INTRODUCTION
Shoulder disorders are the third most common musculoskeletal disorder after low back and neck pain.1,2 When shoulder pain becomes chronic, it may seriously impair work and leisure participation, disturb sleep, and decrease health-related quality of life.3,4 A conservative approach including exercise is the mainstay in the treatment of chronic shoulder complaints.5,6 Although exercise therapy has proven its effectiveness in chronic musculoskeletal pain there is still a lot unknown about which approach is best for conditions of the shoulder.7 Exercise programs mainly focus on scapular posture, scapular/rotator cuff strengthening, and anterior/posterior shoulder stretching.
Besides improving posture and increasing strength and range of motion, it might be important to prescribe exercises to optimize movement behavior in patients with chronic shoulder pain. Hodges and Tucker8 reported changes at multiple levels of the motor system in patients with chronic pain resulting in altered movement behavior with the objective to ‘‘protect’’ the tissues from further pain or injury, or threatened pain or injury. These long-lasting neuromuscular adaptations in response to pain may offer short-term benefit, but have potential long-term consequences due to factors such as increased load, decreased movement, and decreased variability and are advised to address in patients with chronic musculoskeletal pain.8–10 In the majority of clinical practice, patients are provided with explicit guidance for proper movement when retraining motor control. This guidance commonly pertains to coordinating the movements of the patient’s body, including instructions on scapular posture and muscle recruitment. A small alteration in the wording of instructions can result in a substantial influence on both performance and motor learning outcomes. When patients are directed to focus their attention on how their movements affect the environment—an external focus of attention—it leads to more effective and efficient movements.11,12 A movement pattern is considered more efficient or economical if the same movement outcome is achieved with less energy expended. In contrast, directing attention internally towards one’s own movements results in a more conscious form of control that limits the motor system and disrupts automatic control processes.13 The aim of implicit motor learning methods is to minimize the amount of explicit knowledge about movement execution and/or muscle recruitment during learning (internal focus), reduce the reliance on the working memory, and promote a more automatic control process.14
Implicit learning is an approach in which self-organization is key. The principle of self-organization emphasizes that coordinated movements emerge naturally from the interactions among the components of the motor system. Instead of being rigidly controlled from outside, the body adapts and organizes itself to achieve task goals while exploring different movement patterns. This concept highlights the importance of allowing learners to explore and discover their own movement solutions, promoting adaptability and skill development. In sports science, there is increasing evidence that implicit motor learning is superior to explicit learning when it comes to learning new skills and improving performance.15,16 There are a number of disciplines in which implicit learning has been successfully applied, including pediatric physiotherapy, gait training for stroke patients, and ACL rehabilitation, but implicit learning is rarely used in the context of shoulder rehabilitation.14,17,18
Considering the expected duration of rehabilitation within chronic shoulder pain patients, telerehabilitation seems a suitable medium for this population.19 During the COVID-19 pandemic physiotherapists widely used telerehabilitation to coach patients in their home exercise programs. In systematic reviews, both Seron et al. and Gava et al. concluded that telerehabilitation could be comparable to in-person rehabilitation to reduce pain and improve physical function in musculoskeletal conditions generally and shoulder pain specifically, but more high quality research is needed.20,21 The main advantage of telerehabilitation is that both the healthcare professional and the patient can carry out the treatment in their own environment without travel time or necessary transport.
The promising results of implicit motor learning in other conditions and the possibility of implicit learning to change motor control deficits evidenced in chronic pain conditions gave rise to this study. The aim of this study was to investigate the feasibility and clinical outcome of a new implicit motor learning exercise program in a group of patients with chronic shoulder pain.
MATERIALS AND METHODS
Study design
The feasibility study was a single group pre-post intervention design. The Institutional Review Board of Ghent University Hospital (B.U.N.: B6702020000611) approved the study.
