INTRODUCTION
Anterior cruciate ligament (ACL) injuries occur most commonly in the active young population, with individuals between 14 and 25 years having the highest injury risk.1 In patients who undergo surgical treatment after an ACL injury, up to 22% will go on to sustain a second ACL injury when attempting to return to sport (RTS).2
Returning to sport after an ACL reconstruction entails an increased exposure to the risk of sustaining a second ACL injury.3 Therefore, authors have aimed to assess whether patients can be defined as “ready” to RTS; i.e. achieving physical and psychological status that would be associated with reduced, or minimal, risk of sustaining a second ACL injury.4 Patients have reported that psychological impairments such as fear of re-injury are greater and more difficult to overcome than physical impairments such as pain or muscular weakness, both during rehabilitation and when returning to sport after ACL reconstruction.5 Despite clinical practice guidelines (CPG’s) highlighting the importance of assessing psychological factors during rehabilitation and RTS,6–8 time, strength, and hop tests are the most commonly used criteria to determine readiness to RTS. Psychological factors are important to integrate in RTS testing.9 Furthermore, systematic reviews assessing association between passing physical performance based RTS tests and second ACL injury risk show no associations.10,11 Psychological factors are important for patients, and clinical trials should aim to integrate psychological patient-reported outcomes (PROs) in RTS batteries and assess whether passing RTS assessments including both physical and psychological outcome measures is able to reduce the risk of a second ACL injury.
The aim of this study was to determine the association between passing clinical tests comprising both muscle function as well as psychological PROs, and second ACL injury in patients who RTS after primary ACL reconstruction.
METHODS
To enhance the quality and transparency of this study, the REporting of studies Conducted using Observational Routinely-collected Data (RECORD)12 statement, extended from the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)13 statement checklist for cohort studies, was followed. The present study was based on data extracted from a rehabilitation-specific outcome registry, Project ACL.14 The registry was established in 2014, with the aim of improving the care of patients after ACL injuries, regardless of treatment, surgical and rehabilitation or rehabilitation alone. The registry aims to improve care through utilization of standardized and continuous evaluation of rehabilitation specific outcomes in patients with ACL injury. The data in Project ACL consist of the results of unilateral isokinetic concentric strength tests, three unilateral hop tests (muscle function tests; MF) and responses to PROs (i.a. the ACL Return to Sport after Injury scale (ACL-RSI) and the Knee injury and Osteoarthritis Outcome Score (KOOS) from patients with ACL injuries. The data are collected prospectively, according to a standardized schedule of follow-ups, starting from ACL injury or ACL reconstruction (baseline), followed by assessments at 10 weeks, 4, 8, 12, 18 and 24 months, and then every five years. The tests are administered and supervised by physical therapists specifically trained and regularly updated in the test protocol. The test procedures have previously been described in detail.14,15 Prior to participation in Project ACL, patients receive written information and informed consent is obtained.16 Ethical approval was obtained from the Swedish Ethical Review Authority (registration number 2020-02501).
Study execution
Patients registered in Project ACL were eligible. Following inclusion criteria were applied: age between 16-50 years; pre-injury activity level of ≥ 6 on the Tegner Activity Scale (Tegner)17; suffered one ACL injury; treated with ACL reconstruction and participated in all the tests in the test battery. If no test data were available within six months of reaching Tegner ≥ 6, or if patients had not reached Tegner ≥ 6, i.e. returned to knee-strenuous sport, they were excluded. Patients who did not return to Tegner ≥ 6 are patients who might 1) clinically struggle to return to sport, which might be due to physical limitations, 2) change of interest and/or 3) change of life goals; 4) concomitant injuries; 5) a combination of the above.
In this specific study, returning to Tegner ≥ 6 was defined as RTS, since after Tegner level 6, only sport activities are possible choices, thereby excluding all patients who have knee demanding activities as an occupation. Patients who reported a return to knee-strenuous sport (Tegner ≥ 6) before the four-month follow-up after ACL reconstruction were excluded, since a return to knee-strenuous sport within four months of ACL reconstruction was deemed unlikely as the phase of graft healing starts around the fourth month,18 and strength deficits are high between three and six months after ACL reconstruction.19,20 Once included, data available from the follow-up closest in time to when patients reported at least Tegner 6 (RTS) were extracted for further analysis. A survival time of two years from reporting Tegner ≥ 6 after ACL reconstruction was used. Patients were followed for two years or to second ACL injury, whichever occurred first.
Data from MF tests, PROs and demographics for included patients were extracted from Project ACL in April 2021.
Muscle function tests
Before performing the MF tests, patients warmed up according to a standardized procedure consisting of 10 minutes on a stationary bike and sub-maximal trials on each test. The MF tests consisted of five tests: two isokinetic strength tests (knee extensors and knee flexors), and three hop tests. All tests were performed one limb at the time, starting with the reconstructed limb.
