INTRODUCTION
The posterior cruciate ligament (PCL) resists excessive posterior tibial translation and excessive rotation of the knee at different knee flexion angles.1 PCL injuries are uncommon with an estimated annual incidence of 2 per 100,000.2,3 These injuries normally occur due to high-speed traffic and sports-related accidents,4–6 and the prevalence is highest among young men.5,7–9 The major deficits associated with PCL injury is abnormal tibiofemoral kinematics10,11 and early knee osteoarthritis.11,12 These deficits are experienced as discomfort and knee instability.13 Historically, PCL injuries have been treated surgically14 but in recent years, it has been accepted that the PCL has a natural ability to heal7,8,14 and non-operative interventions have become first-line treatments.7 Several studies have reported clinically relevant patient-reported improvements after non-operative interventions.5,8,9,12,14,15 However, results of previous studies have reported insufficient PCL stability following both non-operative interventions and surgical reconstructions.7,8 In addition, prevalence of knee osteoarthritis after PCL reconstruction has been reported to be similar or worse compared to non-operative interventions.6,16–20
Non-operative treatments normally cover supervised exercise and support brace interventions focusing on the most optimal healing of the PCL and regaining range of motion (ROM) and strength with an emphasis on quadriceps activation.1,14,21 Several authors have reported normalized knee strength following non-operative interventions.5,6,15 as well as clinically relevant long-term improvements in patient-reported outcomes.12,22 However, the majority of these studies fail to report the specific rehabilitation regimens and the support brace interventions.5,7,9,16,19,23 Therefore, the primary aim was to investigate changes in patient-reported outcomes of a physiotherapy-led exercise and support brace intervention in patients with acute injury of the PCL over a two-year follow-up period. Furthermore, secondary aims were to investigate changes in isometric knee muscle strength over an eight-month follow-up period, and finally to report conversion to surgical reconstruction over a two-year follow-up period.
MATERIAL AND METHODS
Study Design
This study was performed in accordance with the Code of Ethics of the World Medical Association and the Danish Code of Conduct for Research Integrity. All patients gave informed consent to participate. This study was notified to the Central Jutland Region Committee on Health Research Ethics (Case no. 1-10-72-1-19). The Danish Data Protection Agency permitted handling of personal data (1-16-02-549-13). Patients who declined to participate received similar treatment except for prospective registrations.
Participants
From June 2015 to January 2018, patients with a PCL injury were consecutively recruited from the Department of Orthopaedic Surgery at Aarhus University Hospital, Denmark. The inclusion criteria were an acute injury to the PCL, isolated or in combination with other knee ligament injuries presenting within eight weeks after injury. Exclusion criteria were fibular head fractures, avulsion fractures of the PCL, inability to comprehend, read, or speak Danish.
Scheduled assessments took place at 12- and 16-week follow-up visits and was a part of the routine treatment, while one- and two-year follow-up was scheduled explicitly for the study. Sport traumatology orthopaedic surgeons diagnosed all patients by magnetic resonance imaging in combination with a thorough physical examination.
Physiotherapy-led Exercise Intervention
Over a period of 16 weeks, the included patients were offered seven physiotherapy-led training sessions: one time every two weeks. All sessions lasted 60 minutes and were conducted in the hospital with one-to-one supervision by physiotherapists with more than 15 years clinical experience in training of musculoskeletal disorders. At the first visit a support brace was fitted to the patients, the physiotherapists counselled the patients on how to wear the brace and the patients were instructed in exercises to do at home (Additional File 1). Exercise equipment (handheld dumbbells and a balance mat) was loaned to the patients to increase load and progress stability exercises. All exercises were based on recommendations from previously described exercise interventions24,25 and were individually selected and tailored to each patient.
Weight bearing was allowed from the start of the treatment with or without ambulating. In the first four weeks of the exercise intervention, it was important to respect tissue healing, joint response and individual adaptions, and to produce a minimum stimulus in this post injury recovery period to preserve muscle mass, but not overload the joint. Therefore, patients were recommended to perform one set of 12 repetitions three times a day and the starting level of the exercises (e.g., use of hand support, dumbbells or Thera-band elastic bands) was adapted to each patient’s pain level and ability to perform each exercise.
