INTRODUCTION
Chronic low back pain (LBP) is one of the most common reasons for healthcare visits, costing Americans over $100 billion annually.1–4 A systematic review by Meucci et al.5 reported the prevalence of chronic LBP in adults aged 18 years and older ranges from 3.9% to 20.3%. Multiple interventions are used to address impairments in range of motion, symptoms of pain, and perceptions of disability in individuals with LBP. These interventions include therapeutic exercise, manual therapy, patient education about lifestyle changes, pharmacological management, and modalities such as cryotherapy, heat, ultrasound, and electrical stimulation.6,7 Several interventions for LBP are acutely effective.8–10 The long-term effects of existing approaches are inconsistent, with over half of individuals with LBP experiencing a relapse of symptoms leading to costly surgeries or dependence on pain medication for symptom management.2,11,12 Therefore, more effective interventions are needed.
Recently, researchers have highlighted the potential benefit of therapies targeting the myofascial tissue in individuals with low back pain.13 One alternative intervention for acute and chronic back pain symptoms that targets the myofascial tissues is therapeutic dry cupping.14 Originating from traditional Chinese medicine, static dry cupping (SDC) is a passive technique where the cup is placed and left stationary on the body and is used to induce negative pressure in the underlying tissues.14,15 In Chinese medicine it is thought that SDC promotes the free flow of blood and the vital life force, qi, dispelling chronic pain and swelling.14 In Western medicine, many mechanisms of action have also been proposed for SDC, yet no clear explanation for observed clinical gains has been identified.15 Decreased pain following cupping may be a result of inhibitory pain modulation resulting in altered pain sensitivity, increased blood circulation, reduced inflammation, or immunomodulation.16 Locally, the negative pressure induced by SDC may separate layers of skin and fascia and affect fluid dynamics by stimulating the processes of proteoglycan, hyaluronic acid, and glycosaminoglycan production.17–19 This results in a more hydrophilic environment and altered biomechanical tissue properties such as tissue extensibility. Static dry cupping may also result in peripheral and central nervous system changes, including restoration of sensory processing. One potential example is the release of nerve growth factor (NGF) in the brain, which may improve proprioceptive feedback and motor patterning.14–16,18–21
Static cupping appears to have a therapeutic effect and is utilized for various musculoskeletal conditions,14 primarily to decrease pain. In a systematic review, Kim et al.22 reported the findings of two randomized control trials suggesting that cupping reduced pain in patients with LBP compared with usual care methods and analgesia. The results of a systematic review by Chao et al.23 suggest that cupping might have a short-term benefit in reducing pain for acute and chronic pain conditions. A recent systematic review by Mohamed et al.20 suggested low to moderate support for dry cupping to decrease LBP.
To date, few studies have investigated dynamic myofascial cupping. For the purposes of this manuscript dynamic myofascial cupping (DMC) is defined as cups being placed and left stationary on the body while the participant actively performs a movement. Most of the cupping literature involves static cup placement15,16,19,23 and little is known about what benefits, if any, are obtained by DMC. In persistent musculoskeletal disorders such as LBP, passive interventions that only address the area of symptoms may be inadequate. Chronic LBP disrupts sensory processing resulting in cortical reorganization and impaired touch perception,24,25 alters motor programming,26 and is associated with neuroplastic changes at multiple levels, resulting in central sensitization.25,27–30 Back pain is also commonly associated with reduction extensibility of muscle groups distal to the region of pain such as the hamstrings.31 Reduced hamstring extensibility in individuals with LBP may be due to altered local myofascial tissue characteristics as well as altered motor responses to sensory input during hamstring elongation.32,33 Reduced hamstring extensibility has been associated with adverse spinal alignment and motion in some individuals without LBP.34,35 Although conclusive data for a relationship between hamstring length and LBP are lacking,36 restriction in hamstring extensibility is often addressed clinically in individuals with LBP, particularly those with occupational or athletic activities that require large ranges of motion at the hip. Interventions involving active movements, such as dynamic cupping, may be required to reorganize or reset regional movement patterns and impairments such as reduced hamstring extensibility.
