INTRODUCTION
Shoulder pain in the overhead athlete has frequently been associated with anterior instability, superior labral anterior to posterior (SLAP) lesions, internal impingement, and rotator cuff pathology.1 Posterior shoulder instability (PSI) of the glenohumeral joint as a potential cause of shoulder pain in tennis players is rarely discussed.2 PSI symptoms typically occur in combinations of flexion, horizontal adduction, and internal rotation (IR) which challenge the posterior labrum, capsule and rotator cuff.3,4 The dominant arm of tennis players is frequently subjected to high forces in these combined positions during the follow-through phase of a forehand, preparation for a backhand, backhand volleys, and kick serves.5 This repetitive motion may induce microtrauma and lead to symptomatic posterior translation of the glenohumeral joint which may be associated with capsulolabral, muscular and bony structural lesions.3
The aim of this clinical commentary is to present an overview of the classification, aetiology, clinical presentation, and treatment of micro-traumatic PSI, with a particular focus on tennis players.
Incidence
PSI in the general population is often missed and therefore underdiagnosed.3 The estimated incidence according to data from emergency and trauma settings suggests that PSI accounts for 2 and 3% of all shoulder instabilities.6 This is likely underestimated since only 23 % of traumatic posterior instabilities require reduction.7–9 The incidence of micro-traumatic and atraumatic PSI is even more elusive as small subluxations are easily missed by clinicians, who mistake secondary pathology, such as rotator cuff pathology, internal impingement and acromioclavicular joint pain, as the primary diagnosis.10 The delay in correctly diagnosing and appropriately managing symptomatic PSI has the potential to sideline young tennis athletes for an extended period,11 interrupting circuit tours, impacting contractual arrangements,12 and affecting physical conditioning13 and mental wellbeing.14,15
Classification
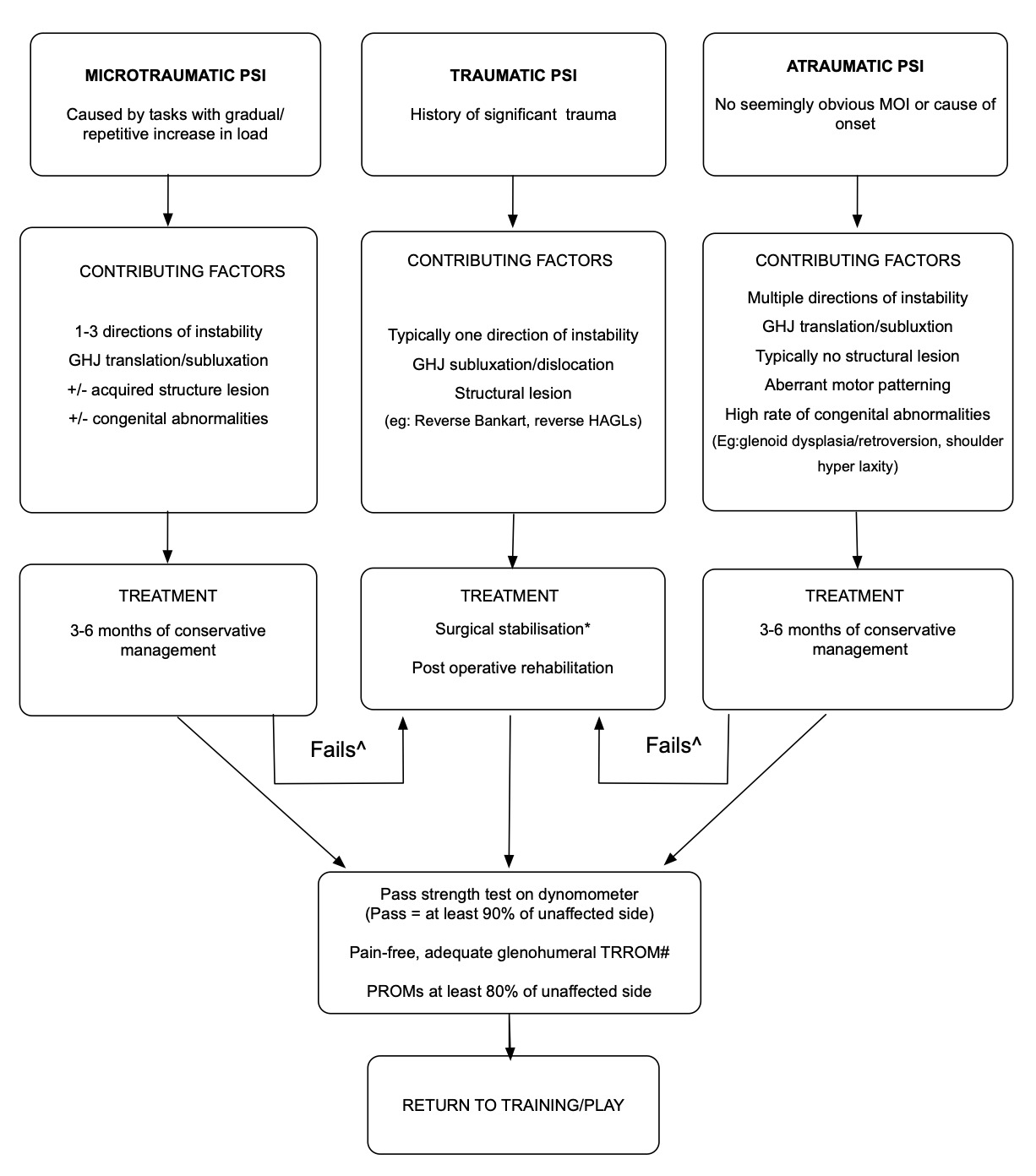
A consensus via Delphi process was recently reached for classifying PSI.16 Shoulder experts agreed on three subgroups: traumatic, atraumatic, and micro-traumatic, linked to a cluster of typical associated factors.16,17 (Figure 1) Traumatic PSI is associated with a significant history of trauma, glenohumeral joint dislocation and structural lesions such as reverse Bankart lesions and reverse humeral avulsion of the glenohumeral ligament (HAGL). Atraumatic PSI has no seemingly obvious mechanism of injury or cause of onset and is typically associated with multiple directions of instability, a high incidence of congenital factors (e.g., glenoid dysplasia, glenoid retroversion, shoulder hyperlaxity), subluxations, a lack of structural lesions and aberrant motor patterning. Micro-traumatic PSI is caused by tasks with a repetitive or gradual increase in load, such as months of continuous tennis with a heavier than usual racquet.18 This sub group, may or may not have congenital factors contributing to their presentation and could acquire structural lesions due to repetitive forces imposed on the shoulder.
Aetiology of PSI in the overhead athlete
Mechanism of injury
PSI in baseball batters (known as “batter’s shoulder”)19,20 and other throwing sports 3 has been previously described and attributed to the extreme forces imposed on the posterior glenohumeral joint during the deceleration phase of a swing or throw. In baseball, the combination of rotational velocity transferred from the lower limb to the shoulder pre-swing (up to 937⁰ .s-1 at the shoulder) and linear bat velocity (31m/s) along with the mass of the bat needs to be counterbalanced by the posterior glenohumeral joint capsule and rotator cuff (to resist distraction, horizontal adduction and IR of the shoulder) during arm deceleration.21 These high decelerative loads, performed repetitively may deform or damage the posterior capsulolabral complex and rotator cuff - structures that normally function to limit posterior humeral head translation.1,21 This mechanism can lead to micro-traumatic PSI in the setting of overtraining, muscle imbalances and/or shoulder congenital abnormalities.2,22,23 The dominant arm of tennis players is frequently subjected to decelerative forces during the follow-through phase of a forehand, preparation for a backhand, backhand volleys, and kick serves.5,24 The rotational velocities associated with tennis, especially serving, may be even higher (3000⁰.s-1)5 than demonstrated in baseball batting, suggesting that stress to the posterior capsulolabral complex and rotator cuff, and therefore risk of PSI, may be even greater in tennis players.
Passive Structures
The posterior capsule becomes taut in positions of flexion, horizontal adduction and IR.25 Deformation or stretching of the posterior capsulolabral complex due to the repetitive mechanical stress and load of tennis may result in greater humeral head posterior translation during these movements.
