INTRODUCTION
Femoroacetabular impingement (FAI) is a common cause of hip pain in the adolescent and adult populations; this pain can impair daily function and ultimately impact athletic participation. The prevalence of FAI is unclear within current literature, but a recent meta-analysis found that the prevalence of FAI in young athletes with non-arthritic hip pain is 61.3%.1 Conservative and surgical management of FAI are both common means of treatment with evidence to support the efficacy of either option. There is, however, conflicting evidence regarding the superiority of one option over the other. Several studies have shown that surgical intervention may provide superior outcomes to physical therapy.2–4 However, the magnitude of success from surgical intervention may be somewhat limited. Palmer et al. showed that only 51% of those treated surgically saw a statistically significant improvement in functional outcomes with the extent of difference between the two treatment options varying based on which functional outcome measure was assessed.2,3 Additionally, several recent meta-analyses have shown similar results, but the quality of their methodology have been called into question.5–10 Saueressig et al. re-analyzed the data used in these meta-analyses and found no statistically significant difference in outcomes between surgical intervention and physical therapy.11 Other studies have shown that physical therapy may yield superior results to intra-articular injections in relation to pain and function, however the generalizability of these results is limited by short-term follow up.12,13
Despite conflicting evidence, when patients do not respond to conservative methods of treatment, they will often seek surgical intervention. The process of returning to sport after hip arthroscopy is important for athletes, surgeons, and rehabilitation providers. For athletes undergoing hip arthroscopy for FAI, there is not a standardized return to sport testing protocol within the literature.
According to a cross-sectional cohort study by Ishoi et al. nearly 84%-87% of athletes will return to sport following hip arthroscopy; however, only 57% of athletes return to their preinjury level with only 16.9% of them reporting their sport performance to be optimal.14 There is ambiguity in appropriate return to sport time frames which ranges in the available literature from 3 to 12 months, with the most common time to return being 7.4 months.15,16 This discrepancy is due to a lack of consistency within the definition of return to sport following surgical intervention, as well as a lack of standardization within return to sport criteria and testing protocols. There have been several publications within the rehabilitation literature suggesting future studies adopt more concise descriptors within the umbrella term “return to play” or “return to sport” in order to provide an accurate assessment of the athlete’s outcome after surgery regarding their achieved level of play within their desired sport.17,18 To help provide clear descriptors, the authors will use the terminology “return to sport” provided by Ardern et al.17 For this clinical commentary, the term “return to sport” most accurately depicts the desired level of activity achieved within the stated criteria-based testing protocol.
A 2018 systematic review of 22 studies on return to sport after hip arthroscopy found that 54.5% did not provide guidance on return to sport duration or testing protocols after surgery. Of the studies that did provide a return to sport timeframe, 36.4% recommended four months. Only three studies provided information on reproducible testing and only two studies met the author’s four measures on return to sport criteria.15
The need for a standardized criteria-based testing protocol was also supported by a 2021 systematic review by Davey et al. that assessed the current state of return to sport following hip arthroscopy. The authors found the overall return to sport rate was 84.5% and most athletes returned to sport in 6.6 months. The most common criterion used to determine readiness to return to their previous sport was time, with no standard objective criterion present in the literature. Unfortunately, most of the studies included by Davey et al. reported generic or vague criteria on return to sport (pain free, full strength, full range of motion, and have completed functional testing) and about one fourth of the included studies did not report any criteria on return to sport guidelines.19 The authors of this commentary believe that a safely guided return to sport testing protocol should include criteria-based objective measures with consideration of biological healing time.
