such as knee osteoarthritis.39–41
However, at the end of the intervention, the PT/BM value increased in both flexion and extension, at different velocities, in relation to the control and baseline. These findings can be attributed to the isokinetic training program because isokinetic exercise is a muscle-strengthening modality that can enable the development of maximum tension by the muscles at all joint angles during ROM, as it is performed at constant velocity, recruiting the largest number of muscle fibers and thus offering greater muscle performance.42,43
Regarding the muscle H:Q ratio, improvement was seen after treatment compared with that before the treatment by 13.3 % (64.7–78 %) and 6.6 % (68.4–75 %), respectively, at velocities of 60 and 300 °/s. The imbalance in the agonist/antagonist muscular strength ratio may increase the likelihood of injury.44 Numerous factors are presumed to influence the ratio, for example, age, sex, limb dominance, physical activity, movement velocity, and functional demands of the patient.45
In the ROM results (Table 3) for extension and flexion, the values obtained before treatment were higher in the patient than in the control, with approximately 8 ° of difference (before ≅ 8 °) at all velocities. These data must be viewed with caution because of the learning factor since the control was only exposed to the dynamometer once. This slight ROM increases may be related to the recovered strength of the quadriceps.46,47
Overall, these findings suggest that isokinetic variables may be more related to the functional status or capacity knee than to the capacity to generate strength because the control individual had better segment functional capabilities than the patient with meniscal injury, who stood out for demonstrating a predominance of strength. However, in the torque–angle–velocity relationship/surface map (Supplementary Material #3A and 3B), which provides a qualitative analysis, the patient had greater capacity to sustain torque, higher torques at different velocities in both the flexors and extensors, generating greater torque at the end of the movement than the control, with higher values after treatment and at 6 month follow up in relation to baseline.
The limitations of this study include the lack of assessment of muscle eccentric capacity and proprioceptive measure. Future studies involving patients with a partial meniscal tear should include isokinetic muscle training as well as neuromuscular/proprioceptive exercise program.
CONCLUSION
The results of this case report demonstrate that 11 weeks of isokinetic muscle training and neuromuscular/proprioceptive exercises led to an increase in the PT/BM for the knee extensors and flexors at different velocities in the included subject. These results indicate that isokinetic dynamometer training may play a role in muscle training for patients with meniscus injury.
Funding
The authors wish to thank the FINEP (MCT/AÇÃO TRANSVERSAL PRÓ-INFRA #01/2007 / #01/2009) for the funding to obtain the isokinetic dynamometer. KO and MFS received doctoral financial support from CAPES (Funding Code: 001). JRC also thanks the CNPq for his productivity scholarship.
Conflicts of interest
The authors report no conflicts of interest.