Introduction
Low back pain is a major global health problem, responsible for substantial disability with many cases progressing to a chronic state.1 Impairments in range of motion and movement are commonly associated with chronic low back pain (CLBP)-related functional tasks, such as forward bending from stance.2–9 Given that impairments in forward bending are associated with increased disability or pain, improving forward bending may play an indirect role in helping to alleviate the burden of CLBP.4,6,7,10–12 In particular, improving initial bending may be beneficial since this phase coincides with reversal of lumbar lordosis and the steepest rise in intradiscal pressure,13,14 a loading phase that may be provocative in some individuals with low back pain, even if not the sole cause of pain.15
Exercise, particularly strengthening, coordination or stabilization exercises, can improve pain, function and disability in CLBP populations.16–18 However, whether exercise improves forward bending is unclear.19–21 Individual responses to exercise vary and the mechanisms behind how certain people with CLBP improve with exercise are poorly understood.18,22,23
To enhance understanding, a biopsychosocial model is recommended.24 Under this model, the underlying mechanisms of response to exercise in individuals with CLBP are considered an interplay of biological, psychological and social factors.24 One important psychological factor to consider in people experiencing pain is pain self-efficacy.25–30 Pain self-efficacy is the belief that certain activities can be carried out despite pain.26 People with CLBP who demonstrated poorer pain self-efficacy also demonstrate greater disability.31,32 Aside from this association with poorer CLBP outcomes, lower (i.e., worse) pain self-efficacy has also been associated with altered lifting mechanics, including a stiffer trunk and reduced lumbar contribution.33 However, little is known about which phase of the forward-bend movement is most sensitive to these psychological influences. In particular, reversal of lumbar lordosis occurs within ~20-25 % of trunk flexion, marking the point of steepest rise in intradiscal pressure and posterior nucleus migration.13 This initial phase is also characterized by the slowest lumbar and hip angular velocities,9 which may prolong the period of increased disc loading in people with CLBP. Therefore, the first quarter of forward bending is a critical phase during which the susceptibility of lumbar and hip movements to influence from pain self-efficacy is unknown.
There are also other elements aside from pain self-efficacy that may impact lumbar and hip flexion range of motion during bending. Kinesiophobia, a psychological factor distinct from pain self-efficacy, measures the fear of being active and of moving due to the possibility of injury or exacerbating pain.26,31,34,35 Someone holding such beliefs may avoid or limit movement.34 The intensity of pain experienced in the lower back may also explain the degree of movement achieved.18,29 This subjective pain rating, along with kinesiophobia, are important to consider when investigating the relationship between pain self-efficacy and lumber and hip flexion range of motion.
Using secondary data derived from a recently published randomized controlled trial,36 the aim of this study was to investigate whether baseline pain self-efficacy influenced either lumbar or hip flexion range of motion (ROM) over the first quarter of forward bending post-exercise intervention. It was hypothesized that adults with lower baseline pain self-efficacy may respond better to exercise than those with higher baseline pain self-efficacy, demonstrated by increased lumbar flexion ROM and/or reduced hip flexion ROM during initial forward bending when assessed at 6 and 12-weeks.
Methods
Study Design and Setting
The design was a cohort study, utilizing data originally collected for a randomized-controlled trial (RCT) of two exercise interventions conducted at a single primary care physiotherapy clinic in Melbourne, Australia over approximately 21 months (between July 2018 and March 2020).36 The present study was approved by an institutional review board or similar committee (reference number 1749845). There was no patient or public involvement in the design, conduct, interpretation or translation of this study. New patients with CLBP presenting to the clinic were screened by a physiotherapist for eligibility into the study. Eligible participants (Table 1) gave informed consent to participate in the study then underwent baseline assessment followed by 12-weeks of global and isolated machine-based strengthening exercises with or without a neuromuscular control retraining exercise.36 In summary, all participants attended two 30-minute exercise sessions per week, supervised in a one-to-one setting by qualified physiotherapists.36 Data were collected again at 6 and 12-weeks post baseline assessment. The research question for the present cohort study was developed following the completion of data collection.