A higher rate of return to sport has been reported among professional athletes compared to lower-level athletes.20 There was also a higher return to sport in the pediatric population and those with a short duration of pre-operative symptoms.16 Despite the high rate of return to sport following hip arthroscopy in these two populations, there are athletes who will fail to return to their preinjury level of sport. Weber et al. found that 12% of athletes will not return to sport. Of those 12%, 74.3% will not return due to hip related issues with 47.3% reporting persistent pain as their main reason.21 Unfortunately, these statistics lack generalizability as only two of the 20 articles included in this systematic review reported the age of the athletes who did not return to their sport.21
The primary limitations in the return to sport literature related to the hip can be attributed to low quality evidence, lack of consistency within the definition of return to sport, wide variety in surgeon preferences, and wide variety in rehabilitation protocols. Currently, a comprehensive, criteria-based, return to sport testing protocol that utilizes objective measures to ensure athletes are safe for return to sport does not exist. The goal of the authors was to develop a criteria-based testing protocol following hip arthroscopy utilizing parameters best supported in the literature. It is the authors’ hope that this new criteria-based testing protocol will create consistency across care, decrease re-injury rates and increase the percentage of athletes successfully returning to sport. Therefore, the purpose of this clinical commentary is to propose a criteria-based testing protocol following a hip arthroscopy for impingement to be continually assessed from early rehabilitation through return to sport.
CRITERIA OF PROPOSED RETURN TO SPORT TESTING PROTOCOL
The following five criteria were identified through literature review as key parameters of a return to sport testing protocol: range of motion, strength, functional testing, psychological readiness, and time. These criteria are then further divided into specific testing components which are described in detail in individual sections below. All passing criteria recommended by the authors of this commentary are in accordance with previously published literature on each individual testing component. The full testing protocol which includes each criteria category, test components and passing criteria is outlined in Table 1.
CRITERIA 1: RANGE OF MOTION
To date, there are no published data on expected range of motion of the hip following surgery to correct FAI. It has been shown that the pathology of FAI causes a significant difference in hip range of motion in the planes of flexion, abduction, extension, external rotation (ER) and internal rotation (IR).22,23 Clinicians should consider contralateral hip FAI morphology or range of motion limitations when clearing an athlete in this category.22
The recommended passing criteria is pain-free active and passive range of motion within five degrees of the contralateral hip in all planes with consideration to any contralateral hip morphology. In this situation, clinicians can reference previously established normative ranges of motion for the hip joint bearing in mind the influences of factors such as age, gender, and race.24,25
CRITERIA 2: STRENGTH
Strength is an often-included criteria as a part of return to sport testing following injury or surgery. The hip is unique in that it has movements in all three planes: sagittal (flexion/extension), frontal (abduction/adduction) and transverse (internal/external rotation). The authors suggest that using manual muscle testing (MMT) alone is not sufficient in determining the full extent of an individual’s strength across these three planes as it is an isometric test and subjective in nature. As an initial test, using a grade of 5 out of 5 MMT may be an indicator that the athlete is ready to progress to a more advanced stage of their rehabilitation. The authors of this commentary recommend more objective testing of an athlete’s strength when determining readiness to return to sport which is described in detail below.
Hand-held Dynamometry
Hand-Held Dynamometry (HHD) has been well established and validated as an objective method of testing strength in individuals.23 When possible, the device should be fixated against a stable base to avoid any error in measurement from clinician pressure or losing joint position during isometric testing.22,23 Not only should the clinician look at the amount of force produced but also the quality of muscle contraction as well as any compensatory movements or patterns noted during the test. Proper setup for HHD strength testing of the hip has been previously described using a belt with an emphasis on a fixed and stable base.22,23 The authors encourage using HHD to test all six motions across three planes.
The recommended passing criteria is a limb symmetry index (LSI) of > 90%.
Single Leg Bridge Test
The Single Leg Bridge Test (SLBT) has been documented to assess hamstring performance in high level athletes.26 The test is described with the athlete positioned supine, the leg being tested on a box 60 cm high and knee flexed to 20 degrees. Once in the proper test position, the athlete performs as many reps as possible on both sides. The test is stopped by the clinician at their discretion for improper technique. The authors of this commentary recommend this test to be done in two ways. First, early in the rehabilitation process as a screen to assess the athlete’s pelvic control and general quality of movement. The athlete is subjectively graded “pass” or “fail” on glute activation, maintaining lumbopelvic neutral, maintaining neutral pelvic rotation, and achieving full excursion of hip extension. Second, as the athlete continues through their rehabilitation program, it should be performed as described by Freckleton et al. to identify any deficits in posterior chain endurance.26 It is the author’s intent that the results of this test will aid in determining the athlete’s readiness to progress into more advanced limb control tasks during their rehabilitation.
