Introduction
Musculoskeletal (MSK) ultrasound is rapidly gaining recognition as a primary investigative tool for diagnosing a broad array of MSK disorders, particularly those affecting the tendons, ligaments, muscles, and joints. This advancement in medical technology provides a real-time, non-invasive, cost-effective, and dynamic approach to visualize soft tissue structures that might be challenging to investigate using traditional imaging modalities. A specific area where MSK ultrasound is making considerable strides is in the diagnosis of patellar tendon injuries. Patellar tendon injuries can be frustrating for both athletes and physicians to diagnose, as they often present with subtle signs and symptoms. Accurate diagnosis is important for proper treatment of the condition, as the symptoms associated with patellar tendinopathy are highly variable and easily missed. Because the signs and symptoms can be subtle, MSK ultrasound is a useful tool for helping to accurately assess patellar tendon injuries. MSK ultrasound allows for detailed visualization of the patellar tendon, providing clinicians with crucial information regarding the extent of the injury. In this article, we explore the role and benefits of this non-invasive imaging technique in the detection and evaluation of patellar tendon injuries.
Understanding Patellar Tendon Injuries
The patellar tendon, a crucial part of the extensor mechanism of the knee, plays a vital role in facilitating knee extension. Patellar tendon injuries, ranging from tendinopathies to partial or complete ruptures, can significantly impair knee function and quality of life. The successful management of these injuries hinges on an accurate and timely diagnosis. Traditional imaging modalities like plain radiographs (X-rays) can offer limited information, as they are primarily focused on evaluating bone structures. Magnetic Resonance Imaging (MRI), although excellent for soft tissues, might not always be accessible due to its cost, availability, and contraindications in some patients. One of the key advantages of MSK ultrasound in diagnosing patellar tendon injuries is its ability to offer high-resolution, real-time imaging of the patellar tendon. This non-invasive imaging technique makes it easier to detect changes in tendon tissue composition and smaller tears that may not be visible on other imaging modalities such as MRI or through the physical examination alone. Additionally, MSK ultrasound can be performed quickly and conveniently, eliminating the need for patients to schedule separate appointments for imaging. The dynamic assessment allows clinicians to visualize the tendon’s structure and function in both static and active states. It can readily identify changes in the structure of the patellar tendon, such as thickening, thinning, or disruption, which could suggest pathology.
The Role of MSK Ultrasound in Diagnosis
When it comes to diagnosing injuries, accuracy is key. This is where MSK ultrasound comes in handy for patellar tendon injuries. This advanced imaging technique allows medical professionals to examine the internal structures of the body in real-time, producing detailed and accurate images of the patellar tendon. With its ability to identify pathologic changes over time and to help guide treatment, MSK ultrasound has become an integral part of the management of these types of injuries. By providing a detailed, real-time view of the anatomy and pathology within the tendon, the use of MSK ultrasound can help to ensure that patients receive timely and appropriate treatment in order to achieve the best possible outcomes.
-
Detection of Injuries: MSK ultrasound can effectively identify structural changes in the patellar tendon, such as thickening, thinning, or disruption. Hypoechoic regions within the tendon, a classic sign of tendinopathy, can be easily visualized. In cases of complete or partial tears, MSK ultrasound can delineate the size and location of the tear.
-
Assessment of Vascularity: Using Doppler imaging, an essential component of modern ultrasound machines, MSK ultrasound can assess vascularity within and around the tendon. This capability can help differentiate normal from abnormal tendons, as neovascularity is often seen in tendinopathy and healing tendons.
