INTRODUCTION
Assessment of joint range of motion (ROM) aids diagnostic and clinical decision-making for persons with a wide variety of neuromusculoskeletal conditions. The current clinical standard for assessing ROM is the standard goniometer (SG), that costs about $10. Visual estimation is often used in clinical practice as a quick and free alternative to SG. However, studies of visual estimation have shown lower intrarater and interrater reliability than assessment using a SG.1,2 Although methodological differences challenge direct comparisons among studies, interrater reliability using the SG varies among studies and is weak.1,3–8 Use of a SG requires lining up the goniometer arms with standard bony landmarks. While some landmarks are superficial and easily found, others, such as the greater trochanter, are more challenging, with as much as 15 mm difference in location recorded between raters,9 leading to significant goniometric measurement errors. Maintaining SG alignment can be challenging in certain populations, such as in children with cerebral palsy10 or in people with orthopedic conditions.3 Additionally, keeping alignment generally requires two hands to reduce the risk of error.11
The HALO® (HALO, HALO Medical Devices, Australia) is a hybrid between a goniometer and an inclinometer that utilizes a laser to intersect proximal and distal anatomical landmarks relative to the joint being measured. The HALO® device costs between $160 and $200.12 While the digitization of angular measurements removes one source of measurement error, the HALO® still requires proper alignment of the laser with proximal and distal landmarks. Intrarater and interrater reliability for the HALO® has been found to be similar or slightly less than the SG for shoulder rotation.13 Smart phone applications which utilize a magnetometer-based goniometer are also available for ROM assessment. Smart phone applications have greater intrarater and interrater reliability than the SG14 and they can be useful for patient self-assessment of ROM.15,16 However, smart phone applications have not been proven reliable across multiple joints or in all movements.17,18 They also require a dedicated clinic phone (or phones) to maintain proper infection control. The lack of consistent guidance regarding alignment may contribute to measurement error.13
Bubble inclinometers are handheld devices used to assess ROM in rehabilitation settings. Bubble inclinometers have a fluid-filled circular face. The fluid is a combination of a colored fluid and clear fluid. The interface of these two fluids moves with gravity, and this movement is used to measure motion against a rotating 360° dial. Bubble inclinometers are typically used to measure spinal motion. This measurement requires the placement of two devices at specific landmarks, zeroing each device, having the patient move through a ROM, and then reading the end measurements once the fluid has stopped shifting within the device. Bubble inclinometers, therefore, require increased time, and, in the case of spinal motion, require the use of two hands. Inaccurate assessment using the bubble inclinometer includes misplacement of the inclinometer on the body part, failure to maintain constant pressure of the inclinometer against the body part and tilting of the device during reading of the face of the device.19
The digital inclinometer is a handheld device placed against a body surface to measure angular position relative to the vertical or horizontal plane. The digital inclinometer does not require alignment with multiple reference points and requires only one hand, making it easier to use than the SG. Many digital inclinometers can store multiple measurements, improving efficiency by allowing multiple motions to be assessed without needing a break to record each motion. Unlike goniometry, there are no universally accepted procedures for using inclinometers to assess joint ROM. A digital inclinometer used in clinical and research settings, referred to as a medical inclinometer (MI), is expensive, with costs exceeding $400. A builder’s digital inclinometer (BI) commonly used by construction workers operates under the same principle as a MI and is much less expensive, ranging in cost from $10 to $50.
Purpose
Studies examining the reliability and time efficiency of the SG, MI and BI are not well represented in the literature. The purpose of this study was to investigate the validity, reliability and time required to assess ROM using a SG, MI, and BI. The research hypotheses were as follows: 1) measurements taken using the inclinometers would be faster than measurements taken with the goniometer; 2) inclinometer measurements would be more reliable than goniometric measurements; 3) measurements with the inclinometers would be highly correlated; 4) measurements taken with inclinometers would be correlated with goniometric measurements.