It is not known how combining SDC with DMC during active movement influences pain, perceived disability, and hamstring extensibility in those with LBP. The purpose of this case series was to explore changes in pain and function following local static and distal dynamic myofascial dry cupping treatments in patients with chronic low back pain.
CASE DESCRIPTIONS
The case series was conducted according to the guidelines of the Declaration of Helsinki,and was approved by a university Institutional Review Board. Informed consent was obtained from all individuals included in this case series. Participants were recruited from the general population via recruitment flyers posted within the general areas of a local hospital facility.
Criteria for inclusion were that participants were between the ages of l8-55 years. Participants were recruited if they had experienced constant LBP of at least 3/10 on the numeric pain rating scale (NPRS) for at least two weeks, or if they had experiences of recurring, but not necessarily constant, LBP of at least 3/10 for more than two months.31 Participants had to be cleared to participate in physical activity as determined by the Physical Activity Readiness Questionnaire (PAR-Q). The Physical Activity Readiness Questionnaire is used when a physician consult is not warranted and is commonly used as a safety screen for participation in research.37–40 Exclusion criteria included any current local or systemic infections, vascular disease including varicose veins, current use of NSAIDS or other analgesics, active cancer, history of lumbopelvic surgery, lumbar fracture, rheumatic disease, currently receiving treatment with corticosteroid, epidural steroid injection, or opioids, moderate to severe osteoporosis, and any previous medical intervention (e.g., physical therapy and chiropractic treatment) for the current episode of LBP. Each participant was screened for potential articular or joint limitations to knee and hip movement and range prior to the PSLR. There were no identified articular limitations noted for any of the three participants. Any potential limitations in the PSLR were due to tissue extensibility disorder, which often limits muscle length. This case series was prepared following the CARE Guidelines for case reports.41
Two female participants and one male participant with LBP were included in this case series. Participant demographics are presented in Table 1.
Outcome Measures
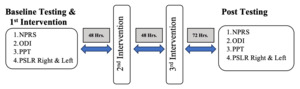
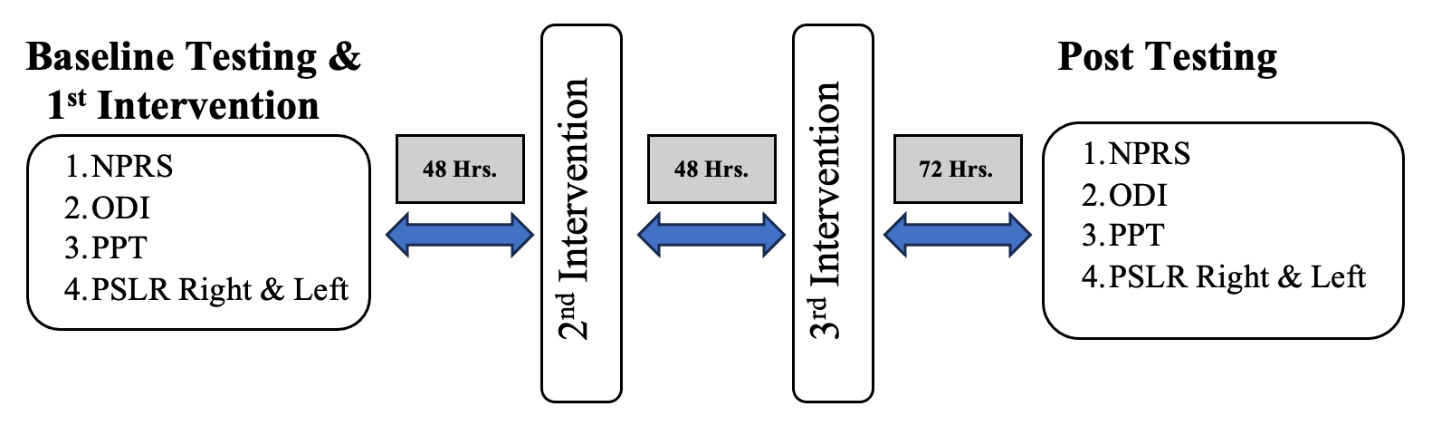
Participants attended three intervention visits, followed by one final data collection visit during which no intervention took place. Intervention visits were spaced 48 hours apart with the final data collection (e.g., post testing) visit occurring 72 hours after the third, and final, intervention (Figure 1). The outcomes were assessed at baseline and at the final post testing visit (Figure 1). The participants were instructed to avoid the use of any non-steroidal anti-inflammatory drugs, painkillers, or new activities throughout the duration of the study. The cupping interventions used in this case series included both SDC and DMC, where cups are placed stationary on a body region during an active movement exercise. A hypoallergenic oil-based lubricant (coconut oil) was used during both cupping interventions to maintain the adhesion of the cup to the participant’s skin. The researcher administering the interventions was the same individual each time with cup placement and amount of pressure determined by a single supervising licensed physical therapist with experience in cupping.