Exercises focused on effusion control, ROM, proprioception, muscle activation of the knee extensors and muscle strength exercises for the knee extensors, hip abductors and calf muscles. At week three a cross-trainer and a stationary exercise bike was recommended for warm up. Progressive Strength Exercises (PSE) were introduced gradually from week five with a starting load of three sets of 12 Repetition Maximum (RM). A 12 RM was chosen because it is considered a moderate load and has been recommended for hypertrophy training by the American College of Sports Medicine in patients who are novice to intermediate in resistance training.26 Patients were recommended to perform the PSE three times per week with a minimum of one restitution day between the sessions. The PSE training modality is documented in Additional File 1, using the strength training descriptors suggested by Toigo and Boutellier.26 PSE included leg extension (ROM 90-0°), heel raise, squat (ROM 0-90°), deadlift, modified leg press and hip abduction. The absolute training load (handheld dumbbells lifted or resistance applied with Thera-band elastic bands) was adjusted on a set-by-set basis for all muscular strength exercises. Patients with moderate swelling and acceptable pain (Numeric Rating Scale [NRS] < five) and who were motivated, were allowed to go to a fitness center from week four. This was to ensure that patients did not underload with the homebased exercises. They were given instructions from the physiotherapists on which exercises to do, and the exercises resembled the exercises from the PSE protocol e.g., leg extension with elastic bands was done in the leg extension machine and hip abduction was done in the pulley tower.
Criteria for load increase in each specific exercise was that patients could perform 1-2 extra repetitions over the desired number.27 This was a simple way for the patients to determine load on their own, making sure that load was progressed when indicated and not only at physiotherapy sessions.
In terms of regression and progression, three principles were applied28 (1) The patients could perform the exercises correctly (i.e. adequate hip, knee and foot alignment); (2) the patients could perform 12 repetitions; (3) patients experienced no knee joint pain above five out of 10 on a NRS for pain anchored by “no pain” (score of 0) and “unbearable pain” (score of 10) during and after the training session.29 The criteria were implemented to ensure that the applied training stimulus was not excessive and causing tissue overload. Patients were also told that the day after training, pain should subside to “pain as usual.” If the pain did not subside, the level of training was reduced.29 The NRS for pain was chosen because it is a well-known scale and easy to administer for patients when rating pain. At the end of the 16-week period, the patients were encouraged to continue exercising at home or at a fitness centre and gradually return to usual activities. The patients aiming to return to knee-strenuous sport were advised not to return before they had recovered full range of knee motion and achieved a Leg Symmetry Index (LSI) of ≥ 90 % in knee extensor strength.2 At the end of the 16 weeks exercise intervention, these patients were recommended to seek supervision from a physiotherapist and complete an intense sport-specific rehabilitation programme including evaluation of return to sport readiness.
Support Brace Intervention
In addition to exercises, the patients wore one of two support braces for the first 12 weeks, either the PCL-Jack brace (Albrecht GmbH, Stephanskirchen, Germany) or the Rebound PCL brace (Össur Inc., Foothill Ranch, CA, USA). Both braces provided an anteriorly directed force to the posterior proximal tibia. Throughout the 12-week period, physiotherapists (BB, RGR) with in-depth knowledge of adapting and adjusting the brace performed individual brace sizing and fitting with the ROM set to 0-90° and the force loading as high as tolerable. In cases with injury of both cruciate ligaments, the load on the brace was reduced to avoid possible anterior subluxation of the knee.
Outcome Measures
Patient-reported outcomes were recorded at baseline (immediately after the diagnosis was confirmed), at one-year and at two-year follow-up. Isometric knee strength was assessed after 16 weeks and at one-year follow-up. Posterior translation of the tibia was measured by stress radiography at one-year follow-up, and by KT-1000 arthrometry and a posterior drawer test at three-month and one-year follow-up.
Primary Outcome
The primary outcome was measured by the International Knee Documentation Committee Subjective Knee Form (IKDC-SKF).30,31 The IKDC-SKF is designed to measure symptoms and function in patients undergoing knee surgery or non-operative interventions.30,31 The Danish translation of the IKDC-SKF has demonstrated excellent test-retest reliability at group and individual level and adequate responsiveness with an intra class correlation of 0.94. Standard error of measurement of 2.6 points and a minimal clinically important change of 7.0 points.32
The IKDC-SKF consists of 10 questions, which can be converted to a total score ranging from 0 to 100 points, where 100 points indicate the best possible outcome.
