Introduction
MSK ultrasound is increasingly recognized as a primary investigative tool for a wide array of musculoskeletal disorders, especially those affecting tendons, ligaments, muscles, and joints. As a real-time, non-invasive, cost-effective, and dynamic imaging technique, MSK ultrasound provides unprecedented insights into soft tissue structures that may be difficult to examine using conventional imaging modalities. The supraspinatus muscle, a crucial component of the rotator cuff, plays an essential role in shoulder function. Injuries to the supraspinatus tendon are relatively common and can lead to pain, weakness, and restricted range of motion. Therefore, accurate diagnosis is vital for effective management. Traditional methods of diagnosing supraspinatus injuries include physical examination, magnetic resonance imaging (MRI), and arthrography. Although MRI has historically been the primary imaging modality, MSK ultrasound has emerged as a reliable alternative, offering real-time dynamic evaluation, accessibility, and cost-effectiveness.
THE ROLE OF MSK ULTRASOUND IN DIAGNOSIS OF SUPRASPINATUS INJURIES
Diagnostic precision is paramount, and herein lies the strength of MSK ultrasound for supraspinatus tendon injuries. A recent meta-analysis concluded that MSK ultrasound is highly sensitive and specific in diagnosing supraspinatus tears, equivalent to MRI imaging.1 MSK ultrasound, with its sophisticated imaging, facilitates precise visualization of the supraspinatus tendon’s internal milieu. This advanced imaging technique allows medical professionals to examine the internal structures of the shoulder in real-time, producing detailed and accurate images of the supraspinatus tendon. With its ability to identify pathologic changes over time and to help guide treatment, MSK ultrasound has become an integral part of the management of these types of injuries. By providing a detailed, real-time view of the anatomy and pathology within the tendon, the use of MSK ultrasound can help to ensure that patients receive timely and appropriate treatment in order to achieve the best possible outcomes. As an asset in the clinician’s diagnostic toolkit, it’s invaluable for detecting pathological shifts over time and is pivotal for therapeutic strategy formulation. Key advantages include
-
Cost-effectiveness: In stark contrast to other imaging modalities like MRI, MSK ultrasound is relatively inexpensive.
-
Dynamic assessment: MSK ultrasound allows for real-time visualization of the rotator cuff during shoulder movement, aiding in the evaluation of tendon function and potential impingements.
-
Immediate Feedback: Instantaneous imaging results facilitate prompt diagnosis and patient communication.
-
Radiation-free: Unlike radiographs and computed tomography (CT) scans, ultrasound does not involve ionizing radiation exposure, making it a safer option, especially for repeat evaluations.
-
Accessibility: Ultrasound equipment is portable and can be used in a variety of clinical settings, including the outpatient clinic, emergency department, and sports events.
Yet, MSK ultrasound isn’t devoid of challenges. Diagnostic accuracy is intricately tethered to the operator’s proficiency, and certain extrinsic factors, such as patient anatomy or equipment settings, can influence image clarity.
Methods: Ultrasound Imaging Technique
The European Musculoskeletal Ultrasound Study Group in Physical Medicine Rehabilitation and Ultrasound Group of the International Society of Physical Medicine Rehabilitation (EURO-MUSCULUS/USPRM) have published guidelines on the basic and dynamic protocols for shoulder scans.2,3 The technique encompasses
-
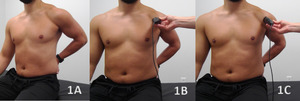
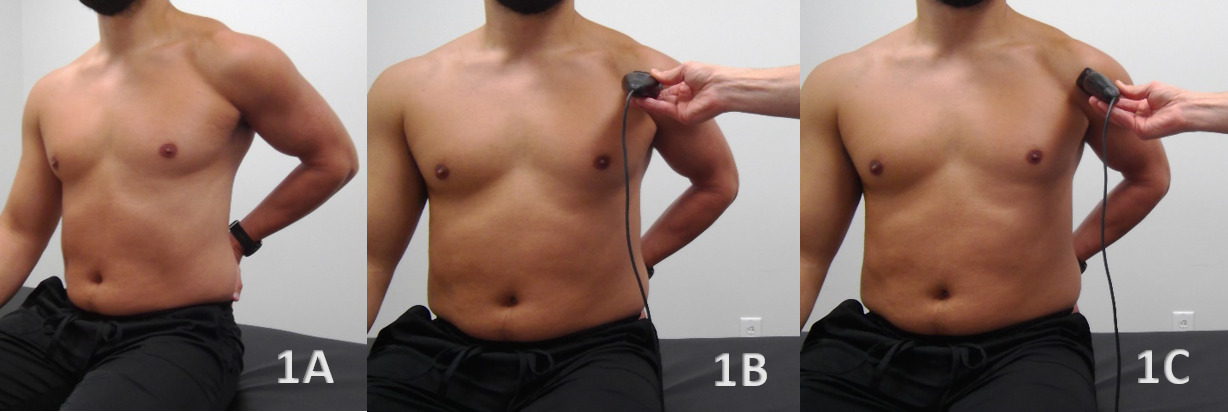
Patient positioning: The patient should be seated with the elbow flexed at 90 degrees and the hand resting on the ipsilateral thigh. This position relaxes the deltoid muscle, improving visualization of the supraspinatus tendon.
