INTRODUCTION
Approximately 250,000 anterior cruciate ligament (ACL) tears occur annually in the United States, with most tears arising from non-contact mechanisms.1,2 Anterior cruciate ligament reconstruction (ACLR) is considered a cost-effective treatment for such injuries in competitive athletes and the standard of care for those who wish to return to sport.3 Worldwide, ACLR appears to be growing for both adult and pediatric populations.4–7 Despite advancements in ACLR techniques, retear rates and return-to-play rates remain unsatisfactory in certain populations.8–10 The overall return to previous level of play is reported to be just below 65% for athletes.3 A recent study on female soccer athletes who underwent ACLR reported that 28% of all female soccer players and 34% of those players who returned to soccer experienced a second ACL tear. In another study on female soccer athletes, less than half returned to preinjury level of sport.9
Increased attention has been placed on residual post-operative rotary instability, which may correlate with increased failure rates, especially in young, highly active individuals.11,12 ACLRs have evolved significantly from one of the first ACL repair operations pioneered by Sir Arthur Mayo-Robson in 1895, and many techniques now exist.13 While most techniques focus on intra-articular graft reconstruction, high graft failure rates and persistent pivot shift have been seen in high-demand individuals.12,14 Persistent pivot shift and rotatory laxity have been shown to correlate with graft failure, lower clinical outcome scores, and increased reoperation rates.15 Such adverse outcomes are particularly pronounced in young patients participating in sports requiring regular pivoting, such as soccer, basketball, and football.16,17
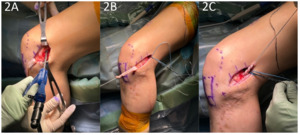
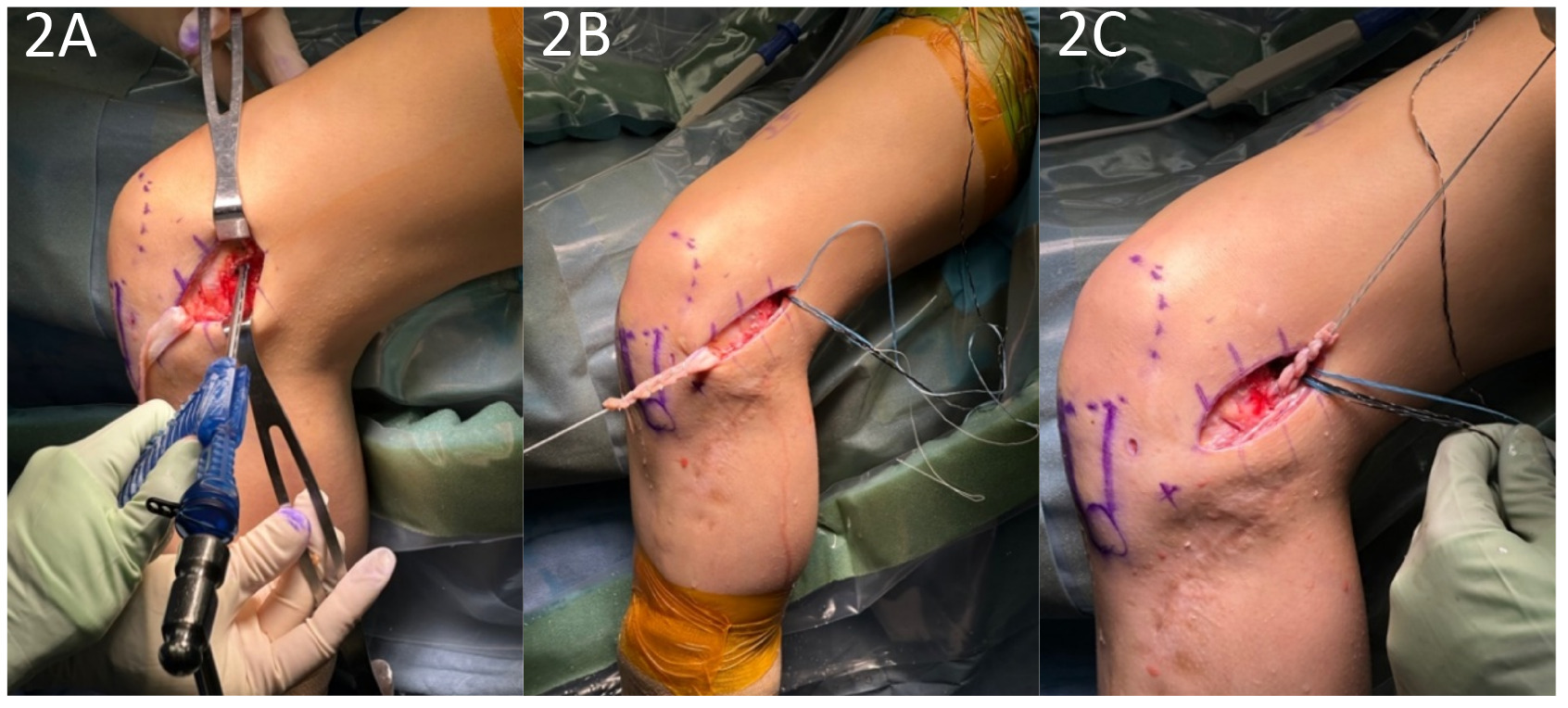
Recent investigations into the persistence of anterolateral rotatory laxity in these patients have led to an increased focus on the role of the anterolateral complex in modulating knee stability.18 Specifically, lateral extra-articular tenodesis (LET) has grown in popularity in the setting of ACLR. This procedure was initially utilized in ACL-deficient knees before the advent of intra-articular reconstruction techniques.19 One method by which to perform an LET is known as the Modified Lemaire Technique. This procedure entails a transfer of approximately an 8x1 cm graft of the iliotibial band (ITB) while leaving it anchored distally to Gerdy’s tubercle. The graft is released proximally from the vastus lateralis, passed under the lateral collateral ligament (LCL), and fixed to the femur just proximal and posterior to the lateral epicondyle (Figures 1-4).20
BIOMECHANICS OF LET
The biomechanical aims of performing a LET in conjunction with an ACLR are the restoration of normal knee kinematics, correcting a high-grade pivot shift, and correcting increased internal tibial rotation. There has been significant investigation into the biomechanical effects of the LET, with cadaveric studies generally supporting its use in conjunction with ACLR.21–23 Studies have shown reduced anterolateral residual laxity, ACL graft force, and anterior tibial translation (ATT).24,25 Further biomechanical studies have also investigated the utility of the LET + ACLR with a concurrent medial meniscectomy,26 showing reductions in ATT and internal rotation. These biomechanical studies suggest that a combined ACLR and LET may provide a protective effect on ACL graft and meniscus repair by increasing knee stability.