Subjective patient-based outcome measures included the Oswestry Disability Index (ODI), a perception of functional disability questionnaire for those with LBP, and the Numeric Pain Rating Scale (NPRS), used to assess current pain severity. The ODI is a valid and reliable outcome measure for spine-related functional disability.42,43 The NPRS appears to be the most accurate of the rating scales for pain severity.44 The NPRS was recorded before and after each of the three intervention sessions, and during the non-interventional post testing visit (Figure 1).
Changes in central nervous system function in response to cupping were assessed using pressure pain threshold. Pressure pain threshold (PPT) is a reliable method of measuring pain sensitivity45,46 in patients with myofascial and low back pain.47–50 Pressure pain threshold localized to the painful area was measured at four locations on the participant’s low back. Participants identified the most painful area to palpation within each quadrant of the low back (right and left, upper lumbar and lower lumbar region, Figure 2).50 In order to determine if cupping influenced pain sensitivity at an area remote to the location of the intervention and the symptoms, generalized PPT was measured at a standard location on the tibialis anterior muscle belly51 on the bilateral lower extremities. A pressure pain algometer (Force Dial ™ FDK/FDN Series Push Pull Force Gage, Wagner Instruments) was used to induce steadily increasing force at each location and the participant was asked to verbally identify as soon as the sensation of pressure turned to pain.52,53 Three measurements were taken at each location and the PPT was averaged. For the low back sites, the average PPT across the four sites was then calculated. In order to ensure the same painful area was re-tested, the identified areas were marked during baseline testing with a dot using a black ink permanent marker. Participants were instructed not to scrub off the marks, and marks were re-marked to prevent fading at each subsequent interventional visit to ensure the same location was re-tested.
Changes in tissue extensibility in the hamstrings were measured by the same investigator each time using the supine lower extremity passive straight leg raise range of motion test (PSLR ROM). The PSLR ROM was quantified on the bilateral lower extremities using a bubble inclinometer (Fabrication Enterprises, White Plains, NY). Inclinometers are a reliable and valid tool for ROM measurements with an ICC of ≥0.81.54–57
Intervention
Static dry cupping was administered with the participant in the prone position on a treatment table with pillows placed beneath their abdomen and lower extremities for patient comfort and to reduce spinal extension. The researcher applied the lubricant and four cups bilaterally on the patient’s low back, one at each of the four sites that they had previously identified as the most painful area in each quadrant of the low back (Figure 2). Standardized cup pressure was applied with a pump to create 1.5 cm of tissue displacement, with all cups having a 2.0-inch diameter (Acu-Point manufacturer, Marknew Products, Buena Park, CA). Once the four cups were applied, the participants were instructed to remain still in the prone position for 10 minutes, after which the cups and lubricant were removed (Figure 2).