Participants
Adults with chronic shoulder pain were recruited on social media and via flyers in public buildings and physiotherapy practices. Potential candidates were first screened through an online questionnaire to check whether they met inclusion criteria (questions on duration of shoulder pain, the experience of an unstable feeling in the shoulder, dislocations/subluxations, mobility restrictions of the shoulder, results of medical imaging, medical diagnosis). To be included patients had to have had shoulder pain for at least six months for which they consulted a medical doctor (MD). Participants were excluded if they were currently in therapy or had undergone shoulder surgery or sustained a shoulder fracture. Moreover, patients that were expected not to benefit the intervention were excluded namely patients with an unstable shoulder (shoulder dislocation/instability, labral lesion), capsular stiffness (frozen shoulder, severe osteoarthrosis) or with inflammatory nociceptive pain mechanisms (bursitis, calcific tendinopathy, rheumatic disorders), as diagnosed by the MD, were excluded. All participants signed an informed consent prior to participation.
Outcomes
Feasibility outcomes consisted of recruitment rate, follow up rate (% of participants who successfully completed the program and were reevaluated after six weeks), subjective reports regarding experience with the content of the program (custom-crafted statements on the content of this program scored with Likert scale eg. “I understood what was expected”, “I thought the exercises were easy to do”), self-reported adverse events, and self-reported adherence. Adherence was scored weekly as 0 (did not meet minimal exercise adherence of 15’, 3x/week) or 1 (meets minimal exercise adherence of 15’, 3x/week). A score of six out of six (100%) was defined as perfect adherence. Based on this outcome the feasibility of a future RCT and the need for protocol modification were assessed.
At baseline and after the six-week home exercise program patients were requested to complete an online questionnaire package that consisted of demographic variables and several patient reported outcome measures (PROMs). Pain and function were evaluated with the Shoulder Pain and Disability Index (SPADI)22 and Auto-Constant score.23 The SPADI was chosen due to excellent reported reliability (ICC≥0.90) in most studies, with reported minimal detectable change (MDC) of 18 points and minimal clinically important difference (MCID) between 8 and 13 points.24,25 The Auto-Constant score (patient self-report based) and the Constant score (clinician-based) have been shown to correlate well but no information on test-retest reliability of the Auto-Constant score is available.23,26 This alternative to the Constant score allows remote assessment which was necessary at the time of the study due to COVID precautions. Self-perceived active mobility and strength was measured with the Auto-Constant score. In this questionnaire patients have to select the pictures of a person lifting a weight or performing a specific movement that correspond with the level of lifting or moving they estimated themselves to be capable of.23 To assess patterns of fear-avoidance and endurance-related responses to pain the Avoidance Endurance Questionnaire (AEQ) was used.27 According to Hasenbring et al.,27 inactive, avoidant behavior would drive disuse-related muscle weakness, deconditioning, and metabolic changes in the musculoskeletal structures and the central nervous system, potentially leading to peripheral and central sensitization and increased pain perception. In contrast, in overactive behavior, inappropriate muscle forces might expose mainly passive structures (vertebral joints, ligaments, connective tissue) to increased stress and repetitive strain, causing microdamage, laxity, and inflammation. The AEQ was developed to assess emotional, cognitive, and behavioral fear-avoidance and endurance responses to pain, and has been validated and repeatedly applied in different chronic pain populations.27–29 This self report questionnaire consists of three parts (pain affective, cognitive and behavioural responses). More detailed information on the subscales of the AEQ can be found in Appendix 2.
Each item was scored on a 7 point-Likert scale (0: never, 1: almost never, 2: seldom, 3: sometimes, 4: often, 5: most of the time, and 6: always). Higher scores represent more thoughts that correspond with avoidance or endurance of pain. All subscales Chronbach’s alpha were in range from 0.76 to 0.91, which showed acceptable internal consistency.27 The participants were asked to fill out the questionnaire considering the pain they experienced in the past 14 days.