Although not pathological, the presence of shoulder hyperlaxity may predispose players to posterior instability.26–28 Shoulder hyperlaxity may be present in 13% of sports men and up to 42% of sportswomen.29 It is important to distinguish laxity from instability. Hyperlaxity is an increase in joint translation due to elongation of soft tissue structures and is asymptomatic. Instability is when translation is not controlled by the sensorimotor system and is symptomatic.30 Ligament laxity might precipitate a decreased stimulation of proprioceptive afferents in the shoulder, reducing efferent muscle control.31,32 This phenomenon is likely to lead to instability in the presence of microtrauma.26
Glenohumeral internal rotation deficit (GIRD) has been associated with shoulder pain in the overhead athlete and posterior capsule stretching commonly recommended to increase IR range of motion.33 However the link between the soft tissue and bony adaptations of the overhead athletes’ shoulder and the incidence of shoulder injury has yet to be firmly established,34 particularly in tennis players. A thickened or stiff (reduced elasticity) posterior capsule in the dominant compared to the non-dominant shoulder is a normal finding in asymptomatic shoulders of overhead athletes and may be an advantageous adaption to further protect the glenohumeral joint against the large deceleration forces of a swing or throw.35–37 GIRD is typically associated with a thickened or stiff posterior capsule,38 and is also a normal adaption in overhead throwing athletes if it is accompanied by a concomitant increase in external rotation (ER) to maintain the total rotational range of motion (TRROM- the sum of internal and external rotational range of motion) similar to the non-dominant side.39–41 A TRROM loss of more than 5 degrees on the affected side compared to the TRROM of the other has been suggested as potentially problematic,42 however significant differences in TRROM between dominant and non-dominant sides can be present in tennis players with asymptomatic shoulders.43 Humeral torsion (the rotation of the humerus that is a normal adaptation to those exposed to overhead throwing type sports) will also have an effect on range of motion measures44 and has been shown to correlate with the presence of GIRD in asymptomatic baseball pitchers.45 When IR range of motion is corrected by accounting for humeral torsion (using ultrasound), GIRD is often no longer present, indicating that soft- tissue tightness is unlikely to be responsible for the reduced IR that may be found clinically in baseball pitchers.46 Comparable findings may be present in tennis players given the sporting similarities of overhead, high force, and repetitive use of the dominant arm.
Care must be taken not to misinterpret PSI for GIRD or a tight posterior capsule. In some cases of micro-traumatic PSI, IR and horizontal adduction range of motion can appear limited due to muscle guarding and /or pain as an attempt to limit positions of vulnerability.47 Prescribing posterior capsule stretches (e.g. sleeper or cross body adduction stretches) in such cases can be detrimental to recovery as these positions (i.e. shoulder flexion, horizontal adduction and IR) not only aggravate symptoms of PSI but may contribute to further unwanted elongation of glenohumeral joint passive structures.41,48 Conversely, PSI can present with an increase in horizontal adduction and IR range of motion, with pain at end of range due to a voluminous or elongated posterior capsule with concomitant pathological posterior humeral head translation.26,49
Glenoid
Glenoid retroversion (a glenoid facing more posteriorly), glenoid hypoplasia/dysplasia (under-development of the posterior inferior glenoid rim) and glenoid bone erosion are statistically significant risk factors for developing PSI.50–53 Glenoid retroversion angles can vary within a normal shoulder population, though most authors agree that a retroversion angle of 10 or more degrees would be considered excessive (Figure 2a).53,54 The degree of glenoid version is considered to be largely genetically determined in the general population,55 however repetitive overhead use of the arm before the age of 12 years (prior to the development of secondary ossification centers) could impact glenoid development.56 Recent evidence57 identifies an increased incidence of posterior glenoid dysplasia in adolescents who participate in demanding unilateral upper limb sports (such as baseball or tennis).
Posterior humeral head subluxations can cause glenoid erosion due to shearing of the humeral head across the posterior glenoid rim which can further progress PSI (Figure 2b).17 These anomalies further reduce bony contact between the humeral head and the glenoid predisposing to a loss of humeral head control, particularly in unilateral upper limb dominant sports such as tennis.
Scapula
In tennis, optimal function of the scapular muscles is required to transmit potential energy generated from the lower extremities to kinetic energy in the upper limb. Any aberrant motion of the scapula increases the potential for injury through compensatory mechanisms.59 Aberrant scapular motion, particularly reduced upward rotation, has been implicated in shoulder pathology in the overhead athlete.60–64 A lack of scapular upward rotation reduces the relative contact area of the humeral head on the glenoid, especially as the arm elevates into overhead positions, contributing to less bony stability and the potential for subluxations through range.65,66 A reduction in bony congruency between the glenoid and the humeral head places additional strain on the surrounding passive structures and inhibits the optimal length-tension relationship of the rotator cuff muscles67,68 - all of which affect the concavity compression mechanism of the humeral head on the glenoid. In tennis players, serving induced upper limb muscle fatigue has been shown to significantly reduce scapula upward rotation compared to pre-training position,69 which has implications for monitoring serving loads.