Participants
Participants with CLBP aged 18 to 65 years who were new patients of a physiotherapy clinic in Melbourne, Australia were recruited in this study. Participants were included if they presented with at least three months of low back pain and at least moderate disability (ie, 21% or higher) on the Oswestry Disability Index (ODI).37 Further details of inclusion and exclusion criteria are outlined in Table 1. A physiotherapist individually screened participants who presented to the clinic. Participants who met the eligibility criteria were presented with written information about the study, including its procedures. Those interested in participating provided written informed consent prior to randomization and the rights of participants were protected.
Variables
Exposure
The exposure (pain self-efficacy) was measured at baseline using the Pain Self-Efficacy Questionnaire (PSEQ), which comprises 10 questions and ranges in score from 0-60 points, where higher scores indicate stronger beliefs or more confidence in performing certain activities despite pain.25,26,35 A score of 41 or more on the PSEQ indicates minimal impairment, while a score of 31 to 40 indicates mild impairment, a score of 21 to 30 indicates moderate impairment and a score below 21 indicates severe impairment.34,38 The PSEQ, with a Minimal Clinically Important Difference of 9 or 11,39 has demonstrated responsiveness (minimal important change of 5.540) as well as high criterion validity (r>0.88) and reliability (ICC>0.70) in CLBP populations.35,38,40,41
Outcomes
The two biomechanical outcomes were i) lumbar flexion ROM and ii) hip flexion ROM over the first quarter of forward bending assessed at baseline, 6 and 12-weeks post-randomization. For kinematic analyses, participants were assessed barefoot while wearing shorts. Non-reflective markers were placed on the skin overlying specific vertebrae, as well as the head, pelvis, upper and lower limbs. Three-dimensional mapping of anatomical landmarks was performed using a 12-camera optoelectric motion analysis system (Optitrack Flex 13, NaturalPoint, Corvallis, OR, USA) sampling at 120 Hz.
Participants started the task standing upright with arms by their sides. Participants were given standardized instructions to bend down and lift an 8-kg object with both hands from the ground to the level of their abdomen using a self-selected technique. They then placed this object on their right side four times then on their left side four times. Bending (Figure 1) was conducted a maximum of eight times, the first and fifth (first time bending to lift the object to the other side) serving as practice.
The marker trajectories were labelled, cleaned and gap-filled using Optitrack Motive software (NaturalPoint, Corvallis, OR, USA). The joint angle data were filtered using a fourth order zero-phase shift low-pass Butterworth filter. Filtering is required to remove noise from kinematic data.42 A frequency of 6 Hz was used as a standard cut-off Butterworth filter frequency for joint angle.43 The marker trajectories were then passed to OpenSim (v4.0) software to calculate the lumbar and hip joint angles using the inverse kinematics tool.44 Joint angles were calculated using an XYZ Cardan rotation sequence corresponding to flexion/extension, abduction/adduction, and internal/external rotation. The hip joint center was estimated using the regression method described by Bell et al.,45 which uses pelvic marker positions to estimate joint center location and is widely applied in lower limb kinematic modelling. Time (from upright stance until the object on the floor was grasped: the forward bending phase of the lift) was standardized to 0%-100%. Lumbar and hip flexion ROM over the first quarter of forward bending was measured in degrees using Matlab (2020a) software. Negative flexion ROM indicated the individual extended their hip or lumbar spine. Mean lumbar flexion ROM and mean hip flexion ROM over the first quarter of forward bending from up to six lifts (excluding the two practice lifts) were used in the data analysis.
Potential Confounders
A causal diagram was developed prior to commencing analysis (Figure S1). The causal diagram made explicit the authors’ understanding of the current evidence for the important influences on pain self-efficacy and initial forward bending and identified potential confounding variables. As depression, anxiety and stress were unmeasured, the present study used data collected at baseline on the participant’s age (in years), sex (male or female), kinesiophobia, and pain intensity. Kinesiophobia was measured using the Tampa Scale for Kinesiophobia (TSK-17), which comprises 17 questions regarding pain-related fear beliefs about movement and re-injury.34,46 Scores range from 17 to 68 with higher scores indicating greater fear of movement. Pain intensity of the lower back over the past week was measured using the Visual Analogue Scale (VAS) with a range of 0 to 10.