-
Transducer selection: A high-frequency linear transducer (7-12 MHz) is recommended for superficial structures like the supraspinatus tendon.
-
Image acquisition protocol: Start by identifying the acromion and the greater tuberosity of the humerus. The supraspinatus tendon can be seen running between these two landmarks. Begin with a longitudinal view of the supraspinatus tendon, scanning from its origin at the supraspinatus fossa to its insertion at the greater tuberosity of the humerus. The transducer is then rotated 90 degrees for transverse views.
-
Dynamic assessment: Perform shoulder abduction and internal/external rotation while observing the tendon’s movement, looking for dynamic impingements or subacromial-subdeltoid bursal effusion.
-
Interpretation: Use a systematic approach to evaluate the tendon for signs of tendinopathy (thickening, loss of fibrillar architecture), partial tears (discontinuity of the tendon fibers), or full-thickness tears (complete disruption of the tendon with fluid filling the defect).
Diagnostic Findings on MSK Ultrasound
Ultrasound can discern normal from pathological tendons, showcasing signs of tendinopathy, partial and full-thickness tears, bursal effusions, calcific tendinitis, and hyperemia. Diagnostic findings on MSK ultrasound include:
-
Normal tendon: A normal supraspinatus tendon appears as a fibrillar, hyperechoic structure.
-
Tendinopathy: Characterized by tendon thickening, heterogeneous echotexture, and reduced echogenicity.
-
Partial-thickness tears: Display as hypoechoic or anechoic defects within the substance of the tendon.
-
Full-thickness tears: Presented by a discontinuity of the tendon or complete anechoic gap in the tendon with visualization of the humeral head beneath.
-
Bursal effusion: An anechoic or hypoechoic region can represent bursitis or fluid from a tear. Elevation of the echogenic bursal line may be noted, suggesting inflammation.
-
Calcific tendinitis: Manifests as hyperechoic foci within the tendon with posterior acoustic shadowing.
-
Doppler imaging: Hyperemia or increased blood flow can indicate inflammation or tendinopathy.
Challenges and Limitations include
-
Operator dependency: Ultrasound requires skilled professionals for accurate interpretation.
-
Cannot visualize structures deep to bone: Ultrasound is limited in visualizing structures beneath bony surfaces.
-
Overlying structures: Fat or scar tissue can occasionally obscure the view.
-
Limited field of view: Smaller field of view compared to MRI.
Discussion
MRI offers superior contrast resolution and a more extensive field of view. MSK ultrasound provides unmatched benefits in dynamic assessment, cost-effectiveness, and immediate results. However, it is operator-dependent, and image quality may vary depending on certain patient populations. With appropriate training and expertise, MSK ultrasound serves as an invaluable tool in the evaluation of supraspinatus injuries. Both modalities can co-exist harmoniously in a diagnostic algorithm, with the choice depending on clinical needs, patient factors, and resource availability.
Conclusion
MSK ultrasound has firmly established its role in the diagnostic pathway of supraspinatus injuries. Its capacity for dynamic assessment, accessibility, and cost-effectiveness makes it a valuable tool in both initial assessment and follow-up evaluations of these injuries. Using MSK ultrasound, healthcare professionals can accurately diagnose supraspinatus injuries and guide appropriate treatment planning. Moreover, MSK ultrasound can help track healing progress and assess the effectiveness of treatment.
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)