The scapular stabilizers have been shown to contribute up to 50% of the force generated in shoulder external rotation.2,3,70 A reduction in scapular stability may place excessive strain on the rotator cuff muscles and/or affect the amount of force the external rotators can generate which will not only affect shoulder performance but may reduce the active support to the posterior humeral head.26 It is unknown if aberrant scapular motor patterning is a cause or effect of glenohumeral joint instability,71 however previous studies have shown that in asymptomatic overhead athletes, a lack of upward rotation is associated with developing shoulder pain.72
Muscle Control and Strength
Weakness in the external rotators of the shoulder has been demonstrated in throwing athletes with shoulder pain potentially due to overload and fatigue of the posterior musculature (supraspinatus, infraspinatus, and posterior deltoid).73–75 Increased tension of the suprascapular nerve, which can occur in late cocking phase of a serve (maximal external rotation), has also been muted as a potential cause of weakness for the external rotators.76
The posterior cuff (supraspinatus, infraspinatus and teres minor) in combination with posterior deltoid provide a mechanical buttress to the posterior aspect of the glenohumeral joint.26 Any weakness in these structures could allow the humeral head to translate posteriorly in movements of flexion and horizontal adduction placing greater tensile loads on the posterior structures such as posterior capsuloligamentous complex, labrum, and posterior rotator-cuff.
A deficiency in the kinetic chain may result in overload of distal segments.77 The leg and trunk segments of the body are considered to be force generators as well as the stable base for distal mobility; with their integrated function considered to represent core stability.78 In a normally functioning kinetic chain, leg and trunk segments develop 51 to 55 % of the kinetic energy and force delivered to the hand, with the shoulder producing only 13% of the entire kinetic energy of the service motion.78 Thus, a deficit in core stability is likely to affect the force contribution at the shoulder, which will overload glenohumeral joint structures. Specifically, Elliot and colleagues79 found that a reduction in knee flexion during the cocking phase while serving resulted in a 17% increase in load at the shoulder if ball velocity was to be maintained.
Clinical Presentation
Symptoms of PSI may include vague or sharp posterior shoulder pain due to the posterior humeral head abutting the posterior cuff, capsule and labrum80 (Table 1). Anterior shoulder pain is commonly present, potentially due to compression of the top edge of subscapularis and biceps long head as the humeral head translates posteriorly.26 Players with PSI frequently present with multiple sites of rotator cuff pain (posterior, anterior, superior and/or lateral). Impingement symptoms (internal and subacromial) may also be present. The impingement is secondary to pathological posterior translations and poor scapular mechanics, but often diagnosed as the primary condition.81 Reports of pain are more common than frank dislocations or subluxations,20,26,82 although subluxations may be evident on examination. A decrease in upper limb power generated during any phase of the tennis swing is often reported.19
Typically, players will report a history of microtrauma that precipitated their symptoms.16 This may include an increase in the load (e.g., number of serves particularly associated with going deep into tournaments/winning matches, training frequency, volume, new technique, racquet weight24) or similarly a significant reduction in load and then a resumption of activity, such that may occur after illness. Players should be questioned regarding any history of shoulder trauma (such as a backhand or kick serve with a sudden awareness of pain) that may indicate structural damage to the shoulder. If the patient reports a significant shoulder trauma in the history, imaging is warranted.68,83,84
Physical Examination
The posterior apprehension test, Kim, and Jerk tests are provocative manoeuvres that have been traditionally described for diagnosing PSI.85 The posterior apprehension test has high specificity (sensitivity: 19.2%, specificity: 99.2%,) when apprehension is used as a criteria for a positive result86 and the Kim test (sensitivity: 80%, specificity: 94%) may have some clinical utility in diagnosing patients with posterior labral lesions.87 The O’Brien test (sensitivity: 83%, specificity: 25%) may also have some clinical value in diagnosing posterior labral tears in young, noncontact overhead athletes.87,88 The posterior drawer test may be used to detect posterior laxity though are not necessarily diagnostic of PSI (sensitivity: 42% specificity: 92% for instability).89,90 The sulcus test may indicate rotator interval laxity77 or inferior glenohumeral instability (sensitivity: 28-72%, specificity: 85-97%)91 if the test produces symptoms of instability.92 In a recent Delphi study, Sadi and colleagues16 reported that examiner agreement was reached on a selection of tests to use for diagnosing micro-traumatic PSI (the posterior apprehension test or jerk test, subjective history, and symptom improvement with humeral head correction) though note that these tests have never been studied in a cluster. Sensitivity and specificity values for shoulder tests should be interpreted with some caution given that positive and negative likelihood ratios with confidence intervals (often lacking in studies that examine shoulder tests) are a truer reflection of a test’s ability to detect a health condition.93