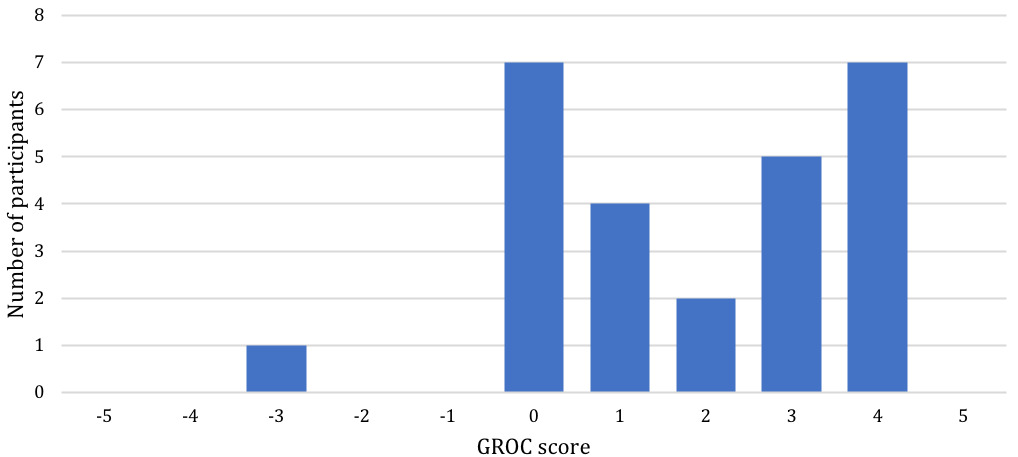
Overall satisfaction with the shoulder condition was evaluated before and after the 6-week program with the Patient Acceptable Symptom State (PASS).30 After the program patients were asked to score the rate of change between -5 and 5 (Global rating of change (GROC).31,32 A score of -5 corresponds with shoulder complaints being a lot worse than before the program, 0 with no change, and 5 with full recovery of shoulder complaints. A systematic review and meta-analysis on measurement properties concluded that GROC shows excellent test-retest reliability (ICC = 0.84) but as recall bias might influence validity it is advised to combine with other outcomes to track changes in symptoms.33
During weekly follow up, patients were asked to rate their pain at rest and at night on a numeric rating scale (NRS) as well as their ability to perform three important functional activities, using the Patient Specific Function Scale (PSFS).34,35 For NRS MCID was found to be 2.17 points in a population with shoulder pain.36 The PSFS shows moderate to good test-retest reliability (ICC 0.71) and MCID was shown to be 1.2 points.35 The advantage of the PSFS is that each patient can rate functional ability during daily life tasks that are relevant for them.
Intervention
For specific content reporting of the home based exercise program the Consensus on Exercise Reporting Template was followed.37 A general instruction video (https://youtu.be/s11NShRi35Y) and videos with exercise instructions (Appendix 1) were accessible online.
The program consisted of five exercises (Figure 1 and Appendix 1 detailed instructions). The exercise program was based on the principles of implicit motor learning.38
Self organization
To elicit unconscious automatic bottom-up organization of motor control of the upper extremities, overall balance was challenged during the exercises.38 Each exercise had ten levels of difficulty to maintain total body balance (Appendix 1). To determine the level at the start, the 70-30% rule was used. Participants were instructed to select the level at which they could execute the exercise approximately seven out of ten times without losing balance.
To encourage participants to expand their range of motor control possibilities and engage their shoulder muscles beyond their comfort zone, they were consistently prompted to reach their maximum extent during all exercises. While performing the exercise, individuals should exert additional effort to reach the target and fully utilize their shoulder mobility. To achieve this, subjects were directed to position themselves in a manner where the target was placed just beyond their normal reach.
External focus instructions
During all exercises the focus was on the target (sliding objects over the floor, reaching towards the wall, touching toes) and no instructions were provided on how to perform the exercise. To correct performance in case of discomfort or low back pain for example analogies were used to elicit the desired movement behavior implicitly throughout the program such as for example: “imagine your legs both in a cast as you perform the exercises, now imagine that your legs are out of the casts” or “imagine your legs stuck in concrete, now the concrete is broken and you are free again”.