Although the above test has been shown to be predictive of hamstring injuries, the authors suggest utilizing it as a way to screen gluteus maximus performance in the early stages of the rehabilitation process. A systematic review by Macadam et al. demonstrated that performing a bridge recruits the gluteus maximus muscle albeit in different amounts based on setup.27 Performing a single leg bridge has been shown to provide high EMG of the hamstring muscle group as well as the gluteus maximus.28 Performing a single leg bridge with the knee fully flexed at 135 degrees, foot flat on table, and contralateral leg held in neutral with the knee straight was found to have the highest EMG activity of the gluteus maximus while minimizing EMG activity of the hamstrings. This position was also found to have a moderate amount of gluteus medius activation.28 The authors suggest modifying the SLBT testing position to have the knee flexed to 135 degrees to better bias the gluteus maximus. However, it is important to note that this adaptation has not been formally studied to date.
The recommended passing criteria is a LSI of >90%.
The Bunkie Test
Core strength and endurance is a key component of rehabilitation following hip arthroscopy; however, there is currently no gold standard for core assessment within return to sport testing. For this return to sport testing protocol, the authors recommend using the Bunkie Test as it is a comprehensive series of movements that assess an individual’s core strength and stability in the frontal and sagittal planes.29 It is a series of five tests that can also be utilized as exercises for athletes if weaknesses are identified and it incorporates static muscle function, static muscle length, postural alignment, and spinal stability.29 The test positions are shown in Figure 1 and an in-depth description of the setup for each test can be found by referencing the prior work by Ronai.29
The Bunkie Test has been shown to be a reliable measure of core endurance in a healthy patient population30 but more in-depth reliability and validity studies are needed to assess efficacy in an injured patient population, and specifically for patients with hip pathology, for purposes of this return to sport testing protocol. Brumitt demonstrated effectiveness of the Bunkie Test in identifying core and hip weakness in a female distance runner with unilateral back pain in a case report.31 Therapeutic exercise interventions were prescribed based on the results and then the Bunkie Test was readministered, resulting in the improved isometric hold times and a resolution of the subject’s back pain.31
The recommended passing criteria is a pain-free, isometric hold of 40 seconds for the anterior power line, posterior power line, posterior stabilizing line and lateral stabilizing line and 20-30 seconds for the medial stabilizing line otherwise, muscle imbalance may be present, in accordance with normative data reported by Ronai.29
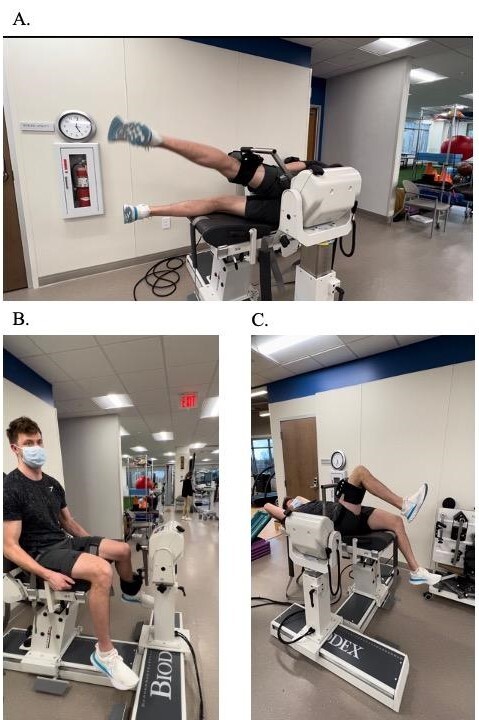
Isokinetic Testing
For objective testing of muscle strength, isokinetic dynamometers are the gold standard. In addition to providing a patient’s peak torque to compare their uninvolved to involved limb, isokinetic assessments allow us to normalize peak torque to body weight for comparison to other individuals as well as to establish agonist/antagonist ratios through different angular velocities. Isokinetic dynamometers are also considered effective for use during rehabilitation to address muscle function. A great deal of research has been generated in the field of rehabilitation and sports performance with regard to isokinetic testing with the knee joint being the most studied and to a lesser extent the hip.32 Although less studied, isokinetic testing of hip musculature does appear to be reliable and valid in individuals with FAI. Meyer et al. showed good to excellent reliability for isokinetic testing of the hip in the directions of hip flexion/extension and abduction/adduction.33 Casartelli showed that patients with FAI have significantly lower maximum voluntary contraction (MVC) strength than controls for hip adduction (28%), flexion (26%), external rotation (18%) and abduction (11%).34 The authors recommend testing in the directions of flexion/extension, abduction/adduction and IR/ER. Meyer showed that testing at velocities of 60 degrees/second for 3 reps and 120 degrees/second for 5 reps is very reliable,33 therefore the authors recommend testing using these parameters. The testing directions are depicted in Figure 2.