Dynamic myofascial cupping was then applied to each lower extremity. Participants were placed in the sitting position, and cups were placed on the quadriceps muscle, antagonist to hamstring, during the active knee extension movement, where the hip is fixed in 900 flexed position, in an attempt to place emphasis on proximal hamstring extensibility. Four cups were positioned in a standardized rectangular pattern over the right and left quadriceps on the anterior mid-thigh by the same researcher at each intervention. The standardized cup placement pattern ensured the cups were placed on the quadriceps muscle and were individualized to the size of each participant. In general, the distal cups were three-to-four inches from the joint line and three-to-four inches apart while the proximal cups were seven-to-eight inches from the joint line and three-to-four inches apart. The participant performed ten repetitions of seated knee extension through the full available knee ROM on one lower extremity followed by ten repetitions on the other. The participant completed two sets of ten repetitions on each leg (Figure 3). After removal of the cups and lubricant, participants lay supine with the knees extended and feet placed on a bolster. The same researcher applied lubricant and four cups bilaterally in a standardized rectangular pattern over the hamstrings on the posterior mid-thigh. The participant performed two sets of ten repetitions of a supine active straight leg raise with each leg with 10-15 seconds of rest between sets (Figure 3). The standardized cup placement pattern ensured the cups were placed on the hamstring muscle and individualized to the size of each participant. In general, the distal cups were three-to-four inches from the joint line and three-to-four inches apart while the proximal cups were seven-to-eight inches from the joint line and three-to-four inches apart.
RESULTS
Participant demographics can be reviewed under Case Descriptions, Table 1. Outcomes were measured by the same researcher for all participants and all visits. Baseline and follow-up scores for ODI, PSLR, and NPRS are presented in Table 2. PPT measures at baseline and follow-up are described in Table 3.
All participants had improved scores post-intervention on the NPRS and ODI. After three treatment sessions, ODI scores improved by an average of 9.33% across the three participants (Figure 4A). At the post-intervention visit, all three participants reported complete pain resolution with 0/10 pain on the NPRS. All participants had increased PPT averaged across the four low back sites (Figure 4C) but not at the tibialis anterior sites (average of both limbs shown in Figure 4D). PSLR ROM on the left improved by an average of 17.3 degrees and an average of 9.3 degrees on the right (average of both limbs shown in Figure 4B).
DISCUSSION
This is the first case series reporting the effects of combining static dry cupping and dynamic cupping to different body regions using multiple subjective and objective assessment metrics. The intervention was safe and was tolerated well without any adverse effects. The intervention resulted in lower perceived disability, decreased pain and pain sensitivity and improved hamstring extensibility. The multiple clinical effects observed in this study may be due to the ability of cupping to decrease pain and inflammation, promote cutaneous blood flow and change biomechanical tissue properties, improve local anaerobic metabolism, and influence the immune system by modulating cellular mechanisms.15,16,20
Previous literature has suggested that a reduction of one point or 15.0% in NPRS scores indicates a minimal clinically important difference (MCID) in relation to chronic musculoskeletal pain58 while others state that a two point change is necessary for the changes to be meaningful.59 Results of a previous study identified meaningful NPRS change in sub-acute LBP to range between 3.5 and 4.7 points while those with chronic pain ranges from 2.5 to 4.5 points.60 In this study, all participants had reductions greater than these MCID values, averaging 6 points with a range of 5-7 points, indicating that cupping reduced pain severity. All three participants also demonstrated decreases in perceived disability, quantified by the ODI. These findings are similar to results found in previous literature that demonstrated improvements in ODI scores following treatment of the lower back.14,61 Copay et al.62 reported a minimum detectable change (MDC) of 10 percentage points for the ODI in lumbar spine surgery patients. One out of the three participants had a change in ODI score greater than 10 points, which suggests that this participant had meaningful improvements in perceived disability. However, the ODI might have a floor effect,63 preventing a meaningful difference to be identified in this group of participants.