METHODS
Fifty healthy individuals (34 females and 16 males, 23 to 58 years of age) were recruited from a local university setting to participate in the study. To be eligible, participants were at least 18 years of age with no reported current shoulder, elbow, or forearm pain limiting movement. Participants wore short-sleeve shirts to allow identification of necessary bony landmarks for testing. The devices used for ROM assessment were SGs (360°, six-inch and 12-inch), MI (Acumar, Grayline Medical; Norwalk, CA), and BI (AccuRemote, San Clemente, CA) The study was approved by the Institutional Review Board of a public university. All participants provided written informed consent prior to participation.
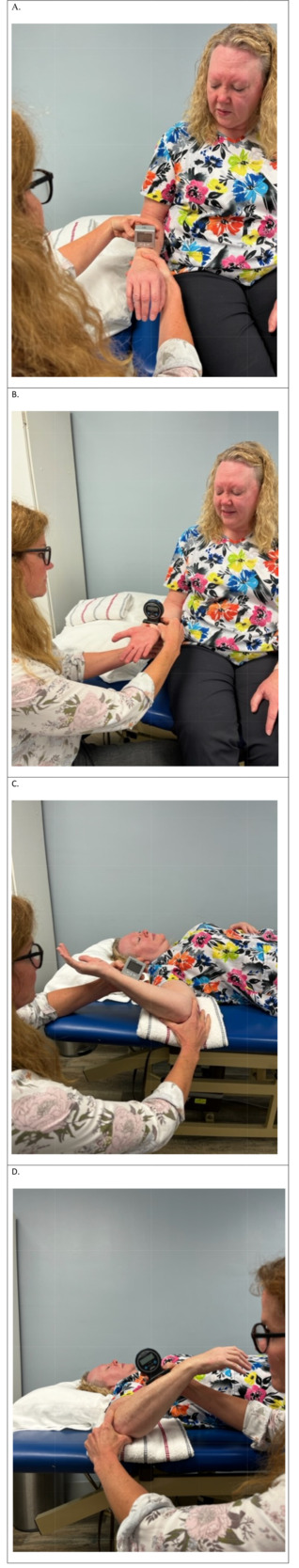
All measurements were taken by the same tester with more than 30 years of clinical experience as a physical therapist. All measurements were performed according to the preferred position as described by Norkin and White.20 For this study, shoulder internal/external rotation was considered as glenohumeral internal/external rotation. A 12-inch SG was used for assessing shoulder internal/external rotation and 6-inch SG was used for assessing forearm pronation/supination. The inclinometers were placed on the dorsal surface of distal forearm for shoulder internal rotation and forearm pronation and on the ventral surface of the distal forearm for shoulder external and forearm supination (Figure 1).
The order of joint testing was as follows: forearm pronation, forearm supination, shoulder external rotation, and shoulder internal rotation. The order of devices was randomly assigned for each participant. Immediately prior to assessment of each motion, the participant performed three repetitions of active ROM, followed by one repetition of passive ROM performed by the tester. With the participant in the standard test position, the participant performed a warm-up of three repetitions of active ROM, followed by one repetition of passive ROM performed by the tester to take the joint to end range of motion prior to passive ROM measurement. The warm-up was performed to minimize the increase in ROM with repeated measurements. The tester then positioned the participant in the neutral starting position for the given joint motion. For the first repetition with each device, the tester signaled the timer to begin timing the assessment and passively moved the participant to the end range of motion and aligned the measurement device. Once the device was properly aligned at the end of joint passive ROM, the tester signaled the timer to stop. The timer then read and recorded the amount of passive ROM as well as the time required to the nearest second.
The digital display on the MI ranged from 0-180° in 1° increments. The digital display of the BI ranged from 0.0° to 90.0° in 0.1° increments, with ROM beyond 90° displayed as –89.9° to –1.0°. For ROM greater than 90°, the recording researcher calculated the ROM (e.g. for a display reading of -80°, the recorded ROM was 100°). All information was recorded on a data recording form, transferred to a spreadsheet, and uploaded to the Statistical Package for the Social Sciences (SPSS) version 28.0 for analysis.
Statistical Analysis
The Shapiro-Wilk test indicated a non-normal data distribution; therefore, the Wilcoxon Signed Rank test with an alpha level of 0.05 was used to determine the difference in the time required for each motion with each device. Intrarater reliability for each device was calculated with the intraclass correlation coefficient (ICC) (3,k) two-way mixed model with absolute agreement using the three trials for each motion.21 Construct validity, determined by correlations between devices, was assessed using the ICC.22 Interpretation of correlation strength varies among authors.8,21–23 For this study, reliability was considered excellent for ICC values > 0.90; good for values 0.70-0.89; acceptable for values 0.60-0.69; fair for values 0.50-.59 and poor for values <0.50.