Although the provocative manoeuvres may have some clinical utility in diagnosing patients with PSI, most (i.e., Kim and Jerk tests) have only been validated in patients with structural lesions and/or use the presence of glenohumeral joint subluxation and apprehension as a positive result (i.e., posterior apprehension test). Given the aetiology of PSI in the overhead athletes is often micro-traumatic, with patients commonly presenting with pain rather than subluxations and frank dislocation,20,26,82 these tests used in isolation have the potential to miss non-structural posterior humeral head translation which is still pathological.10,20
Given that aberrant motor control of the scapula and humeral head are often contributing factors to PSI, assessing active and loaded movement strategies in association with symptoms can provide valuable information to the clinician and assist with treatment decisions. At a minimum, active flexion and abduction range of motion should be assessed to determine the presence of scapular dyskinesia and aberrant humeral head translations. The therapist might observe a lack of scapular upward rotation at rest and through range of motion, and possibly some scapular medial rotation (winging) compared to the unaffected side. Scapular medial rotation may be a compensatory strategy to place the glenoid under the humeral head during movement in the sagittal plane as an attempt to increase bony stability.47
The presence of posterior humeral head translation should be assessed through combinations of active flexion, IR, and horizontal adduction. Humeral head translations may range from observable and obvious subluxations to subtle increases in posterior humeral slide on palpation associated with symptoms. Range of motion may appear “blocked” due to subluxation of the humeral head off the back of the glenoid or deficient motor control preventing smooth articulation of the humeral head on the glenoid fossa through range.47,94 More provocative tests may be needed to assess posterior humeral head translation under load47 in the elite tennis player, such as loaded external rotation in the horizontal adduction plane, or any other position that mimics the players’ position of aggravation.
The Effect of Correction
Once the presence of aberrant scapular motion and/or posterior humeral head translation has been established, the effect of correction of the scapula and humeral head can be used to i) confirm the diagnosis, ii) determine if the patient will respond to rehabilitation and iii) what type of exercise strategies to employ.
The effect of manual correction involves the therapist choosing an objective test and noting the patient’s faulty scapular and/or humeral head biomechanics during that test in association with symptoms.47,94,95 The clinician then applies manual correction of the scapula (Figure 3), humeral head (Figure 4a and 4b) and possibly a combination of both to correct the faulty mechanics while reassessing the test, noting any improvements in range of motion, pain, subluxations/dislocations, and/or strength on reassessment.
For the effect of scapular correction, the therapist typically corrects the scapula by placing one hand under the axilla (often to achieve increased upward rotation and/or elevation), while using the other hand to guide the medial boarder of the scapula through the corrected range of motion (or apply the resistance during a special test) (Figure 3). For the effect of posterior humeral head correction, the therapist uses the pad of their thumb/s on the posterior glenohumeral joint line to prevent the humeral head gliding excessively posteriorly during reassessment of a test which is typically active flexion, (Figure 4a) or horizontal adduction (Figure 4b). A positive corrective test should be at least 20° improvement in active range before symptoms, or an improvement in strength and/or pain on a loaded test.96
Scapular corrective techniques have good inter-rater reliability (reliability coefficients ranging from 0.53 to 1.0).97–99 and variations of scapular assistive manoeuvres have been previously published by a number of authors for different shoulder pathologies. Kibler61 describes the scapular assistance and scapular retraction test for scapular dyskinesia. Watson describes corrective techniques in atraumatic47,100 and multidirectional shoulder instability,95 and Lewis97 discusses the shoulder symptom modification procedure. The effect of supporting the posterior humeral head during active range of motion has been previously described by Watson in PSI47 and MDI94,95,101,102and by Boiletee and colleagues (the Thumb assistance test) for PSI.103 While correction of the anterior humeral head has good inter-rater reliability (sensitivity: 63.89%; specificity: 98.91%),104 the psychometric properties of posterior humeral head correction have yet to be evaluated.103 Irrespective of the corrective method used, the aim of shoulder assistive techniques should be to determine which position produces the largest reduction in symptoms for the patient.