Torque (as a measure of strength) of the knee extensors and knee flexors was tested using an isokinetic dynamometer (Biodex System 4; Biodex Medical System, Shirley, NY, USA) at an angular speed of 90°/second. Strength testing with Biodex has been reported to be reliable (ICC = 0.95) when measuring muscle strength.21,22 Patients performed the strength test as previously described,14 sitting on the dynamometer chair, starting with knee extension. After the warm-up, patients performed three maximal trials, with 40 seconds’ rest between each trial. The rest period of 40 seconds was allowed to ensure patients were able to push as hard as possible, since the peak torque was the objective of the test. The highest values in Newton meters (Nm) were recorded.
The three unilateral hop tests were performed in the following order: the vertical hop, the hop for distance, and the 30-second side-hop test. For the vertical hop and the hop for distance, two trial repetitions were allowed before maximal testing. All the hop tests were performed with the patients holding their hands behind their back. For the vertical hop, the time from take-off to landing was converted into hop height in centimeters (cm) (Muscle lab, Ergotest Technology, Oslo, Norway). Three maximal trials were performed and the highest hop in cm was recorded. In the hop for distance, the distance in cm from toe at take-off to heel at landing was measured. Patients were required to perform a stable landing, without losing their balance or letting go of their hands. Three maximal trials were performed and the longest hop in cm was recorded. For the 30 seconds side-hop test, patients were required to perform as many hops as possible over two lines 40 cm apart. One 30-second trial was allowed, and the total number of hops (not touching the lines) was recorded. The hop tests were performed as described by Gustavsson et al,23 and were chosen as hop tests with the highest ability to discriminate hop performance in patients who had sustained an ACL injury and in patients who had undergone an ACL reconstruction. The hop tests have been reported to have a high level of sensitivity and accuracy in patients with an ACL injury (87% and 84%, respectively) and in patients who had undergone ACL reconstruction (91% and 88%, respectively).23
Patient-reported outcomes
The PROs used for analysis in this study were the ACL-RSI as well as only the Quality of Life (KOOS QoL) subscale of the KOOS, i.e. no other subscales than the QoL were used from the KOOS. The ACL-RSI was chosen, as it has been reported as a PRO with high methodological quality for evaluating patients with an ACL injury.24 The ACL-RSI measures the patients’ emotion, confidence and risk appraisal of RTS. The ACL-RSI has 12 items. Each item is graded from 0 to 10, where 10 is the highest response, representing the strongest positive emotion, confidence and low risk appraisal regarding RTS.25 The results for each item are summarized in a total score, normalized on a 0-100 scale. The KOOS QoL was chosen, as knee-related quality of life is an important part of recovery and can be impaired up to 20 years after an ACL reconstruction.26 The KOOS has five subscales: pain, symptoms, function of daily living, function in sports and recreation and QoL, and in this study only the QoL subscale was used. Each item is rated from 0 to 4 on a 5-point Likert scale. A normalized score from 0 to 100 is calculated for each subscale, where 0 indicates the most severe symptoms and 100 indicates no symptoms.
Four different test batteries to assess whether patients are ready to RTS were created for analysis. The same test batteries were previously introduced in a publication from our study group (Table 1).27
For the two MF test, the vertical hop and the hop for distance were chosen as Abrams et al.28 reported that these tests were the most commonly used after ACL reconstruction. The five MF tests were chosen according to current consensus criteria.29 Psychological PROs were added to both the two MF and the five MF tests, creating two additional different test batteries.
To interpret the results of all of the MF tests, a cut-off value of ≥ 90% limb symmetry index (LSI) was chosen to define whether or not a patient passed a test.30,31 The Limb Symmetry Index is the ratio between the injured and uninjured limb expressed as a percentage. For the ACL-RSI, a score of 76.6 points was used as a cut-off or passing score, since this score has been reported to have maximal sensitivity for discriminating between patients who suffer a second ACL injury and patients who do not.32 For the KOOS QoL, a score of 62.5 points was chosen as a passing score, since Mueller et al.33 suggested that this score represents a threshold of “feeling well” after primary ACL reconstruction.
Statistics
Patients demographics were presented stratified by patient sex, but no statistical comparison between sexes was performed. To pass (yes/no), each of the test batteries was used as an independent variable for analysis. A multivariable Cox proportional hazard model analysis was performed, with suffering a second ACL injury (yes/no) as the dependent variable. Sub-analyses were performed depending on whether the second ACL injury was ipsilateral or contralateral. A hazard ratio with a value greater than 1 indicates a variable that is positively associated with a second ACL injury, while a hazard ratio lower than 1 indicates a variable negatively associated with a second ACL injury.34 The results of the Cox proportional hazard model were reported with hazard ratios (HR), 95% confidence intervals (CI) and p-values. Statistical analyses were performed with the Statistical Analysis System (SAS) software 9.4 version (Copyright © 2013, SAS Institute Inc., Cary, NC, USA). Mean values with standard deviations (SD) or medians (min-max) were presented for demographic data for the entire cohort and stratified by sex. A significance level of 0.05 was set.