The absolute reliability of each device was quantified using the standard error of measurement (SEM) and minimal detectable change (MDC).22 The SEM is a measure of how much test scores vary about a “true” score. The SEM was calculated using the formula: SEM = standard deviation * √(1-r).22 The MDC is the smallest change that can be considered a true change as opposed to change due to measurement error. The MDC was calculated using the formula: MDC = SEM * 1.96 * √2 to determine the magnitude of change that would exceed the 90% confidence interval.22 Given the normal distribution of the difference scores between devices, the level of agreement between the BI and MI was visualized using Bland-Altman plots with 95% limits of agreement calculated using the formula: mean difference ± 1.96 * standard deviation.24
RESULTS
Table 1 provides the means and standard deviations of ROM measurements for each motion with each device. On average, the mean difference between the inclinometers was less than 2°. In contrast, the average mean differences between the SG and BI were 3° and 5° for the MI.
Research Hypothesis 1: Time Required
Figure 2 demonstrates the mean time required to perform each measurement with each device. The Wilcoxon Signed Rank test indicated that the BI and MI inclinometers required significantly less time than the goniometer (p < 0.001) for all motions. Assessment using the MI required significantly less time than the BI for both pronation and supination, p = 0.004 and p = 0.005, respectively. Therefore, the first research hypothesis was supported.
Research Hypothesis 2: Intrarater Reliability of Devices
The results of intrarater reliability with ICC and 95% confidence intervals for each device are listed in Table 2. For convenience, the SEM and MDC for each motion and each device have been included in Table 1. While all devices had good reliability (ICC > 0.70), SG measurements were less reliable than inclinometer measurements. Except for shoulder external rotation, the MI was the most reliable device for all motions, with all but one motion (supination) exceeding 0.90, equating to excellent reliability. While slightly better for the inclinometers, absolute reliability was good considering the low SEM across devices, ranging from 1.4° to 3.5°. The MDC and was low across devices, ranging from 1.7° to 2.8°. Therefore, the second research hypothesis was supported.
Research Hypothesis 3: Correlations Between Inclinometers
Inter-device correlations are listed in Table 3. Correlations were highest between the BI and the MI. The ICC values for pronation, supination, and shoulder internal rotation were all > 0.70, indicating good correlation between the BI and the MI. The correlation between inclinometers for shoulder external rotation was slightly less at 0.680. Therefore, the third research hypothesis was partially supported.
Research Hypothesis 4: Correlations Between the Goniometer and Inclinometers
As listed in Table 3, the correlations between the SG and the BI ranged from a low of 0.434 for forearm pronation ROM to a high of 0.727 for shoulder internal rotation. The correlations between the SG and the MI were similarly low, ranging from 0.377 for forearm pronation to 0.647 for shoulder external rotation. Therefore, the fourth research hypothesis was not supported.
Data Visualization
The Bland-Altman plots in Figure 3 and Figure 4 demonstrate the 95% limits of agreement between the BI and MI. More than 95% of measurements fall within these limits and are evenly distributed both above and below the mean throughout the ranges of motion. For pronation, supination, and shoulder external rotation, the mean differences between the BI and MI were less than 2°, with most measurements within ± 5°. For shoulder internal rotation, the mean differences were approximately 4°, with most measurements within ± 5°.
DISCUSSION
Accurate, reliable, and efficient measurements are important to detect motion deficits and changes over time. The SG is readily available in most clinics, has standardized methodology, and low cost. Use of the SG is taught in many medical professions relying on joint ROM assessment to determine baselines and the impact of interventions. However, the time efficiency and comparison of the SG to multiple types of inclinometers has not previously been fully described.