The effect of correction can be used to determine if aberrant scapular motion and posterior humeral head translation are contributing to the patient’s symptoms as well as assist in differential diagnosis.47,61,103 For example, apparent restrictions in horizontal adduction and/or IR range are common findings in PSI and patients may be misdiagnosed as having a tight posterior capsule and/or GIRD.46 If therapist-assisted support of the humeral head to prevent posterior translation improves range of motion (Figure 4), then pathological capsular restriction is unlikely to be a contributing factor to the patient’s presentation.47,103
Similarly, the findings of tests for ‘impingement’ and SLAP tears may change. For example, although the O’Brien’s test can be diagnostic of a SLAP tear,105 if correction of the posterior humeral head improves symptoms, then posterior humeral head translation may be contributing to a positive O’Brien’s test, and not necessarily a structural lesion. Manual corrections also assist in exercise selection. If a patient’s objective tests improve with upward rotation of the scapula, then scapular upward rotation is the motor strategy to retrain.
The ability to ameliorate symptoms in these functional provocation positions can also indicate if further investigation with imaging is required (if not already performed) and if the patient is likely to respond to rehabilitation. If manual corrections do not prove effective, a structural lesion of significance may be a larger contributing factor to the patient’s pathology. If a structural lesion of significance is suspected, early referral for imaging may be warranted. Alternatively, if the therapist suspects that rotator-cuff tendon reactivity
Imaging
MRI is the gold standard when assessing capsular and labral integrity associated with PSI.106 MRI scanning without contrast has been used to successfully diagnose most cases, but MR arthrogram may be required for subtle lesions. A significant proportion of tennis players with micro-traumatic PSI will have an absence of significant structural lesions on MRI, indicating that loss of humeral head motor control and/or excessive capsular laxity107 may be contributing to their symptoms. Posterior labral tears, avulsion of the posterior band of the inferior glenohumeral ligament, reverse Bankart lesions and muscle atrophy may be found in players with a history of trauma or longstanding symptoms.77,107,108 Labral lesions may not be isolated to the posterior aspect of the glenohumeral joint and may extend to the anterior and/or superior labrum which has been shown in up to 47% of cases in a cohort of young, active military cadets presenting with PSI.11
Rotator cuff tendinopathy and partial articular surface tears (PASTA) of the supraspinatus and/or infraspinatus are commonly observed on MRI in patients with PSI as poor scapula mechanics and pathological humeral head translation overloads and damages the surrounding active tissues. Tendinopathy of the subscapularis and/or fluid around the long head of biceps tendon are common in PSI as chronic posterior translation of the humeral head compresses and stresses anterior/superior structures. The presence of glenoid retroversion and dysplasia should be assessed in all players with PSI, which may present for the first time when extra stresses of elite training are instituted. Computer Tomography (CT) scanning (with or without 3D reconstructions) is helpful in cases of underlying bony pathology,22 or those where the posterior instability has become macro-instability with bone wear posteriorly.