Study Size
The present cohort study was a secondary analysis of data collected for a RCT,36 and, as such, the convenience sample of 69 participants was obtained due to COVID-19 restrictions preventing the continuation of the supervised exercise programs and data collection.
Statistical Methods
A descriptive table for pain self-efficacy (the exposure), lumbar and hip flexion ROM (the outcomes), and age, sex, pain intensity and kinesiophobia (the potential confounders) was generated for the total cohort with participants grouped by whether they completed only the baseline assessment, the baseline and 6-week assessment, or all three assessments to explore whether there was differential loss to follow-up.
Multivariable linear mixed-effects models were fitted per outcome with an interaction term between baseline pain self-efficacy and time, and adjustment for the confounders age, sex, and baseline kinesiophobia and pain intensity (identified as the confounder set in the causal diagram, Figure S1). These models were fitted using restricted maximum likelihood with an unstructured residual covariance, and all available outcome observations were analyzed (i.e., an available case analysis) where missing outcome data were assumed to be missing at random.47 Scatter plots at each timepoint with LOWESS (locally weighted scatterplot smoothing) curves were used to check the model assumption of linearity between the outcomes and baseline pain self-efficacy and continuous potential confounders, age, baseline kinesiophobia and pain intensity.
Sensitivity analyses of the model results for each outcome were conducted with potential outliers (residuals (≥3 standard deviations [SD]) removed. The model for each outcome was also refitted using all the individual observations from each of up to 6 lifts per participant as the outcome (instead of the average from up to six lifts) by nesting the individual observations within each participant. All statistical analyses were performed using Stata Version 15 (StataCorp, College Station, TX, USA).
Results
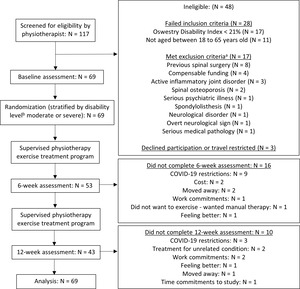
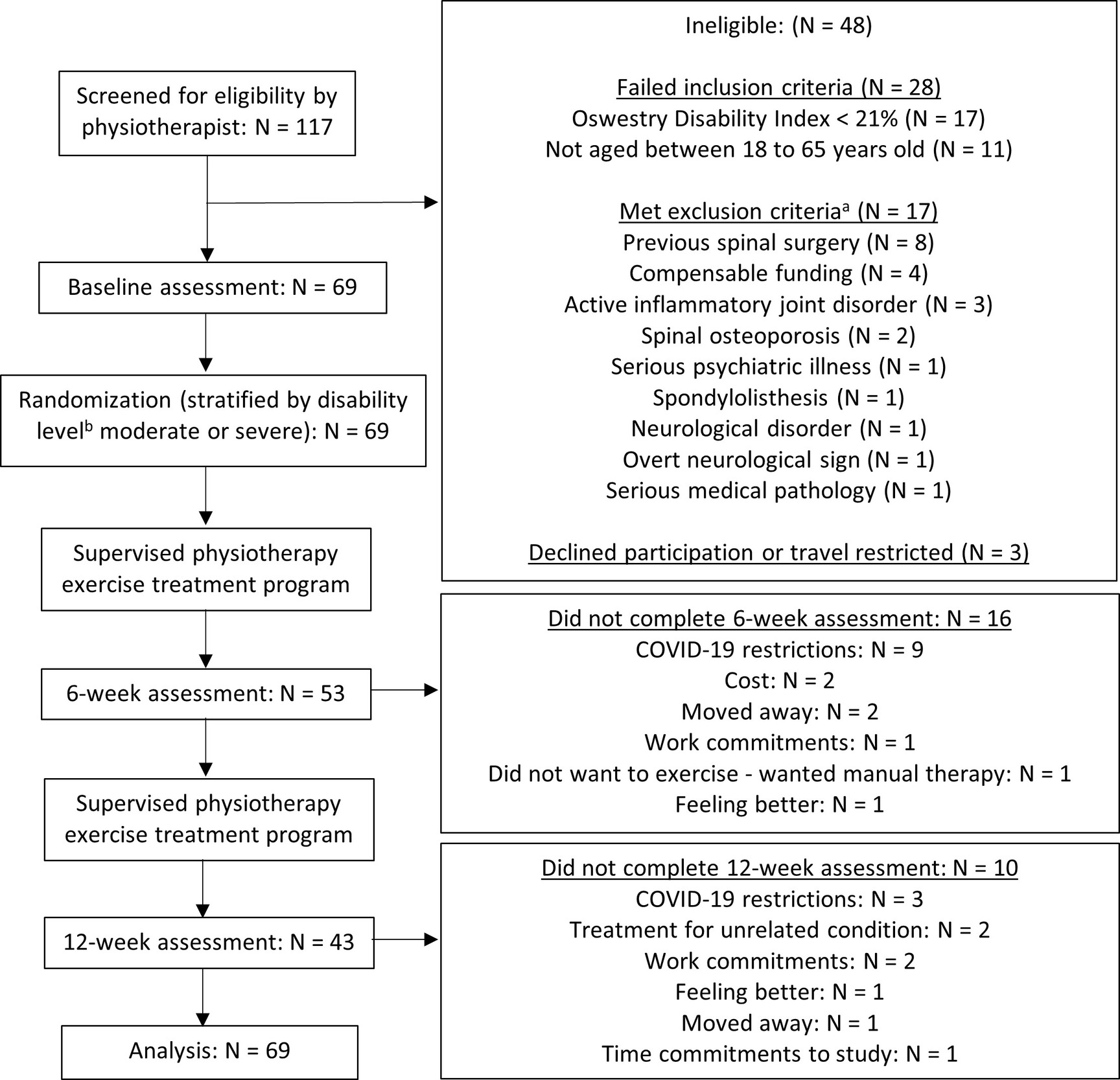
Sixty-nine participants completed the assessments and their data were analyzed. Figure 2 shows the number of individuals at each stage of the study and the reasons for non-participation. The primary reason for ineligibility was a score of ‘minimal disability’ (less than 21%) on the ODI. While 69 participants completed baseline assessment, 53 completed the baseline and the 6-week assessment, and 43 completed assessments at all three timepoints. Of the 26 participants who did not complete the 12-week assessment (38% of the total sample), 16 (23% of the total sample) also did not complete the 6-week assessment. The primary reason for non-participation was due to COVID-19 restrictions (N = 12).