Secondary Outcomes
Secondary outcomes were isometric knee extensor and flexor strength and conversion to surgery. Strength tests were performed with a static strength dynamometer (Echo™ Wireless Static Force Gauge, JTECH Medical, Utah, USA), assessing pull force, using a standardized test protocol.33 (Figure 1A and 1B).
The highest level of strength testing includes isokinetic devices, but dynamometry provides a clinically applicable and less costly alternative for isokinetic testing. Isometric strength testing of knee extensor and flexor strength using dynamometry offer sufficient intrarater reliability when consecutive contractions within one session are performed in a standardized seated position.34,35 Tests were carried out by a physiotherapist (RGR) trained and experienced in measuring knee strength with the static strength dynamometer and tests were performed as a make test. The make test assesses the patient’s full maximum voluntary isometric contraction possible. However, in this study pull force was assessed using a load cell. This type of dynamometers has shown to be reliable with an ICC of 0.953, and MDC of 11.4 kilogram-force. The patient was seated with 90° of knee flexion. An external strap was placed around the ankle five cm proximal to the prominence of the lateral malleolus, and the load cell was fixed between the strap and a wire attached perpendicular to the wall. Isometric knee extension was measured first followed by measurement of isometric knee flexion. For practice, patients were instructed to exert one submaximal contraction into the strap. After practice, the patients exerted four maximum voluntary contractions against the strap with a break of 30 seconds between each contraction. The patients were instructed to push as hard as possible for five seconds against the strap. If the fourth contraction was higher than the previous, additional trials were performed, until no higher measurements were recorded. The best result of each test (knee extension and flexion) was recorded. The moment arm was calculated by measuring the distance from the knee joint lateral space to five cm proximal from the prominence of the lateral malleolar tip - the site of the external strap fixation including the load cell.
Strength values were normalized to moment arms and weight and reported as Nm/kg bodyweight. Finally, the limb symmetry index (LSI) was calculated as knee extensor and flexor strength performance of the involved limb/knee extensor and flexor strength of the uninvolved limb x 100%
The physiotherapist (RGR, BB) extracted information about conversion to surgery from the patients’ medical records.
Other Outcomes
Other outcomes included the Knee injury and Osteoarthritis Outcome Score (KOOS), PCL stress radiography, objective PCL laxity measured by KT-1000 arthrometry (instrumented drawer testing) and tibial offset using the posterior drawer test. The same radiographer specialized in the kneeling technique for posterior cruciate ligament stress radiography did all the PCL stress examinations. The KT-1000 and tibial offset examinations were performed by an experienced and trained physiotherapist (LM).
The KOOS is a valid, reliable and responsive outcome measure designed to measure symptoms, function and quality of life in patients with knee injuries and knee conditions following operative and non-operative interventions.36 The KOOS includes 42 questions divided into five separate subscales: Pain, symptoms, function of daily living, function in sport and recreation, and knee-related quality of life. Each sub score can be converted to a total score ranging from 0 to 100 points, where 100 points indicate the best possible outcome. The KOOS has a high test-retest reliability with an ICC across subscales ranging from 0.61- 0.95 and the MDC across subscales ranges from 5-12 points.37
Objective quantification of knee laxity was done by PCL stress radiography with the kneeling view technique38,39 measuring total posterior displacement (Additional File 2). PCL stress radiography using the kneeling stress method provides a reproducible method to quantify posterior laxity in patients with PCL lesions with intra- and interobserver reliability ICC of 0.973 and 0.955 respectively.40,41 The degree of tibial displacement in millimeters for the injured and the non-injured knee was measured, and the mean side-to-side difference (SSD) was calculated.