Self-controlled learning and enhanced expectations
In the majority of rehabilitation scenarios, clinicians typically dictate the specifics of the training session. This includes decisions about the sequencing of tasks, the duration of practice, and when or whether instructions or demonstrations are provided. Consequently, patients often play a relatively passive role, with clinicians maintaining general control over most practice aspects. However, self-controlled learning, such as allowing patients to have some influence, requesting feedback, or selecting exercises, emerges as a potent instrument in the realm of motor learning. From a motivational perspective, patients were encouraged by the therapists (two last year master physiotherapy students that were specifically trained and under the supervision of two experienced senior shoulder physiotherapists) to take maximal responsibility in their training program and received the autonomy to make choices.13,39 During the six weeks participants were asked to practice with a minimum of three times a week. The therapists suggested that there may be superior outcome if the patients practiced more than three times per week. Duration of one exercise session was instructed to be 15 to 20 minutes but participants were allowed to perform shorter sessions multiple times a day. The sequence and duration of each exercise was not set. Participants could choose when and how much a specific exercise was done as long as a total of 15-20 minutes was reached. To control the pain (during and immediately after exercise, day to day, and week to week), participants were instructed to follow the pain monitoring model (Appendix 1).40,41 When pain increased or fatigue began, participants were instructed to switch to another exercise.
Follow-up with the participants was provided by the therapists during a weekly video or phone call according to individual preference. During these calls pain, PSFS, the level of difficulty achieved for each exercise (and whether this was challenging enough), adverse events, and the frequency and duration of training sessions were discussed.
Statistical analysis
Data were analyzed with SPSS statistical software (IBM SPSS Statistics, Version 27.0). Descriptive statistics were used to assess the feasibility outcomes. A Shapiro-Wilk test was combined with a histogram to check normal distribution. Paired sample t-tests and Wilcoxon signed-rank tests were used to compare SPADI, AEQ, Auto-Constant scores and NRS at rest, at night, and during patient specific activities (PSFS) pre to post. Differences in the PASS were analyzed with a McNemar test. Statistically significant differences were considered at p<0.05. Post hoc power analysis was conducted based on the SPADI.
RESULTS
A group of 28 participants (Mean age= 34.9 years ±13.59; male/female= 10/17) was recruited. Baseline characteristics are summarized in Table 2. Medical diagnoses of their shoulder pain differed among the group most of which were related to the rotator cuff (shoulder impingement, subacromial impingement, rotator cuff related shoulder pain, subacromial pain syndrome, rotator cuff tendinopathy, rotator cuff muscle “sprain”) however, some patients did not have clear medical diagnoses (such as “functional shoulder pain”). Twenty-six patients completed the study and two were lost to follow-up (one spontaneous improvement of pain before start of the study and one decided to consult an orthopedic surgeon for second opinion).
Feasibility outcome
-
Recruitment rate: A total of 16 weeks was required to screen 96 patients of which 28 patients met the inclusion criteria and were eligible for participation in this study.
-
Follow up rate: 92.9% of participants successfully completed follow up assessment after 6 weeks.
-
Subjective experience with the content of the program: The outcome of the questions regarding the personal experience of the exercise program is visualized in Figure 2. Majority of participants (66.6%) indicated their expectations regarding the exercise program were fulfilled. Therapist guidance, follow up and content of the exercise program received positive feedback from all participants. Moreover, 62.9% of participants felt the exercise program had positive effects on their shoulder pain.
-
Self-reported adverse events: Five patients reported adverse events during performance of exercises: low back pain (n=3), groin pain (n=1) and knee pain (n=1). All could be resolved by providing information on correct performance of the exercises or adapting the exercises. No patients reported adverse events after completion of the study.
-
Self-reported adherence: The mean adherence to the exercise program was 77.1 ± 29.41%. It can be observed in Figure 3 that the adherence was higher during the first two weeks, decreased after that, and increased again towards the end of the program.
Effect of the program on PROMs
An overview of the pre- and post-intervention scores for the PROMs and the corresponding p-values are presented in Table 1. Post hoc power analysis based on the SPADI resulted in a power of 0.94.
SPADI pain scores were significantly lower after six weeks of training (median difference [95%CI]= -14.0 [-22.0; -7.0]; p<0.001). SPADI function scores were significantly improved after the exercise program (median difference [95%CI]= -10.0 [-15.0; - 5.6]; p<0.001). Total SPADI scores improved significantly (mean difference [95%CI]= - 13.6 [-19.8;-7.4]; p<0.001).