Several factors have been previously associated with second ACL injury risk: they include young age (13-19 years), female sex, high BMI (≥ 25), time to return to knee-demanding physical activity (≥ 9 months) and several surgically related factors, i.e. graft choice and fixation.16,35,36 To account for variables associated with a second ACL injury risk, demographic variables were compared with the outcome of interest, i.e. suffering a second ACL injury (yes/no), using Fisher’s exact test. Consequently, model analysis was adjusted for variables significantly associated to the risk for a second ACL injury, that is: time to RTS (months) and patient sex.
RESULTS
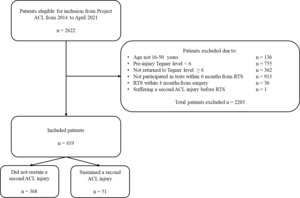
A total of 419 patients were included in the study (men, n=214; 51%). A flowchart of the inclusion process is presented in Figure 1 and demographics for the included patients are summarized in Table 2.
A total of 51 (12.2%) patients suffered a second ACL injury within the first two years after RTS, of which 31 (61% of second ACL injury) occurred ipsilaterally and 20 (39% of second ACL injury) occurred contralaterally (Table 2).
The number of second ACL injuries per month following primary reconstruction and the side of the second ACL injury are presented in Figure 2. The number of second ACL injuries per month following RTS (Tegner ≥ 6) and the side of the second ACL injury are presented in Figure 3.
The proportion of patients that passed the different test batteries, stratified by whether or not patients suffered a second ACL injury, is presented in Figure 4. There were no differences in passing rates for the respective test batteries between patients who suffered a second ACL injury and patients who did not. As such, the test batteries were not able to identify patients who were at increased risk of sustaining a second ACL injury. Results for the univariable and adjusted Cox proportional hazard model are presented in Table 3.
When stratifying patients depending on whether the second ACL injury occured ipsilaterally or contralaterally, passing any of the test batteries was not able to identify patients who were at an increased risk of sustaining a second ACL injury (Table 4 and 5).
The Cox hazard ratios associated with a contralateral second ACL injury was only performed in a univariate manner (not adjusted) since no confounding variable showed a significant difference between groups and was therefore not deemed to be a confounding variable.
DISCUSSION
The main finding in this study was that passing various clinical test batteries consisting of muscle function and psychological PROs had no association with the risk of sustaining a second ACL injury in patients who had undergone primary ACL reconstruction.
The addition of psychological outcomes to the RTS test batteries in the present study was not able to identify patients running an increased risk of suffering a second ACL injury. However, the authors’ still assert that the inclusion of psychological outcome measures in the assessment of individual patients prior to RTS is meaningful, as patients express that psychological factors are of great importance,5 and second ACL injury risk is likely a complex puzzle incorporating physical and psychological dimensions.37,38 Results of interview studies suggest that some patients may not feel ready to resume sports participation and are afraid to RTS due to the risk of sustaining a new knee injury.39–41 RTS assessments seldom include the assessment of fear and readiness and, as a result, they may not measure factors that predispose patients to second knee injuries.42,43 Although psychological outcomes in terms of emotions, confidence and risk appraisal of RTS, as well as knee-related quality of life were assessed in the current study, there might be other psychological outcomes, such as fear or readiness to RTS, which might be better when it comes to understanding second ACL injury risk. Further, clinicians aiming to assess whether patients can RTS with the lowest second injury risk, cannot rely on a single type of measurement (performance or strength), as second injury risk depends on many different factors. Consequently, therapists need to improve understanding of the many available PROs and cut-offs that are most relevant in order to identify patients who may be at greater risk of second ACL injuries. For instance, the KOOS QoL subscale might not be an appropriate tool for second ACL injury risk reduction, and the cut-off of 62.5 was calculated by anchoring QoL to a specific question considering patients 'satisfaction with current knee status. The ACL-RSI was developed to measure patient emotions, confidence and risk appraisal regarding and confidence in RTS,25 which are three different constructs. Psychometrically, concerns have been raised as to whether the outcome of three different constructs can be added up to produce one score or whether it should be presented as two different scores, as principal component analysis has shown at least two underlying factors.44,45 However, the ACL-RSI was the only scale in the test batteries that proved able to discriminate between patients who suffer a second ACL injury and patients who do not in previous studies.32,46