At baseline, all 69 participants recorded measures of pain self-efficacy, age, sex, pain intensity, kinesiophobia and initial bending outcomes for six lifts except for one participant with recorded outcomes for five lifts and one participant with recorded outcomes for two lifts. Of the 53 participants who completed the 6-week assessment, all participants recorded outcomes for six lifts except for three participants with recorded outcomes for five lifts each. All 43 participants who completed the 12-week assessment recorded outcomes for six lifts.
Table 2 indicates that some characteristics and summary measures of study participants differed according to which assessments were completed. In particular, the 16 participants who only completed the baseline assessment were more likely to be male (75% vs 49%) and flexed at the hip (11.9° vs 8.8°) slightly more at baseline than those 43 who completed all three assessments. The 10 participants who completed only the baseline and 6-week assessments flexed at the lumbar spine (8.5° vs 5.9°) and hip (11.2° vs 8.8°) more at baseline than participants who completed all three assessments.
At baseline, 45 out of 69 participants (65.2% of the sample) were classified as minimally impaired in pain self-efficacy (a PSEQ score greater than 40). There was a similar proportion of participants with minimal impairment in baseline pain self-efficacy remaining at six weeks (66.0% or 35 out of 53 participants) and 12 weeks (67.4% or 29 out of 43 participants). No participants recorded PSEQ scores in the severe impairment band (a score less than 21).
Table 3 shows the estimated mean change in each outcome at each timepoint with a 10-point increase in baseline PSEQ score, adjusted for age, sex, and baseline kinesiophobia and pain intensity. A 10-point change in baseline PSEQ was chosen because the standard deviation (SD) of the PSEQ measure in this study was 9.96 and the minimal important change in PSEQ has been reported as nine.35 At baseline, there was an estimated mean decrease of 1.47 degrees (95% CI: -2.68, -0.27) in lumbar flexion ROM and 1.74 degrees (95% CI: -3.68, 0.21) in hip flexion ROM over the first quarter of forward bending per 10-point increase in baseline pain self-efficacy, adjusted for age, sex, and baseline kinesiophobia and pain intensity. At 6- and 12-weeks, there were, respectively, estimated mean decreases of 0.51 (95%CI: -1.41, 0.39) and 0.94 degrees (95%CI: -1.75, -0.13) in lumbar and 1.64 (95%CI: -3.70, 0.41) and 1.43 degrees (95%CI: -3.34, 0.48) in hip flexion ROM over the first quarter of forward bending per 10-point increase in baseline pain self-efficacy, adjusted for age, sex, and baseline kinesiophobia and pain intensity.