-
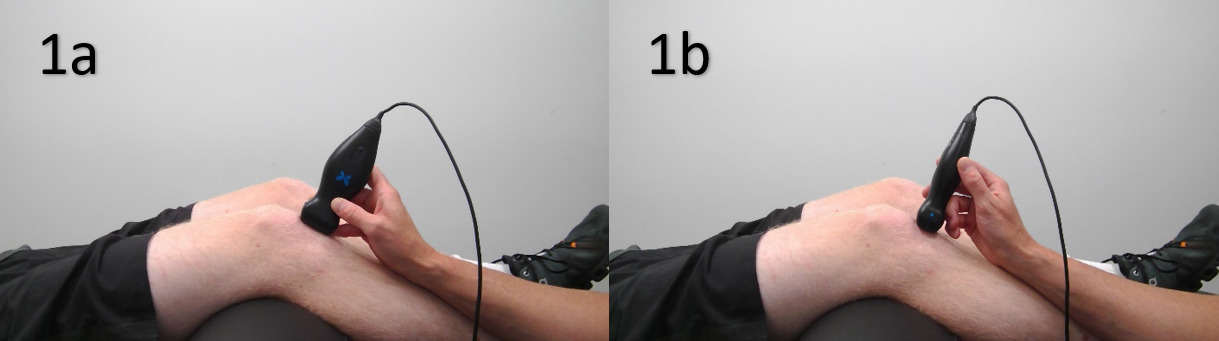
Dynamic Assessment: Unlike other imaging modalities, MSK ultrasound can assess the patellar tendon while the patient is actively moving their knee. This feature is particularly useful in cases of fat pad impingement or patellar instability, where the pathology might only be evident during specific movements or positions.
-
Guidance for Interventional Procedures: In addition to diagnostic uses, MSK ultrasound can guide clinicians during interventional procedures such as injections or aspirations, increasing the accuracy and safety of these treatments.
MSK ultrasound is also helpful for monitoring post-treatment progress since it can be used to track changes in tendon structure and composition over time. This is important for ensuring that the treatment plan is having the desired effect and can aid in determining if a different course of action may be necessary. In addition, MSK ultrasound can also help to identify potential areas of re-injury or tendinopathy which may require further attention or intervention. MSK ultrasound can therefore be an essential part of post-treatment management for patellar tendon injuries.
Limitations and Considerations
Despite its numerous advantages, it is important to acknowledge that the efficacy of MSK ultrasound is highly operator-dependent, requiring significant expertise and training for accurate interpretation. Specifically, one should ensure that the transducer is positioned correctly, as an inaccurate positioning can lead to incorrect diagnosis. Additionally, it is important to be mindful of the ultrasound settings being used, as incorrect settings can result in poor image quality. Tendons are also susceptible to anisotropy, an imaging artifact that may lead to an incorrect diagnosis of a tear. Finally, interpretation of the ultrasound image can also pose a challenge, as patellar tendon injuries can sometimes appear similar to other injuries. With these considerations in mind, practitioners can ensure that they are making the most of MSK ultrasound in diagnosing patellar tendon injuries.
Conclusion
In conclusion, MSK ultrasound is an important and invaluable tool in the assessment of patellar tendon injuries. With its advantages of high-resolution visualization, cost-effectiveness, accessibility, real-time assessment, and dynamic images of the patellar tendon, it is becoming a first-line imaging tool for many clinicians in the assessment of soft tissue structures. It can provide detailed information regarding the structure and composition of tendons that other imaging modalities cannot, as well as guide treatment decisions and monitor response to therapy over time. As such, MSK ultrasound should be considered as part of any comprehensive evaluation and management plan for patellar tendon injuries. By providing a real-time view of the anatomy and pathology within the tendon, MSK ultrasound can help to ensure that patients receive timely and appropriate treatment to achieve the best possible outcomes. While MSK ultrasound has become an essential tool in the diagnosis and management of patellar tendon injuries, continual research is necessary to further refine its use. Advancements in technology and imaging techniques may provide even greater resolution and clarity, aiding in our ability to diagnose and manage patellar tendon injuries effectively.

.png)
.png)
.png)
_and_short_axis_(sax).png)
.png)
.png)
.png)
_and_short_axis_(sax).png)