The results of the clinical tests used in the current study were not associated with a second ACL injury, which confirms results summarized in two systematic reviews that investigated associations between passing RTS test batteries and occurrence of second knee injuries after an ACL reconstruction.10,11 The current results indicate that four different test batteries were unable to identify patients at increased risk of sustaining second knee injuries after ACL reconstruction.10,11 Future research should examine the test batteries and assess each component of the battery (e.g. hop test or PRO) to identify patients running the risk of new ACL injuries after ACL reconstruction. With regard to passing MF tests, a cut-off of an LSI of ≥ 90% was used to define “pass”, based on consensus criteria published in 2015.30 Notably, the consensus criteria stating that 90% LSI is “successful outcome” after ACL reconstruction, does not clearly define what “successful” infers. Arguably, an LSI of ≥ 90% has been used as a proxy for muscular recovery,47–49 and consequently, as a logical step towards assessing patients for RTS. However, the sensitivity or specificity of the cut-off in relation to the risk of a second ACL injury has perhaps not been accounted for. Taken together, further studies determining cut-off values for all included tests of MF and their relationship to a second ACL injury after a primary ACL reconstruction are warranted, and clinicians working with patients who have undergone ACL reconstruction should look beyond results from test batteries and consider second ACL injury risk as a multifactorial construct not only displayed in clinical tests results, where factors such as female sex,50 younger age,3 concomitant injuries and surgical outcomes interplay.51,52
Limitations
There are some limitations to this study. The exact rehabilitation that was administered and the extent of rehabilitation compliance are not known. Patients compliant with rehabilitation that consists of high-intensity training might be more prone to attempt RTS earlier and possibly have higher scores on PROs as well. Another limitation is that concomitant injuries such as cartilage, multi-ligamentous, or meniscal injuries, were not accounted for, which could potentially further increase the risk of a second ACL injury.53 Several statistical analyses were made in this study, raising the risk of type 1 error. However, the possibility of type 1 errors was accounted for by providing CIs for all hazard ratios as a measurement of uncertainty, attempting to move away from the assumption that significant p-values mean “true” or clinically significant results.54 Another limitation is that data were analyzed for the available follow-up closest in time to when patients reported having returned to a Tegner ≥ 6. Project ACL’s follow-ups are 10 weeks and 4, 8, 12, 18 and 24 months after baseline. The results for a patient who has returned to Tegner level ≥ 6 at 10 months after ACL reconstruction might therefore have been taken from the 8-month follow-up. However, muscle strength, knee function and psychological readiness can develop and change over a period of two months and the actual patient status at the time of RTS might therefore have been different compared with the time of RTS testing. This limitation was partially accounted for by excluding patients who did not participate in a follow-up within six months of reaching Tegner ≥ 6. The use of Tegner as a measure of functional status is a limitation in this study, as the Tegner assesses the level of knee-strenuous activity, but it does not account for the time of exposure or the intensity of exposure for a patient, which are factors that contribute to the risk of a second ACL injury.55 A further limitation is the exclusion of patients who did not return to Tegner ≥ 6 in the analysis. Patients who do not return to Tegner ≥ 6 might have presented with physical problems which obstructed their possibility of performing physical tasks and would have prevented their RTS. Therefore, it is important for clinicians to consider that results from the current study might not be applicable to patients who do not return to Tegner ≥ 6. A further limitation concerns the exclusion of patients who reported RTS before the four month follow-up. The use of LSI to assess muscle strength is a limitation itself as it does not account for movement quality, nor for eventual strength losses in the uninvolved leg, compared with pre-operative values.56 Additionally, a further limitation might concern treating RTS as a dichotomous variable. The RTS involves a criteria-based progression starting from return to participation to RTS and, ultimately, return to performance, and can be described as a continuum that starts the day of injury.57 Taken together, these limitations affect the general external validity of results in the present study. However, it is important that clinicians not rely solely on the results of test batteries to assess the risk of second ACL injury in the process of sharing information (regarding test results and second ACL injury risk) with patients who are about to resume RTS after ACL reconstruction. Future prospective studies with large cohorts and different test batteries, with different cut-offs are warranted in order to develop greater knowledge of passing clinical test batteries including physical and psychological outcomes and their ability to reduce the risk of a second ACL injury.
Conclusion
No associations between passing any of four clinical tests batteries that included assessments of muscle function and psychological PROs and the risk of a second ACL injury were found in patients who had undergone primary ACL reconstruction.
Grant support
Local Research and Development Board for Gothenburg and Södra Bohuslän: grant number 937140. The funding source had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Conflict of interest
Author KS reports he is a Member of the Board of Directors of Getinge AB (publ).
Acknowledgement
The authors thank biostatisticians Bengt Bengtsson and Nils-Gunnar Pehrsson from Statistiska Konsultgruppen for help with the statistical analyses and advice on the interpretation of data.

_as_baseline.jpg)



_as_baseline.jpg)