Management
There is a growing body of evidence that traumatic PSI with significant structural lesions have better outcomes with surgical stabilization.18,80 Patients with atraumatic PSI (commonly with no structural lesions) generally have good outcomes with rehabilitation.26 If patients with atraumatic PSI fail three to six months of good conservative management, surgery may be considered once basic scapula and humeral head motor patterning has been normalised. Patients with micro-traumatic instability (plus or minus a structural lesion) are more varied in their presentation and typically require three to six months of good conservative management. If this fails, surgery may be considered (refer back to Figure 1).77 Failure of conservative management refers to a player’s inability to return to play due to ongoing shoulder symptoms.109
Conservative management
The aim of conservative rehabilitation is to restore optimum scapular biomechanics, prevent pathological posterior humeral head translation and address any deficits in the kinetic chain. Restoring efficient scapular mechanics ensures maximal bony congruency65,66 and rotator cuff efficiency of the glenohumeral joint.68 Regaining motor control, then endurance, then strength of the rotator cuff and deltoid muscles assists in preventing excessive humeral head translation. Optimizing all segments of the kinetic chain reduces the forces required at the shoulder for the same power output.78,79,110
A systemic review26 of rehabilitation programs for PSI found overall favourable outcomes for pain, instability recurrence, functional scores (Rowe Score, Constant Score, Subjective Shoulder Rating System) and return to activity levels for programs that focused on re-establishing scapular control and a focus on posterior rotator cuff and deltoid, although included studies were not specific to overhead athletes. After the publication of that systematic review, Blacknall et al.,111 reported on 19 patients with atraumatic PSI using a retrospective case series. They found significant improvements in patient reported outcome measures (mean WOSI from 49.8% to 87% and mean Oxford Instability Shoulder Score from 22.7 to 40.9) and functional outcomes (able to return to study, sport and/or occupation) after a rehabilitation program that focused on motor control movement re-education, initially of simple movements then progressing to more functional movements. Many participants were involved in overhead sports, although only one in tennis. Specific exercise drills and parameters were not reported.
To date, there is only one published rehabilitation program specific for PSI with enough detail to replicate in the clinical setting.47 The Watson Instability Program for Posterior Shoulder Instability (WIP-p) is based on the Watson Instability Program (WIP1) for multidirectional instability (MDI). In a randomized controlled trial,102 the WIP1 has been shown to result in significant improvements in functional outcomes over a general rotator cuff and deltoid strengthening program in MDI patients, as well as significant improvements in strength, scapular upward rotation, and functional outcomes in single group study designs in MDI112 and high-level circus performers.100 In these studies, more than half of the participants had a component of posterior instability.100,102,112
The WIP-p focuses on regaining patient specific control of any observed scapular dysfunction (scapula phase) prior to the addition of rotator cuff and deltoid exercises (arc of motion phase) over five stages (Table 2). Scapular resistance (SR) bands are often looped around the scapula to provide resistance and enhance scapular stability with exercise drills.47,95,101 Exercises are progressed into functional and sports specific ranges as per the individual’s functional requirements. The program has a particular focus on posterior deltoid and rotator cuff function to control posterior humeral head translation and progresses exercises are eventually progressed into the sagittal (flexion) and horizontal adduction plane to gain control over previously vulnerable positions. Dosage for drills typically commence at a motor control dosage (1-2 sets x 20 repetitions, 2-3 times a day, light load) and progress to an endurance (2 sets x 15 repetitions, 1 x day, medium load) then strength (3 sets x 10-12 repetitions, 3 times a week, heavy load) then hypertrophy dosage if required (4 sets x 6-8 repetitions, 1-2 times a week, heavy load). In addition to addressing dysfunction at the shoulder, kinetic chain dysfunctions are assessed and normalized throughout the shoulder rehabilitation process.
The WIP-p has been evaluated in a single group study design in overhead athletes (n=24) with micro-traumatic PSI.113 Sporting categories of participants included four tennis players, two swimmers, four Australian football players, two cricketers, four netball players, and eight overhead weightlifters. Three participants had a structural lesion including a small tear of the posterior band of the inferior glenohumeral ligament and two posterior labral tears. After 24 weeks of the WIP-p (maximum 18 sessions) participants had significant improvements at 12 (effect size: 1.1, p<0.001) and 24-weeks (effect size: 1.8, p<0.001) on the Western Ontario Shoulder Index (WOSI) and significant improvements at six (effect size; 0.74, p=0.036), 12 (effect size: 0.41, p=0.007) and 24 weeks (effect size: 1.7, p<0.001) for the Melbourne Instability Shoulder Score (MISS). For return to sport, 22 of the 24 (91.6 %) participants returned to full activity at the 24-week time point. The remaining two participants were unable to return to their overhead sport and went on to have reconstructive surgery. One of these participants was a tennis player and the other was an overhead weightlifter, neither had a structural lesion.