The recommended passing criteria is a peak torque LSI > 90% for each testing direction.
CRITERIA 3: FUNCTIONAL TESTING
The Step-Down Test
The step-down test is a common functional performance test used in the clinical setting to assess basic dynamic movement patterns of the trunk and lower extremity. Previous authors have shown the test to be a reliable and valid functional performance test in the evaluation of physical function for patients with nonarthritic hip pain.35 It should be noted that those who pass the step-down test report less pain and greater function during sports related activities as assessed by a Visual Analog Scale and the Hip Outcome Score-Sports Subscale.35
The testing procedure is carried out in the manner outlined by McGovern et al.36 A single evaluator assesses the overall test performance of the individual’s affected side; this is determined by the individual’s balance, balance or acceleration provided by heel contact, gross arm deviation, and their ability to perform the test. Each repetition is then graded as “positive” or “negative” based on five criteria: trunk movement (forward lean, lateral rotation, lateral flexion, thoracic rotation), posture of the pelvis (tilt or rotation), posture of the hip joint (adduction or internal rotation), posture of the knee (knee valgus or tremor) and depth of squat (inability to contact heel to ground).
The authors recommend following the test parameters outlined by McGovern et al, which means that for an individual to pass, the evaluator must first grade the overall impression of test performance as passing. Second, a total of four out of the five specific criteria must be negative for deviation. Third, a passing grade of at least one out of the three tests is required.36
Y-Balance Test
The Y-Balance test (YBT) is a functional test developed from the Star excursion balance test (SEBT) to improve reliability and field expediency of the SEBT.37 The YBT was simplified to use only the most reliable three reach directions of the SEBT (anterior, posteromedial, posterolateral). The test is intended to assess dynamic postural control and has been shown to be predictive of lower extremity injuries in young, athletic populations.38 There is also evidence that demonstrates a correlation between reach distance in both the posterior-medial and posterior-lateral direction and hip extension and abduction strength.39,40 The authors recommend using The YBT instrument (FunctionalMovement.com, Danville, VA) for more reliable and valid testing. To score the YBT, first calculate the average reach distance in each direction in centimeters, by taking the average of three trials for each direction. Then, calculate the distance in each direction as a percentage by taking the average distance in each direction, divided by the patient’s leg length, multiplied by 100.37
The recommended passing criteria is >94% symmetry and <4cm difference in reach difference between the involved and uninvolved extremity.38
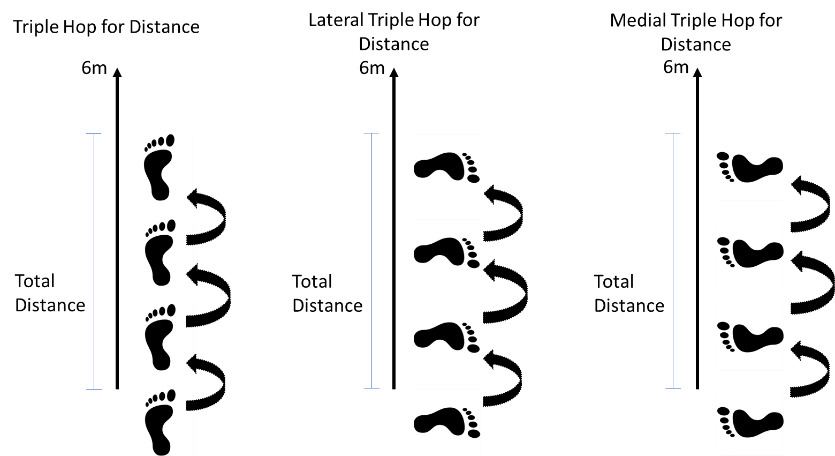
Hop Testing
Functional performance tests have been commonly used to identify impairments related to ankle or knee injuries and determine the readiness of an athlete to return to sport after injury.39,41–44 Multiple authors have determined hop testing to be reliable, correlating with lower extremity strength as well as functional performance.39,45–50 There may also be a correlation between functional testing and injury prevention. In ACL rehabilitation, passing a battery of tests which include hop testing has been shown to reduce the odds of an ipsilateral ACL graft rupture by 78-84%.51–53 Evidence of their validity in the rehabilitation of hip pathology is scarcer. Therefore, the development of a testing protocol that bases progression of performance on functional tests that inform hip rehabilitation should be prioritized.