Figure 3 shows that the association between baseline pain self-efficacy and each outcome did not change substantially over time, and this was confirmed with the interaction terms for baseline pain self-efficacy and follow-up time (interaction p-values ranged from 0.086 to 0.931).
The main analysis was robust to removal of outliers (observations more than 3 SD from the mean residual) and to using the individual lift scores instead of an average of up to six lifts per participant (Table S1 and Table S2, respectively).
Discussion
Key Results
Adults with CLBP often demonstrate altered forward bending mechanics, yet it remains unclear why some individuals show greater changes in movement patterns following exercise interventions than others. Pain self-efficacy has been linked to disability and lifting strategies in CLBP populations and may be one factor influencing this variability. Understanding whether baseline pain self-efficacy influences changes in lumbar and hip movement during forward bending could inform personalized rehabilitation strategies. Therefore, the aim of the present study was to determine whether baseline pain self-efficacy was associated with lumbar and/or hip flexion ROM in the initial phase of forward bending following a 12-week exercise program. The present study found no evidence that baseline pain self-efficacy influenced lumbar flexion ROM or hip flexion ROM during initial forward bending post-exercise in adults with CLBP. This is the first study that has investigated the potential influence of baseline pain self-efficacy on this movement post-exercise intervention. The present study also found that, at baseline, participants with higher pain self-efficacy flexed their lumbar spine less than those with lower pain self-efficacy during initial forward bending. The difference, however, was less than 2 degrees for every 10-point change in pain self-efficacy, which may be clinically negligible. This initial phase of forward bending in people with CLBP was of interest as it may be associated with pain provocation given lumbar disc degeneration.15 In a degenerated lumbar disc, intra-discal pressure is not uniform and often accompanied by annular fissuring and ingrowth of nerve endings into the nucleus.15 Movement of the nucleus during initial lumbar flexion may compress these nerve endings, resulting in irritation and pain.15 A strategy to minimize the risk of pain provocation during the initial stage of bending movement could be to flex less through the lumbar spine and/or more through the hip (i.e., lower lumbar-hip ratio).15 This is consistent with previous research identifying that, during forward bending, those with CLBP flexed their lumbar spine less or their hips more than those without CLBP.4,8 While prior studies have analyzed either total range of motion4 or later quartiles,8 the present study extends this work by examining the initial quartile of motion, when mechanical loading on spinal structures rises most steeply. However, whilst we hypothesized that pain self-efficacy may influence the adoption of a movement strategy post exercise intervention similar to those without CLBP, the current findings failed to support this notion.
Higher levels of pain self-efficacy, which indicate greater confidence in one’s ability to perform activities despite experiencing pain, are associated with better outcomes in terms of pain management, disability reduction, and functional ability.29,33,48 Previous research suggests CLBP sufferers with lower pain self-efficacy lift light loads (of approximately 10% body weight) using a different technique (i.e., stiffer back, knees more bent) compared to those with higher pain self-efficacy.33 This is somewhat in contrast to the current results of higher pain self-efficacy being associated with less lumbar spine flexion during initial bending. Lifting a light load with an extended lumbar spine could be detrimental to spinal health as this posture is associated with a higher amount of loading.49 Consequently, investigating how pain self-efficacy influences bending and lifting kinematics following interventions such as exercise is important.