Despite such benefits, concerns have been raised regarding over-constraint and increased loading of the lateral compartment of the knee, although clinically, short to midterm studies have not shown increased osteoarthritis of the lateral compartment.27–29 Furthermore, there have been mixed results regarding the effect of LET on in-vivo mechanics.30,31 Nonetheless, a recent systematic review concluded that the LET procedure can resist internal rotation and improve residual knee rotatory laxity when performed in conjunction with ACLR.21
CLINICAL OUTCOMES
While the biomechanical results establish a foundation for the benefits of LET, recent clinical studies have provided further support for the use of LET. In the largest randomized clinical trial of LETs performed to date, 618 patients with a mean age of 18.9 years (range: 14-25) were randomized into ACLR vs. ACLR+LET groups. The addition of a LET to a hamstring autograft ACLR led to a statistically and clinically significant decrease in graft rupture rates from 11% to 4% and clinical failure rates (persistent asymmetric rotatory laxity and graft rupture) from 40% to 25%.32 The number to treat with LET to prevent one graft rupture was 14.
In another study, 49 consecutive patients aged 11 to 16 years old (mean 14.2 years) with a 98% participation rate in high-risk competitive sports demonstrated a graft re-rupture rate of 0% with a mean follow-up of 3.4 years and a return to sports rate of 100% following a quadriceps autograft ACLR with LET.33 Furthermore, another study of 66 pediatric patients between 12-16 years old showed patients who received a LET in addition to an ACLR had better KT-1000 arthrometer readings, better rotational stability measurements using kinematic rapid assessment (triaxial accelerometer), and lower graft rupture and cumulative failure rates than patients who underwent ACLR alone.34 In the revision setting, LET has been shown to improve International Knee Documentation Committee scores, restore rotational stability, and reduce failure rates compared with isolated ACLR.35
When considering operation morbidity, adding the LET does not appear to be a significant factor, as there were no clinically significant differences in motion or adverse events in a large-scale randomized trial.36
INDICATIONS
Significant risk factors for ACL re-tear include but are not limited to gender, age, sport, anatomic variation, hyperextension, and athletic level, all of which should be considered when deciding on the utility of a LET. The senior author of this paper (AMM) typically adds an LET for “high-risk” patients during ACLR. Common indications include female sex, soccer athletes, elite athletes, inherent ligamentous laxity, increased posterior tibial slope, high-grade pivot shift, revision ACL surgery, meniscal root tears/subtotal meniscectomies, and chronic ACL tears (Table 1).
In the revision setting, LET+ACLR has shown good return to sport rates in high-level basketball and soccer players.37 A study of 78 athletes in the Netherlands found a significant difference in RTS rates for revision ACL with LET (52%) compared to ACLR without LET (31%).38 Similar benefits have been seen for athletes competing at an elite (national or international) level. In a study of 455 elite athletes (83% male, mean age 22.5 years), 117 underwent ACLR + LET, and 338 underwent ACLR only. The cohort with ACLR only had a 9.5% retear rate, whereas the ACLR + LET group had a 3.4% retear rate. This reduction equated to ACLR + LET reducing graft failure by a factor of 2.8.39
REHABILITATION
One concern often raised regarding the addition of the LET is the effect on rehabilitation timelines. In the senior author’s practice, the LET does not change the rehabilitation protocol compared to a stand-alone ACLR. Furthermore, there is not increased rate of adverse events. The study by Heard et al. demonstrated that the ACLR + LET group had increased hardware irritation and increased pain at 3 months only. With regard to hardware irritation, many of the patients in that trial underwent LET fixation with a metal staple, which can be proud and irritating. Current techniques allow us to fix the LET with low-profile, knotless anchors.36
CONCLUSION
LET, when performed in conjunction with ACLR, has the potential to improve rotational stability, re-tear rates, and return to play for athletes. The procedure results in minimal morbidity and should be selectively used for higher risk patients. Further randomized studies are underway to better understand the indications for LET in patients with ACL injuries.