The authors recommend utilizing three functional hop tests to determine readiness for progression to higher level activities. These are the triple hop for distance, medial triple hop for distance, and lateral triple hop for distance, these are depicted in Figure 3. The triple hop for distance test is well established in rehabilitation of knee conditions. Although less established in rehabilitation for the hip, triple hop work seems to correlate with hip strength.54 Kollock et al. showed that triple hop work was a strong to very strong indicator of max strength and rate of force development of the hip abductors, adductors, and flexors. The medial and lateral triple hop for distance tests are less established; however, have been shown to be valid and reliable in individuals with hip pathology.54 Kivlan et al. showed that both tests were reliable (ICC: medial hop 0.96; lateral hop 0.93) with the medial hop test showing a significant difference in hop distance between the involved and uninvolved sides in dancers with hip pathology.55 These tests are intended to evaluate the individual’s performance both qualitatively and quantitatively. The individual begins by standing on the uninvolved limb. They hop three times consecutively for distance in the predetermined direction and hold the last hop for five seconds. The assessor measures the distance hopped on each trial in centimeters and the best of the three trials is used for assessment. The procedure is then performed on the involved limb. The best trial of each extremity is compared. Each trial of the test is also graded qualitatively by the assessor. Each performance is scored through observation as “good”, “fair” or “poor.” A grade of “poor” is considered a “fail” and is not considered for assessment.
The recommended passing criteria is a LSI of > 90% for distance hopped and qualitative rating of “good” for each of the three hop tests.44
CRITERIA 4: SELF-REPORTED FUNCTION AND PSYCHOLOGICAL READINESS
Self-reported Function (Patient-Reported Outcomes)
Self-reported functional questionnaires were designed with the intent of assessing a patient’s ability to return to an active lifestyle through obtaining subjective measures of symptoms and function, as well as emotional and social health status. Unfortunately, many questionnaires assessing the function of patients with hip pathology were designed with a focus on lower-level activities with little consideration for the requirements of a younger, more athletic population. The International Hip Outcome Tool (iHOT-12) is a good example of such a tool. It has been shown to be valid, reliable, and responsive to change in young adults with various hip conditions.56 It was designed to assess Activities of Daily Living in an active population, however, has limitations in assessing athletes who participate in higher level sports-related activities. The Hip Outcome Score (HOS) is another validated functional scale that consists of an ADL subscale and Sports subscale. Martin et al. have shown the HOS to be a valid assessment tool for individuals with the diagnosis of a labral tear as well as for those who have undergone hip arthroscopy. Martin et al. also found that the HOS was able to differentiate between functional abilities of individuals, depending on their current activity level, surgical outcome, and age at a follow-up assessment performed more than three years after surgery on average.57 The authors propose that the iHOT-12 be used for assessment in the initial phases of rehabilitation, as it is a good tool for monitoring ADL progress. The authors then recommend transitioning to the Hip Outcome Score - Sports Subscale (HOS-Sports) in the later phases of rehabilitation to monitor self-reported function as it relates to sport specific tasks.