Changes of lumbopelvic movement coordination are thought likely to be a result of specific motor control training of the lumbopelvic region.50 Tsang et al.50 (2021) reported changes in lumbar spine and hip angular velocity during repeated forward bending movement following a 6-week training program. The participants in this study also reported improvement in pain self-efficacy (assessed using the PSEQ) following the program. Tsang et al. examined deep abdominal (transversus abdominis) muscle activation, while the present study concentrated on isolated lumbar extensor muscle strengthening using a lumbar extensor dynamometer with pelvic stabilisation.51 Additionally, Tsang et al.50 progressed their exercises from activating deep muscles to performing controlled movements of the lumbopelvic area. In contrast, the exercise progression in the present study involved increasing resistance to the same movement. The lack of targeted training may explain why the results of the present study did not show associated changes in lumbopelvic motor control.
A strength of the present study was the utilization of longitudinal data from the robustly designed prior RCT. The causal diagram also made explicit the investigator’s evidence-based assumptions of what influences pain self-efficacy and initial forward bending post-exercise in this CLBP population and identified potential confounding variables that were adjusted for in the analyses.
Limitations
As a secondary analysis of data originally collected as part of an RCT investigating the effect of two exercise interventions on disability, the (general strengthening) exercises were not targeted to improve initial forward bending. Hence, a lack of change in this movement, regardless of pain self-efficacy score, may explain the null result.2,8,22,28,48,52 As most participants were minimally impaired in pain self-efficacy, and no one severely impaired, the generalizability of the results are also reduced. The present study sampled participants seeking treatment, which may explain why most had high pain self-efficacy. Though the hypothesis related specifically to the initial 25% of the forward bending movement (as this is where it was theorized a change in response to exercise may occur),15 the biomechanics of lifting may not be adequately reflected in lumbar and hip kinematic data in the initial 25% of forward bending alone and may need to be combined with knee and ankle kinematic data, data on the remaining 75% of the forward bending motion or kinetic data. It is a limitation of the present study, however, that this other data was not analyzed. Additionally, the magnitude of change that was observed (<2° for both lumbar and hip flexion) is smaller than the typical measurement error reported for marker-based optical motion capture of the spine and hip. Specifically, typical soft tissue artifact-related angular errors (5-10° lumbar; 6-8° hip) and published minimal detectable change values (≥ 6-15°) exceed the <2° changes observed in the current study, indicating these differences may lie within measurement noise.53–55 Hence, the small angular differences detected in this study should be interpreted with caution, as they may fall within the error of the measurement system. Finally, there was substantial missing outcome data, largely due to COVID-19 restrictions, with indications of differential loss to follow-up. Consequently, the results may be biased since mixed-effects modelling assumes data are missing at random, after controlling for the measured confounders.
Interpretation
Given these limitations, a lack of evidence that pain self-efficacy influences initial forward bending post-exercise is not conclusive. Further studies are needed to corroborate these findings. Such studies may consider analyzing other lifting-related kinematic and kinetic data. These studies may also consider alternate methods of recruitment aside from sampling only those seeking treatment. Targeting exercise to improve certain kinematic and kinetic outcomes, such as by training lifting techniques for tasks such as lifting groceries, would also maximize the chance of detecting an effect of pain self-efficacy on these outcomes, if one existed.
CONCLUSION
In the present study, baseline pain self-efficacy did not influence initial forward bending at 6- and 12-weeks following exercise but was associated with less lumbar flexion during initial bending at baseline. Further research on other modifiable variables that may affect exercise outcomes is required.
Disclosure of interest
The authors report there are no competing interests to declare.
Corresponding Author:
Fiona McManus
Centre for Epidemiology and Biostatistics
Level 3, 207 Bouverie Street
The University of Melbourne, Parkville, Victoria 3010
Australia
Phone: +61 3 8344 0637
Fax: +61 3 9349 5815
Email: fmcmanus@unimelb.edu.au
Acknowledgements
The authors would like to acknowledge the research team involved in the original Randomized Controlled Trial (RCT) (Dr. Joshua Brodie Farragher, A/Professor Adam Bryant, Dr Adrian Pranata, Professor Gavin Williams, Professor Doa El-Ansary, A/Professor Selina Parry and Professor Jessica Kasza), Dr Kathleen Leach, for her assistance with developing the causal diagram and the patients and staff at Kieser Brighton for their involvement in the original RCT.

_in_each_outcome_at_baseline__6-weeks_.png)

_in_each_outcome_at_baseline__6-weeks_.png)