Surgical Management
The threshold for surgical intervention is typically lower for overhead athletes, owing to the demands placed on the glenohumeral joint.11 Surgery aims to restore passive integrity of the joint by repairing structural lesions and/or excessive capsular laxity.114 This is primarily achieved through labral repairs and/or capsular plication. The outcomes of soft tissue stabilization for traumatic and micro-traumatic PSI are generally good with improved American Shoulder and Elbow Score (ASES) scores from baseline and return to sport rates of between 55 and 90%,18,20,53,115–118 though not all at their pre-injury level.18,117
Treatment selection is typically based on aetiology (i.e., surgery for traumatic PSI and failed conservative management for micro-traumatic or atraumatic PSI). Heterogenous patient populations (e.g., sporting with non-sporting, overhead sports with non-overhead sports, and traumatic with micro-traumatic populations), non-instability specific outcomes measures and a lack of control groups make synthesis of the true effect of surgery on PSI and return to sport challenging. To date, there is only one study that has investigated the effect of surgical stabilisation on 13 tennis players with PSI and posterior labral tears.119 Hoy et al,119 found that post arthroscopic posterior shoulder stabilisation, there were significant improvements in MISS and WOSI scores at 12 month follow up. Return to sport data were available for nine players with 89% returning to play and 56% at their previous level.
In patients with higher levels of glenoid retroversion (e.g. higher than 20 degrees) and/or glenoid dysplasia, an osteotomy may be considered in order to achieve a more congruent articulation at the glenohumeral joint, although there is no current evidence of its use in tennis players.120 Bone grafting procedures are not without risks and complications (e.g. failure of the graft, iatrogenic fractures, degenerative joint change)120 and should be considered only in cases where soft tissue reconstruction is likely to fail.
Return to Sport
Return to training and competition should be based on pain free shoulder function and reliable objective measures (refer back to Figure 1).121,122 Shoulder instability patients who pass an objective shoulder strength test (with assessment of isokinetic and isometric IR and ER strength and ER endurance) prior to returning to training and competition, may reduce their incidence of an instability recurrence by nearly five times compared to patients cleared to return to sport based on time from injury alone (5% vs. 22%; odds ratio, 4.85; p<.001)121 A “pass” was classified as having 90% strength and endurance of the unaffected side.121 Isokinetic machines are not always available clinically, however handheld dynamometry for evaluating shoulder strength over a range of positions has good inter- and intra-rater reliability when used by experienced practitioners (Intra-rater ICC; 0.84 -0.96. Inter-rater ICC: 0.82-0.96) .123 A detailed strength testing protocol for shoulder instability using a hand held dynamometer has been previously published123 and should include a range of shoulder positions, including those in the sagittal plane.123 Quantifying adequate glenohumeral range of motion for return to sport in PSI can be challenging as it depends on the intervention administered (surgery versus conservative), if the patient’s sport is unilateral or bilateral and pre-injury (or normal/adaptive) side to side TRROM differences. In the authors’ experience, achieving 90% TRROM post-surgery and 100% TRROM post conservative management of the unaffected side is required for commencing overhead competition in patients participating in non-unilateral sports (e.g., football, swimming). However, given the normal TRROM differences that may exist in unilateral, repetitive, overhead athletes (which may be up to 46 degrees44), comparing side to side differences may be unreliable. In such cases, it may be more appropriate to use normative dominant- arm TRROM values as a guide, which for adolescent tennis players has been shown to be 155.6 degrees in males and 160 degrees in females.124 Instability specific PROMs should reach at least 80% of the unaffected side prior to return to training.102
CONCLUSIONS
PSI in tennis players can be the result of repetitive microtrauma in combinations of shoulder flexion, horizontal adduction, and IR, which are characteristic shoulder positions for backhands, backhand volleys, and the follow-through phase of forehands and serves. Initial management of micro-traumatic PSI typically involves rehabilitation focusing on posterior rotator cuff and deltoid function and eventually progressing exercises into the sagittal and horizontal adduction plane. Due to the large demands placed on the shoulder in tennis, some individuals may require surgery if they fail appropriate evidence-based conservative management.
Conflict of Interest Statements
Lyn Watson, Simon Balster, Tania Pizzari and Sarah Warby were involved in the development and testing of the WIPp that is discussed in this paper. The Melbourne Shoulder Group pays consulting fees to Lyn Watson, Simon Balster and Sarah Warby. Lyn Watson and Simon Balster are directors of the Melbourne Shoulder Group. Sarah Warby provides research services on a contractual basis for Mr. Greg Hoy and the Melbourne Shoulder Group.