The recommended passing criteria is a score of >90% ability (or <10% disability) on these questionnaires, with a higher score indicating better function.
Psychological Readiness
A key factor in returning any athlete back to sport is psychological readiness. Fear of re-injury and loss of confidence has been shown to significantly affect an athlete’s readiness for returning to sport, regardless of their physical state.58 Fear of re-injury has been studied in athletes returning after Anterior Cruciate Ligament (ACL) surgery but data are sparse in athletes returning to sport after FAI surgery. Assessing the psychological milestones of an athlete is imperative in the clinician’s efforts to ensure successful return to sport. The Hip Return to Sport After Injury Scale (Hip-RSI) was adapted from the ACL-RSI and is an easily administered scale that is intended to be used alongside functional tests and measures and other patient reported outcomes to determine readiness for successful return to sport. The Hip-RSI has been found to be both reliable and valid for assessing psychological readiness for return to sport following hip arthroscopy.59
The recommended passing criteria is a score of >90% ability (or <10% disability), with a higher score indicating a greater level of psychological readiness.
CRITERIA 5: TIME
There is no current evidence to support the appropriate time frame to initiate return to sport testing following hip arthroscopy. It is the author’s suggestion that the Criteria 1-4 are assessed throughout the athlete’s rehabilitation to identify specific deficits, impairments and performance limitations to ensure the patient is progressing appropriately toward return to sport goals. Taking biological healing times and rehabilitation protocol progressions into account the following time frames are suggested for initiation of return to sport testing.
Clinicians should begin testing the single leg bridge test and step-down test no sooner than eight weeks post-op, after these movements have already been introduced to the exercise program.60 Additionally, testing of the YBT and Bunkie test should occur no sooner than 12 weeks post-op, also after these movements have been added to the exercise program. Athletes should meet all ROM criteria by 12 weeks post-op.60 Strength testing via HHD can occur throughout the patient’s rehabilitation, with the expectation that 90% LSI is achieved by 16 weeks, prior to hop testing. Hop testing is initiated no sooner than 16-20 weeks post-op. Isokinetic testing is completed no sooner than 20-24 weeks post-op once all other previous measures have been achieved to ensure safe testing with proper motion, strength, and in accordance with biological healing of the involved structure.19,61,62
Athletes must be at least five to six months post-surgery (as this is the average time to return to sport reported in the literature19) and have passed all the above outlined criteria before being cleared for return to sport. If a testing component is not passed it should be retested every 7-14 days until a passing criteria/score is achieved. Isokinetic testing is repeated every six weeks until passing scores are achieved.
CONCLUSION
Currently there is no validated return to sport testing protocol following hip arthroscopy, in part due to inconsistencies between physician preferences, rehabilitation protocols, and a lack of high-quality research. After an extensive literature review, the authors have identified the best available tests and measures to be used in return to sport decision making for athletes post hip arthroscopy as a result of pathologic hip impingement and propose a comprehensive criteria-based testing protocol to make informed decisions regarding whether athletes are ready to return to sport. Moving forward, the authors intend to validate the use of this testing protocol as a part of a comprehensive rehabilitation program following hip arthroscopy with the hope that a higher percentage of athletes will be able to return to sport.
Conflicts of interest
The authors report no conflicts of interest.
__posterior_power_line_(b).jpg)

__posterior_power_line_(b).jpg)