In this study, the inclinometers were more than twice as fast as the SG for measuring range of motion, equating to 3.2 to 6.0 seconds per measurement. Consider a clinician performing pre/post treatment ROM measurements for two motions, for example shoulder internal and external rotation, this could mean saving half a minute of time. When considering the course of a full-time work week, the time required equates to over 30 minutes that could be spent on patient management, clinical documentation, or limiting the need for overtime. The saving of time should entice both clinicians and clinic managers to incorporate inclinometers into clinical practice. While there was a statistically significant difference between the BI and MI for measuring pronation and supination, the nearly half second difference is not clinically relevant, such that, the adoption of either inclinometer device would improve efficiency.
Intrarater reliability for each device was good to excellent with the highest reliability demonstrated with the MI (average ICC value of 0.914), followed closely by the BI (average ICC value of 0.908), and the lowest ICC found with the SG (average ICC value of 0.809). In this study, the SG was the least reliable assessment tool; a result consistent with other studies that found inclinometry to be more reliable than goniometry.25,26 Nonetheless, the SG is the most used clinical tool to assess ROM. Cools et al.27 found high SG intrarater reliability for shoulder rotation (ICC ranging from 0.850 to 0.990). However, for that study, two individuals performed the measurements: one providing stabilization and one performing the measurement. In clinical practice, it is rare to have the assistance of another individual when performing ROM assessment.
Measurement error in the current study was low, with an MDC from 1.8° to 2.8 for the SG and from 1.7° to 2.0° for the inclinometers. Cools et al.27 reported a greater MDC for shoulder rotation, ranging from 4.4° to 8.0° for the SG and 4.0° to 6.4° for the inclinometer. Likewise, both the SEM and MDC for shoulder rotation with the SG and inclinometers in the current study were lower than those found by Correll et al.13 when using a SG and the Halo® device.
As expected, measurements taken with the BI and MI were more highly correlated with each other than with the SG. The average ICC value for BI and MI was 0.703 indicating good, but not excellent, consistency between devices. One reason for the small differences between the BI and MI could be due to the different device contact surfaces. The flat contact surface of the BI may allow for unintentional tilting of the device and thus align differently with body contours compared with the central rounded cutout of the MI. While the correlation between inclinometers was lower than expected, the mean differences between devices were quite small (0° to 4°). Clinically, these differences are unlikely to be relevant. However, given individual measurements varied by as much as 5°, it is recommended that clinicians use the same type of inclinometer when measuring a patient to ensure a change, or lack of change, has occurred. These suggestions are consistent with recommendations of other studies.3,28 Given the low cost and high reliability of the BI, clinicians and clinic managers may consider use of a BI rather than investing in the more expensive medical inclinometer.
Strengths
This study included participants of a broad range of ages without regard to prior injury or surgery, theoretically resulting in a wider range of scores than if only young, healthy individuals were tested. Having more variability in ROM is expected to prevent a misleadingly low reliability coefficient due to low score variability.22 This study utilized one tester who was blinded to measurement results, reducing the potential for variations in passive force application to achieve end ROM.
Limitations
This study included participants who were symptom free. Therefore, it is unclear if the results might apply to individuals who experience pain with testing. Since this study utilized only one tester, it is not possible to determine interrater reliability. Additionally, the tester was an experienced clinician and results may not generalize to an inexperienced clinician. The BI used in this study is typical of builder’s digital inclinometers, in that the device cannot record measurements greater than 90°. Angles greater than 90° required the recorder to calculate the true measurement which could have been a source of error. It is not known if other types of BI would perform similarly to the one used in this study.
CONCLUSION
The BI and MI were found to be reliable for measuring pronation, supination, and shoulder rotation. The low correlation between the SG and inclinometers indicates that clinicians should utilize the same device for testing. Because time can be a barrier to clinician measurement and remeasurement during an episode of care, the greater efficiency and reliability of inclinometers warrants consideration as the new measurement standard. In contrast to the SG, inclinometer assessment requires only one hand to manage the device. The MI cost may be prohibitive for routine clinical use. However, the lower BI cost makes the device clinically affordable. Future studies should examine the reliability of a BI capable of displaying angular measurements greater than 90°. Assessment of a greater number of joint motions using the BI and on various patient populations would be beneficial. Given the current lack of standardization, creating and utilizing a standard for patient and inclinometer positioning is recommended to enhance reliability.
Disclosures
The authors report no conflicts of interest.