The posterior tibial translation of the knee was additionally measured with the KT-1000 arthrometer (MEDmetric, San Diego, CA) using the method described by Daniel et al.42 The KT-1000 arthrometer has been shown to have an intra- and intertester reliability of 0.79 and 0.62 respectively and a SEM of ±2.53 in patients with a PCL injury.43 Two tests on each leg were performed; the first test at 30° of flexion and the second test at 70° of flexion. KT-1000 arthrometry was done with a 30 lb force, equivalent to 135 Newton. The mean SSD of the second test was calculated and used in the analysis.
Evaluation of tibial offset using the posterior drawer test39 was classified by the tibial grading system; In grade A injuries, the plateau remains anterior to the medial femoral condyle. In grade B injuries, the plateau is flush with the medial femoral condyle and in grade C injuries the plateau is displaced posteriorly to the medial femoral condyle. Evaluation of tibial off set using the posterior drawer test provides a 96% accuracy for detecting a posterior cruciate ligament tear, with a 90% sensitivity and a 99% specificity.44 Patient characteristics were recorded at baseline, including age, gender, height, weight, dominant leg (i.e., preferred leg to kick a ball), mechanisms of injury, date of injury and previous knee injuries.
Statistical Analysis
Continuous data were reported as means with standard deviations (SD) if normally distributed, otherwise reported as medians with interquartile ranges. Histograms and Q-Q plots were used to test for normality. Categorical data were reported as numbers and percentages. Changes from diagnosis to follow-up after 12 weeks, 16 weeks, one and two years were analyzed with a mixed effects model with patients as a random factor and time as a fixed factor. Model assumptions were based on inspection of plots of standardized residuals versus fitted values and Q-Q plots of the standardized residuals. The STATA 14.2 (StataCorp, College Station, TX, USA) software package was used for data analysis, and results were considered statistically significant if p < 0.05.
All data were reported as one group only (covering both isolated and combined PCL injuries) as the study population was considered representative for the isolated and combined PCL injury distribution at Aarhus University Hospital. However, outcomes divided into isolated PCL injury and multi-ligament injury were additionally calculated applying the same mixed effects model as aforementioned.
Sample Size Considerations
The aim of this study was to investigate changes in the IKDC-SKF over a two-year follow-up period and changes in isometric knee muscle strength during eight-month follow-up. Annually, approximately 20 patients are treated non-surgically at Aarhus University Hospital. Based on a clinical and research judgment, a convenience sample size of 45 patients was considered appropriate to represent the target population and large enough to provide data on changes from before to two years after treatment. To consider dropout, this study aimed to recruit 50 patients.
RESULTS
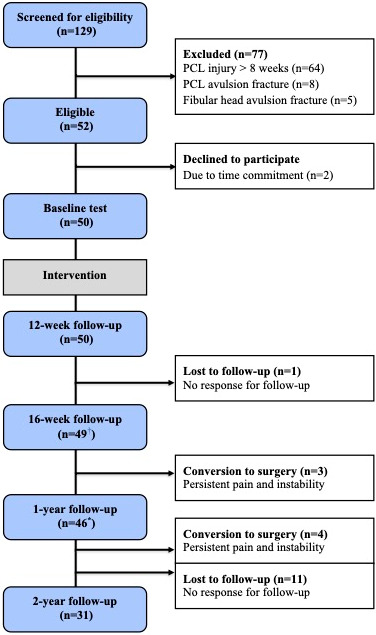
In the study period, 50 patients were included out of 52 eligible patients (Figure 2).
In total, four patients (one isolated PCL injury) were lost for the one-year follow-up (baseline characteristics; three males, median age 38 (range 20-41), median BMI 29 (range 21-31), mean IKDC 36 (range 22-53) and a total of 15 patients (11 isolated PCL injuries) were lost for the two-year follow-up (baseline characteristics; 14 males, median age 33 (range 17-47), median BMI 28 (range 19-37), mean IKDC 36 (range 22-53). The characteristics of the included patients are reported in Table 1.
Results divided into groups of isolated PCL injury and multi-ligament injury are available in the Additional File 3.
Primary Outcome
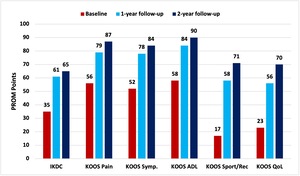
The IKDC score increased statistically significantly from 35 IKDC points at baseline to 65 IKDC points two years after injury (p <0.001) (Table 2 and Figure 3).