Pressure pain threshold increased, or improved, in all participants, with an average increase in 11.0 psi (Table 3, Figure 4C). There is no consensus regarding clinically meaningful changes in PPT. However, it has been suggested than when the PPT changes are accompanied by a 2.5 point NPRS change in those with LBP, the PPT changes are considered meaningful.60 In this case series, the average pain decrease was 6 points, indicating the PPT changes after cupping may have been meaningful changes. These changes may be due to manipulation of the skin, subcutaneous fat, muscle, and fascial layers using cupping therapy thereby stimulating inhibition of nociceptive dorsal horn neurons in the spinal cord and brain.14,16 The decrease in perceived pain levels on the NPRS and pain sensitivity at the PPT locations may be related to inhibition of nociceptive receptors following cupping.
The improved hamstring extensibility post-intervention may be explained by restoration of normal fascial gliding. Impaired fascial gliding can lead to modifications in the composition of surrounding loose connective tissue and induced muscular stiffness, leading to dysfunctional movement patterns and reduced mobility.26,64,65 Cupping is theorized to restore normal fascial gliding by creating negative pressure, which increases lubrication, prevents collagen cross-binding, and restores hyaluronic acid viscosity.17,66 In addition, mechanical stress on the fascia increases the temperature of the tissue and reduces the viscosity of hyaluronic acid polymers to restore normal fascial gliding.67,68 In the hamstring musculature, the intent was to also to influence the mechanoreceptors for stretch (muscle spindles) and tension (Golgi tendon organs) to increase the hamstring’s ability to lengthen and to decrease coactivation during lengthening, thus influencing central neural control and increasing spatial range prior to contraction during movements which lengthen the muscle.33 Both of the dynamic myofascial cupping interventions used active contraction of the anterior lower extremity musculature to leverage reciprocal inhibition relaxation (RIR), where the contracting muscle is the antagonist to the muscle being treated. Performing the active exercises with the hamstring at different lengths appeared to improve hamstring extensibility, which may have been the result of improvements throughout the entire muscle length.32 Active knee extension with the hip in generally fixed flexed position intended to target the distal hamstring whereas hip active straight leg raise with motion with the knee in a generally fixed extended position intended to focus the intervention to the proximal hamstring.
The results of this case series must be interpreted with caution due to limitations in study design. A first limitation is the lack of standardization of the low back locations where the cups were placed on the subjects. This reduces the ability to compare findings between the subjects, but the subject-specific approach was consistent with clinical practice. A second potential limitation is the incorporation of multiple treatment methods. This study assessed two forms of cupping applied to sites in the painful area and sites non-local to the symptoms. We did not assess which method was more effective to reduce pain and functional disability. The chosen treatment approach was based on the concept of regional interdependence, which considers all regions of the body to be mechanically influenced by one another. This concept may explain how treatment of the anterior and posterior surfaces of the lower extremities may have affected lower back pain symptoms.69 A third limitation is the small sample size and strict exclusion criteria, which may limit the generalizability to other back pain populations, and the absence of a control group for comparison of treatment outcomes. Although hamstring extensibility, or length, was used as a metric of improvement and the protocol for cup placement was intentional for improving the length of the hamstring muscle, it was not an inclusion criterion and should be interpreted based on individual clinical presentations and within the context of positive changes within all four metrics. Since cups were placed on the low back as well as the hamstring, any improved hamstring length cannot be directly attributed to placement of the cups on either the hamstring or the low back. However, the combination of cup placements appeared to make positive changes in both the subjective and objective measures.
CONCLUSION
The results of this case series indicate positive outcomes of combining static and dynamic cupping on pain and muscle extensibility in three participants with LBP. These results should be interpreted with caution until future research involving randomized trials with rigorous methods and a control group are conducted to investigate the efficacy of combinations of static and dynamic cupping to treat musculoskeletal dysfunction and pain.
Competing interests
Authors state no conflict of interest.
Research funding
None declared.