In the Auto-Constant questionnaire, significant improvement was attained for pain, self-perceived strength, and ROM. The pain scores decreased significantly (median difference [95%CI]= -3.0 [-4.5; -1.5]; p<0.001), strength scores increased significantly (median difference [95%CI]= 2.5 [0.0; 5.0]; p=0.008) and ROM scores improved significantly (median difference [95%CI]= 2.0 [1.0; 3.5]; p=0.001). Activity scores did not change significantly (mean difference [95%CI]= 0.5 [-0.2; 1.2]; p=0.168) and the total Auto-Constant score was not significantly different after intervention (mean difference [95%CI]= 3.0 [-0.1; 6.1]; p= 0.060).
Before the program, 23.1% of the participants was satisfied with their shoulder condition, whereas after the study 69.3% were satisfied as measured with the PASS. This proportional change was significant (p<0.001).
The mean NRS pain score at rest improved significantly through the research (median difference [95%CI]= -0.5 [-1.5; 0.0]; p=0.033) as did the pain scores at night (median difference [95%CI]= -0.8 [-1.5; 0.0]; p= 0.029). For the PSFS the participants reported a significantly lower score reflecting improved ability to perform functional activities after the program (mean difference [95%CI]= -2.4 [-3.4;-1.5]; p<0.001).
Regarding the AEQ, the Pain Emotional Reactions score improved significantly after the intervention. The Anxiety Depression Scale (ADS) showed a significant mean difference [95%CI] of -0.6 [-0.8;-0.3] (p<0.001). Additionally, the Positive Mood Scale (PMS) significantly improved after training with a median difference [95%CI] of 0.5 [0.2; 1.0] (p=0.007). For the subscale Pain Cognitive Reactions, only the Help Hopelessness Scale (HHS) reached a significant difference (mean difference [95%CI]= -0.7 [-1.0;-0.3]; p= 0.002).
The self-perceived change in the condition of the shoulder after six weeks of exercising as measured with the GROC showed a mean change of 1.9 points (±1.89). The distribution of the scores are presented in Figure 4.
DISCUSSION
The aim of this research was to determine whether a novel home exercise program conducted via telerehabilitation based on implicit motor learning was effective for patients with chronic shoulder pain and whether the study protocol was feasible. The results showed that the study protocol was feasible in terms of follow up rate, exercise adherence, and adverse events. Statistically significant improvements were observed for the SPADI, NRS at rest and at night, and PASS after only six weeks training.
Twenty-six participants completed the six-week exercise program at home with weekly remote follow-up. The results showed that the study protocol was feasible with respect to follow-up rate and acceptable in terms of personal experience with the program, exercise adherence and adverse events. Majority of participants (66.6%) indicated their expectations regarding the exercise program to be fulfilled. Therapist guidance, follow up, and content of the exercise program received positive feedback from all participants. Moreover, 62.9% of participants felt the exercise program had positive effects on their shoulder pain. This is an important finding, since perception of participants about the exercise program is crucial for adherence to the treatment and thus successful rehabilitation.42,43 Although patient and therapist never met in person due to COVID-19 measures, participants indicated that they understood the instructions on the phone or video-calls, when combined with the YouTube videos.
Frequency of follow-up also appeared important in view of adverse events. Providing instructions on how to adapt the exercises was key in preventing pain in other joints such as low back and knee to persist. Hence, the communication used in this study appeared suitable for telerehabilitation.
The clinical outcome results are very promising after only six weeks of training. There was a 13.6 point decrease in the primary outcome (SPADI score). This result is higher than the MCID of 8-13 points but lower than the MDC of the SPADI of 18 points.24 The magnitude of this difference is comparable to other studies investigating the effect of more traditional exercise programs with strength and mobility exercises.44,45 Littlewood et al. for example showed improvement of SPADI scores after three months with 12.4 points in the self-managed group and 16.7 points in the usual physiotherapy group in patients with subacromial pain syndrome.45 Especially considering the study population (>6 months shoulder pain) a longer duration is recommended given that earlier research indicated longer lasting complaints may require a prolonged rehabilitation.46 The improvement in pain was significant for pain at rest and at night. The amount of change was smaller than the MCID of 2.17 points but comparable to changes seen in other intervention studies in this population.47,48 It is important to note that the small improvement might also be related to the rather low pain scores at baseline (1.8-1.9) which is most likely the result of exclusion of serious shoulder pathology such as frozen shoulder in the current study. A mean change in shoulder complaints of 1.9 points on the GROC represents that participants consider the change valuable regarding their health status.31
After the program it was shown that pain emotional reactions, as measured with the AEQ, significantly improved, meaning that patients had fewer depressive thoughts and anxiety and were in a better mood. This may relate to a happier lifestyle and thus a higher quality of life. In contrast, no significant changes were seen in participant’s coping reactions. Pain cognitive reactions also did not change significantly except for the HHS. The HHS represents the lack of hope and the feeling of impossibility to become pain-free.49 In other words, participants believed in the advantages of exercising and had a more optimistic point of view on the future after study completion. Combining the exercise program with behavioral change techniques could be an interesting direction for future research.