Secondary Outcomes
Isometric knee strength
There was no change in isometric knee extension strength. In contrast, isometric knee flexion strength of the injured knee increased from 0.93 Nm/kg at 16 weeks to 1.1 Nm/kg after one year, corresponding to an increase of 16% (p < 0.001) (Table 3).
KOOS Scores
All KOOS subscores increased statistically significantly, with the highest increase in the subscore function in sport and recreation.
Knee Stability Measures
PCL stress radiography showed a mean of 6 mm tibial displacement in the injured knee whereas the healthy knee showed a mean of 10 mm tibial displacement at one-year follow-up. The mean SSD was 4 mm at one-year follow-up. For the KT-1000 arthrometer assessment, baseline posterior laxity in the injured knee was unchanged from baseline 9 mm (SD 3.3) to one-year follow-up 9 mm (SD 3.3) p=0.804, whereas the healthy knee was 6 mm (SD 2.7) at baseline and 5 mm (SD 2.5) at one-year follow-up and the overall mean SSD was 5 mm (range 0-14). Tibial offset was measured in 39 patients: Five patients improved from grade B to grade A, one patient improved from grade C to B, one patient improved from grade A to grade 0, and no changes were observed in 24 patients (62%). Finally, eight patients worsened from grade A to grade B or C.
Conversion to Surgery
During the study period, seven patients converted to PCL surgical reconstruction. Out of these patients, two patients had an isolated PCL injury and five patients had knee dislocation injuries. Injuries at baseline and conversion to surgery are reported in Table 4. Median time from initiation of non-operative intervention to surgery was 13 months (range 10-14).
DISCUSSION
The primary findings of the present study were that patients with acute isolated and multi-ligament PCL injuries treated with the physiotherapy-led exercise and support brace intervention reported clinically relevant improvements from baseline to two-year follow-up, isometric knee flexion strength improved clinically relevant from 16 weeks after injury to one-year follow-up and only 15% of patients needed conversion to surgical reconstruction.
Several previous studies have reported patient-reported outcome after non-operative intervention for PCL injury. However, no studies have investigated changes from injury to one- and two-year follow-up. Compared to previous studies on non-operative treatment, the scores of this study are relatively low. Two studies by Shelbourne et al.8,15 reported IKDC-SKF scores of 83 points in 85 patients at nine-year follow-up and 73 points in 68 patients at 18-year follow-up in patients with an isolated PCL injury. Patel et al6 reported an IKDC-SKF score of 84 points in 57 patients with an isolated PCL injury seven years after injury. Jacobi et al.7 reported an IKDC-SKF score of 95 points two years after injury in 17 patients with an isolated PCL injury. The lower patient-reported outcome score in the present study can probably be explained by a shorter follow-up and since this study included 22 patients with multi-ligament injuries, who were more severely injured compared to the patients in the previous studies with isolated PCL injuries.6,8,15 as shown in Additional File 3. Based on one study by Shelbourne et al.15 reporting subjective improvement in 23% of patients after two years, the authors expect the patients with an isolated PCL injury to improve to a level similar to the follow-up score reported in the previous studies.7,8,15,23 (also indicated in Additional File 3). In the Additional File 3, the authors report baseline patient characteristics and results divided into two groups e.g., isolated and multi-ligament injury. These data indicate that patients with multi-ligament injury report lower baseline scores compared to the patients with isolated injuries. Nonetheless, at one-and two-years follow-up the scores of the two groups seem to be similar. However, no formal statistical tests for group differences were done.
Knee extensor strength is associated with patient-reported outcomes following a PCL injury.45,46 In this study, knee extensor strength in the injured knee did not change from 16 weeks to one-year follow-up, but the isometric knee flexor strength improved by 16%. Previous studies on knee extensor strength following non-operative intervention showed that the majority of patients treated non-operatively regained almost normal knee extensor strength after isolated PCL injury.5,12,15,23 One study by Shelbourne et al.5 reported an LSI of 97% in mean knee extensor strength and 93% in mean knee flexor strength in 44 patients 14 years after (isolated) PCL injury. In another study by Mygind-Klavsen et al.,47 only minor differences in knee extensor strength between 77 patients with isolated PCL injuries compared with 119 patients with combined PCL injuries were reported six years after PCL reconstruction, and both groups were classified as normal or nearly normal. Follow-up strength outcomes were slightly lower in the present study compared to the previous studies, and this can be explained due to several factors. First, this study included patients with isolated PCL and multi-ligament injuries, typically experiencing more residual knee instability and symptoms negatively affecting rehabilitation. Second, as opposed to the study by Shelbourne et al.5 only a few of the patients in the present study were semi-professional athletes, possibly impacting negatively on rehabilitation conditions due to lower motivation and physical functioning. Third, the start of progressive strength exercises was delayed as the mean time from injury to start of treatment was 23 days. Fourth, different muscle strength tests were used making comparison difficult. Fifth, in the present study knee strength was measured 13 years earlier than reported in the previous studies. Finally, all patients underwent prospective scheduled follow-ups. On the contrary, the previous studies were typically based on retrospective data, possibly negatively influencing risk of information and selection bias.
Currently, non-operative intervention is considered first-line treatment for patients with an isolated PCL injury followed by PCL reconstruction if needed.48 The results in the present study support this treatment strategy, showing little need for PCL reconstruction (9%) in case of isolated PCL injury. This is supported by a previous study,6 reporting that two out of 58 patients required PCL reconstruction after non-operative intervention in patients with an isolated PCL injury. In recent years, non-operative interventions have played an increasing role with the use of support braces to ensure optimal healing of the PCL. In this study, both progressive exercises and a support brace were applied. However, the residual PCL laxity may indicate that the brace treatment failed to ensure sufficient anatomical PCL healing to a degree where the PCL is fully stable. Nevertheless, no previous clinical studies have described the non-operative intervention as thoroughly as in this study.
The authors acknowledge that there are several limitations to the present study. First, the sample size was based on a convenience sample, and therefore lack of statistically significant changes because of to low power may exist. Moreover, the authors expected a dropout of five out of 50 patients. However, at the two-year follow-up, only 31 patients completed the outcomes, and therefore, the risk of too low power is even higher for this time point. In general, PCL injuries are relatively rare resulting in a low sample size in most studies on the management and outcomes of PCL injuries. Nevertheless, the authors still believe that this study adds valuable knowledge about non-operative treatment intervention of this patient group. The patients lost to follow-up were comparable to patients who completed follow-ups regarding baseline characteristics and thus, the loss to follow-up could result in either under- or overestimation of the results. Second, knee muscle strength and PCL laxity were not measured at baseline for ethical reasons (risk of injuring a healing ligament). Third, the study population was heterogeneous covering patients with both isolated PCL injuries and multi-ligament injuries. However, dividing patients into two groups, would also be problematic, because of the consequence of additional concerns for low power. The heterogeneous group causes a large variety of data, meaning that results may be underestimated if compared to patients with isolated PCL injuries whereas changes would be overestimated if results are compared to patients with multi-ligament injuries. This study consecutively included all patients who met the inclusion criteria and thus, the study population represents the distribution of isolated and multi-ligament PCL injuries at Aarhus University Hospital. Fourth, the physiotherapists who tested the patients clinically were not blinded, and therefore, the authors cannot rule out that lack of blinding may have an impact on the results. Fifth, the results were not compared to results of a control group and no training or health technologies were used to document rehabilitation adherence. Consequently, the authors do not know if the changes occurred due to time or if the changes were because of the intervention. However, offering no treatment to a control group would not be ethically acceptable. Sixth, a delay in treatment initiation of up to eight weeks in some patients may have resulted in worse outcomes. Nevertheless, delay in treatment initiation at our institution do occur, and therefore, the results in this study will describe what patients and clinicians should expect following treatment.
CONCLUSION
Patients with an acute PCL injury treated with the physiotherapy-led exercise and support brace intervention can expect clinically relevant improvements in patient-reported outcomes and knee flexion strength, and the risk of PCL reconstruction is considered low within the first two years. However, further studies are needed to establish the effect of different exercise and support brace interventions.
Conflict of interest/competing interests
The authors declare that they have no financial or non-financial interests to disclose.