The current study attained a high percentage of compliance of 77%. Compared to other studies this adherence rate with home-based training was rather high. For example, Burns et al.43 reported an adherence of 41% with a home exercise program for patients with rotator cuff pathology. Possible reasons for this strong adherence might be the weekly follow-up calls, the dynamic nature of the exercises and the freedom of planning practice. Freedom of planning their own practice was perceived as an advantage by 96% of participants. Rehabilitation outcome strongly depends on treatment adherence. Interestingly, in this study it was observed that adherence decreased to the lowest value at week four and then started improving again towards the end of the program. A potential cause for the motivational dip could be that the novelty of the exercises was gone, and the end of the training period still seemed a long way off. NRS scores at rest and at night increased between week four and five probably causing the participants to see the benefit of the exercise program which in turn increased the adherence. After six weeks of training 70.4% of participants indicated they planned to continue to perform the exercises after study completion. The setup of this study with a home-based program and maximal responsibility for patients might be advantageous for patients’ self-efficacy, autonomy, and active coping behavior.
The training program only consisted of exercises based on implicit motor learning with external focus, no manual therapy or strength training was included. The underlying mechanism that could explain the clinical improvements might be related to motor learning resulting in more efficient and less rigid movement patterns. Studies investigating EMG muscle recruitment during a variety of exercises comparing external focus of attention to internal focus of attention showed lower muscle recruitment in the first.11,12,50–55 In these studies, where the executed movement remains constant and only the focus of attention is shifted, a decrease in muscle recruitment could indicate enhanced efficiency in performing the exercise. This could be beneficial during functional movements in daily activities. During follow up, some participants spontaneously reported that they noticed starting to use their affected shoulder more during daily activities and a significant improvement was found in their ability to perform individually reported activities as measured with the PSFS. A future study might include objective measurements of arm use in daily life. The placebo effect due to being included in a study and receiving attention from the therapist cannot be out ruled as there was no control group.
Limitations
A first limitation of this study is the lack of a control group. In addition to ruling out the influence of natural recovery, incorporating a control group would provide clarity on how the outcomes of this novel exercise program compare to a conventional function-based program. The latter typically includes a range of isolated shoulder strengthening and mobility exercises.
The second limitation is that no objective data on strength and mobility could be collected due to COVID measures at the time of the study. To evaluate exercise adherence objective data would also be desirable. Since the follow-up calls were not anonymous, socially desirable responses might unconsciously have been encouraged.
Finally, study duration can be considered a limitation. A future trial should have a longer training program of at least 12 weeks and include long term follow-up after six months up to one year.
CONCLUSION
The results of the current study provide promising results of a novel way designing shoulder exercises for patients with chronic shoulder pain. The home-based, six-week exercise program based on implicit motor learning produced significant improvements in pain and function in patients with chronic shoulder pain. The study protocol was feasible in terms of follow up rate, exercise adherence and adverse events. Participants especially appreciated the freedom to plan their exercise sessions and instructions and follow up provided by the therapists. Recruitment rate was rather low. Future studies should incorporate a control group, provide longer follow up, and include objective measurements to analyze changes in strength, range of motion, and use of the affected upper limb during daily life.
Conflict of interest
The authors declare that they have no conflict of interest.


_over_6_weeks_(100__equals_exercising_as_prescribed_at_least_3_.png)


_over_6_weeks_(100__equals_exercising_as_prescribed_at_least_3_.png)